Pancreatic surgery has evolved since Whipple's description of the pancreaticoduodenectomy.1 In recent years, great efforts have been made to perform more conservative techniques in order to reduce postoperative morbidity. For benign diseases, various groups have described techniques to try to preserve healthy pancreatic tissue. Beger et al.2 published a series of 128 patients who underwent pancreatic resection with duodenum preservation and satisfactory postoperative outcomes, concluding that conservative pancreatic surgery was feasible. Martínez-Castro et al.3 analysed duodenum preserving as a conservative form of head of pancreas resection in four patients with chronic pancreatitis, with no postoperative mortality, preserving good endocrine and exocrine function in the short and long term. Busquets et al. also performed duodenal preservation in a group of 20 patients. None had disease recurrence over the course of follow-up for the resected tumours.4 Therefore, we can see that conservative surgery of the pancreaticoduodenal region has become well established in processes such as chronic pancreatitis, and some groups have even begun to use these techniques to treat benign tumours, and even tumours of uncertain malignant potential.
Various different conservative techniques have been described, including duodenum-preserving partial head of pancreas resection according to the Beger et al.2 technique, or duodenum-preserving partial resection of the upper portion of the pancreatic head combined with total resection of the lower portion of the pancreatic head according to the Pedrazzoli et al. technique.5 Several variants and modifications to this technique have since been developed, such as that used by authors Frey and Smith, combining with longitudinal bypass of the pancreatic duct,6 or the technique used by Gloor et al.7
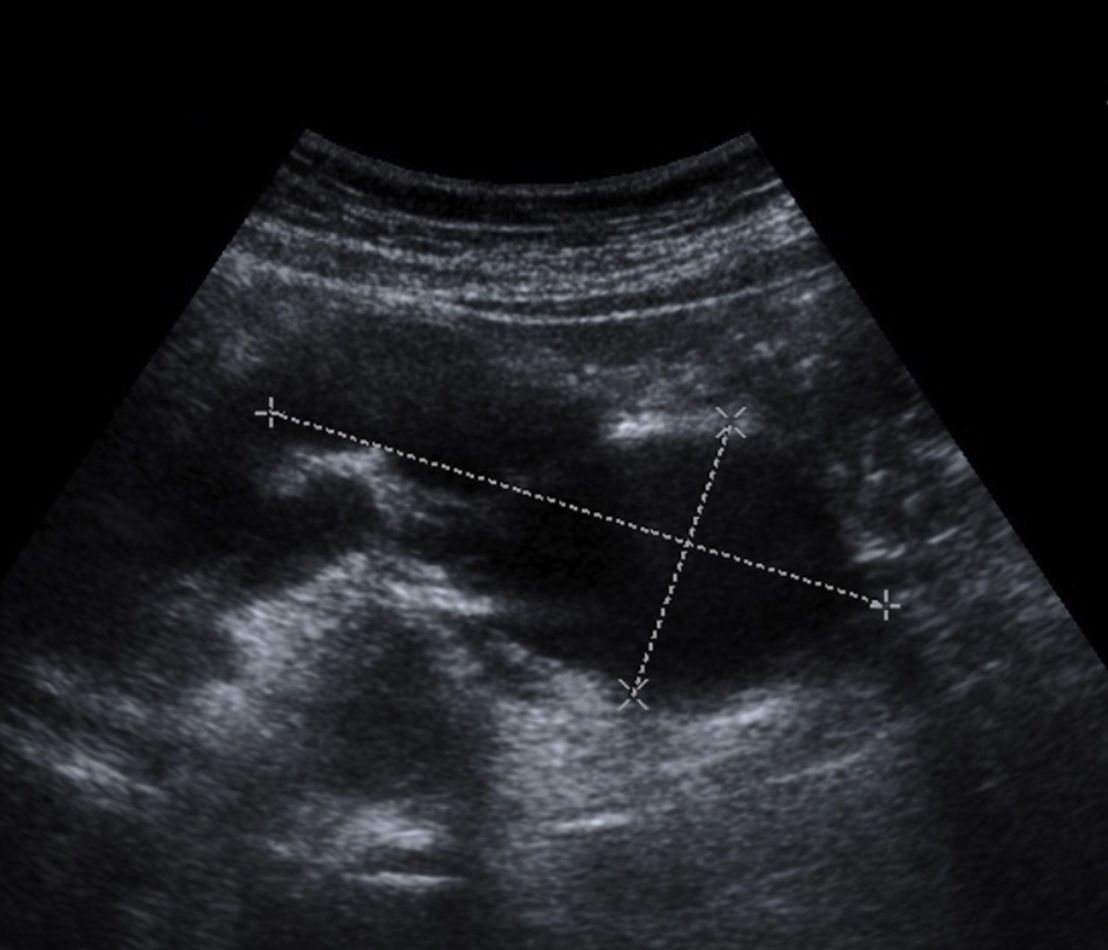
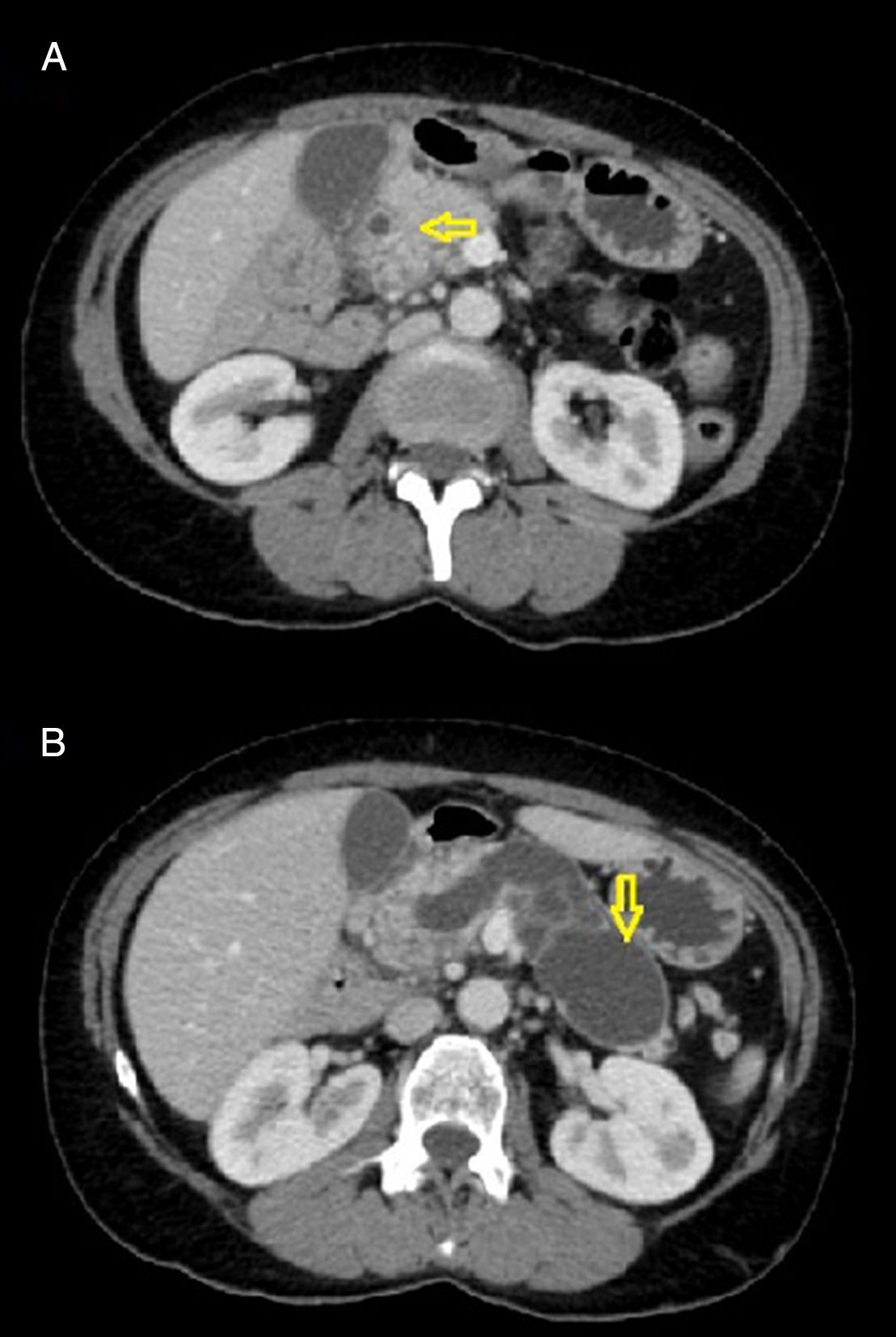
In the case report we present here, a duodenum-preserving pancreatectomy was performed in a case of intraductal papillary mucinous neoplasms (IPMN). This was a 54-year-old woman who consulted for abdominal pain with suspected biliary colic. An abdominal ultrasound showed a multicystic image in the tail of the pancreas (Fig. 1). In view of these findings, it was decided to complete the study with a computed tomography (CT) scan, which showed a lobulated-septated cystic lesion, with an approximate size of 8cm×3.5cm, possibly related to a cystic tumour of the pancreas, showing continuity with the main pancreatic duct, which was dilated (Fig. 2A and B). Given these findings, the patient underwent a duodenum-preserving subtotal pancreatectomy with preservation of part of the pancreatic head adjacent to the papilla. The pathology report was of an intracystic papillary mucinous neoplasm with moderate epithelial dysplasia, with no signs of cancer cell invasion in the resection margin. The patient made good postoperative progress. She needed insulin adjustment for adequate blood glucose control and was discharged on day seven post-intervention. Now, three months after surgery, the patient is asymptomatic, with good blood glucose control and she is free of disease.
IPMN has aroused great interest in recent years due to a progressive increase in frequency and also because of the variation in the way it presents clinically and pathologically.8 These neoplasms can originate in the main duct or in any of its branches, and they have recently been divided into categories according to whether there is mild, moderate or severe dysplasia or cancer cell invasion.9 Patients most commonly present with abdominal pain (49–82%), acute pancreatitis (13–64%) and weight loss (29–50%). Other clinical abnormalities include the onset of diabetes mellitus (11–72%), jaundice (9–18%) and exocrine insufficiency (7–17%).10 In our case, the first symptom was colicky abdominal pain.
The standard surgical technique for the treatment of IPMN is pancreaticoduodenectomy, particularly for patients with invasive IPMN. However, duodenum-preserving partial pancreatic resection seems to be a safe and highly effective procedure in the treatment of patients with branch-duct-type IPMN localised in the head of the pancreas. Fernández-Cruz et al. analysed a group of patients with IPMN and concluded that in patients with the branch-duct type it is possible to perform duodenum-preserving conservative surgery, obtaining good results with minimal morbidity.8 In our case, the intraoperative biopsy enabled us to rule out malignancy in the resection margins, which allowed us to preserve the duodenum with part of the head of pancreas that was not affected by the cystic lesion, thus avoiding having to perform a standard pancreaticoduodenectomy.
In light of this case report, we believe that in future studies a more in-depth analysis is required of the improvement in quality of life and the physiological repercussions according to the technique used. The technical complexity of this type of intervention may be greater than that of a conventional technique such as pancreaticoduodenectomy, and there may be more complications. The indications are therefore still under debate, but in selected cases it could be a good option for preserving healthy and functioning pancreatic tissue.
Please cite this article as: García-Santos EP, Padilla-Valverde D, Villarejo-Campos P, Sánchez-García S, Puerto-Puerto A, Martín-Fernández J. Pancreatectomía con preservación duodenal en un caso de neoplasia mucinosa papilar intraductal. Gastroenterol Hepatol. 2018;41:306–307.