We present the case of a 37-year-old woman with a history of T2N1M0 invasive ductal carcinoma of the left breast diagnosed 18 months earlier. After diagnosis, surgical resection was performed, but turned out to be incomplete, and the patient was started on chemoradiotherapy. She had no other relevant medical or surgical history. A repeat breast ultrasound was performed after she found a lump in her right breast (contralateral to that of the initial tumour) on self-examination. The test ruled out involvement of the right breast but incidentally detected left axillary lymphadenopathy, for which an ultrasound-guided fine-needle aspiration biopsy was performed. Cytology was positive for malignancy and compatible with ductal carcinoma. In view of the recurrence of the patient's disease, we performed a positron emission tomography (PET) scan, which showed uptake in the stomach, meaning a gastroscopy was required.
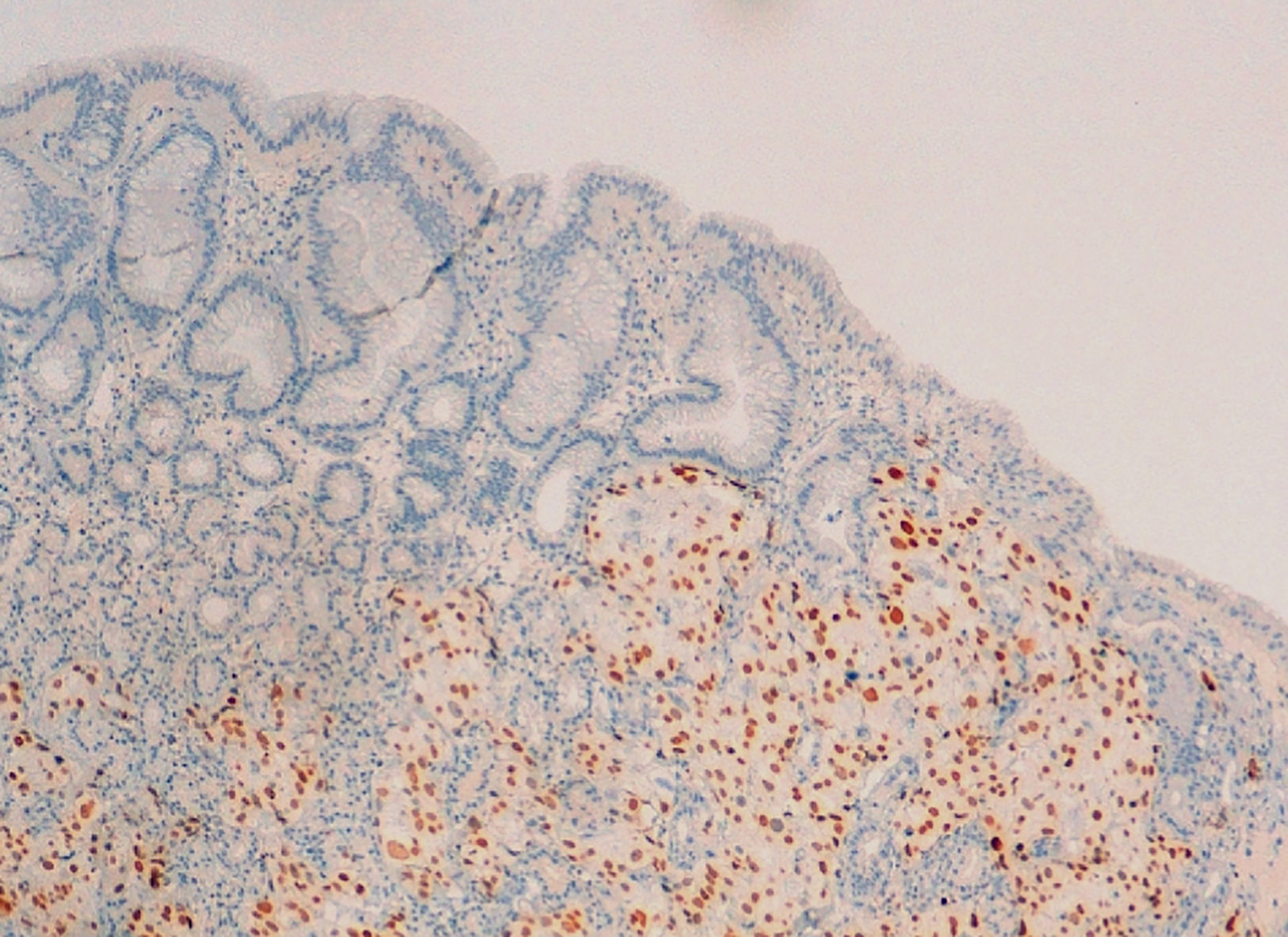
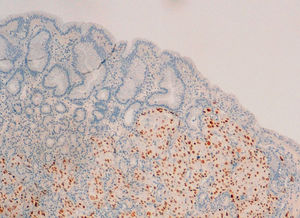
Endoscopically, several superficially ulcerated lesions measuring 3–5mm in diameter, with the appearance of being submucosal, were seen in the fundus and gastric bodies (Fig. 1). Biopsies were taken from the lesions and sent to the pathology department for histological study. After haematoxylin–eosin staining, neoplastic invasion was observed with loss of normal glandular architecture. Immunohistochemistry (GATA-3) confirmed the breast origin of the metastases (Fig. 2).
The patient died four months after having the gastroscopy, despite the chemoradiotherapy, from cancer-related complications.
Although relatively rare, metastatic spread of breast cancer to the gastrointestinal tract does happen.1–4 Ductal breast cancer is normally associated with liver, lung and brain metastases.1,5,6 Gynaecological, retroperitoneal and, less frequently, gastrointestinal metastases are more typical of lobular breast cancer1,4–7 and very uncommon in ductal cancer.7 Even in cases of mixed histology, it is the lobular component that tends to metastasise to the gastrointestinal tract,1 and the stomach is the region most commonly affected.1–4,6,7 Published series report an incidence of gastric metastasis from 4% to 18% after performing post-mortem examinations on patients diagnosed with breast cancer.6,7 We need to be aware, moreover, that after malignant melanoma, breast cancer is the second leading cause of gastric metastasis.6–9 Gastric involvement tends to occur in the form of linitis plastica resulting from metastatic infiltration.1–4,6 Other less common forms of presentation include nodular, polypoid, and ulcerated lesions.1–3,7,9
Endoscopy is the best method to assess gastrointestinal tract involvement.1–4,8,9 Endoscopic assessment is mandatory in patients with a history of breast cancer and gastrointestinal symptoms, even if their cancer was more than 30 years ago.1,2,7,8 Gastric involvement caused by breast metastasis has also been described in patients with no history of cancer or known breast cancer at the time of diagnosis.6 There are no specific gastrointestinal symptoms and the clinical signs can even be confused with the side effects of the cancer treatment or with other gastrointestinal disorders.1,4,7–9 In cases presenting for the first time with this type of metastasis, such misinterpretation may delay definitive diagnosis and treatment.1,9 Endoscopic ultrasound enables us to visualise the depth of the lesion and locate the best area for taking biopsies.1–4 Immunohistochemical study of gastric biopsies is essential for histological diagnosis.4,6–8 Differentiating between primary gastric cancer and gastric metastases is essential in order to determine the most appropriate treatment plan.4,6–8 The increase in the life expectancy of patients with breast cancer could lead to an increase in the detection of this type of lesion2,3,9 which, despite the advances in treatment with chemotherapy, radiotherapy and hormone therapy continue to be associated with a poor prognosis.4,6–8
Please cite this article as: de Zárraga Mata C, Thomas Salom G, Vilella Martorell A, Salvà Ramonell F, Maura Oliver ÁL, Dolz Abadía C. Extensión metastásica gástrica de carcinoma ductal infiltrante de mama con presentación endoscópica atípica. Gastroenterol Hepatol. 2018;41:304–305.