Endoscopic ultrasound (EUS) is a more sensitive technique than transabdominal ultrasound for the diagnosis of gallstones. This greater sensitivity, especially in the diagnosis of microlithiasis/biliary sludge, facilitates the indication of cholecystectomy in patients with symptoms of probable biliary origin but may result in over-indication of this surgery.
ObjectivesEvaluate the role of EUS in the diagnosis of minilithiasis/biliary sludge in patients with digestive symptoms of probable biliary origin by resolving the symptoms after cholecystectomy. Analyse factors related to the remission of symptoms following cholecystectomy.
Patients and methodsRetrospective, longitudinal, single-centre study based on a prospective database of 1.121 patients undergoing EUS. Seventy-four patients were identified as meeting inclusion-exclusion criteria (diagnosed with minilithiasis/sludge by EUS after presenting digestive symptoms of probable biliary origin without a history of complicated cholelithiasis). A telephone questionnaire for symptoms was conducted with cholecystectomized patients. Factors related to a good response were analysed with logistic regression analysis.
ResultsOf the 74 patients, 50 were cholecystectomized (67.5%), mean age 49 years (SEM 2.26) (41 women). Seventy percent of patients (35/50) presented remission of symptoms with median follow-up 353.5 days (95% CI, 270–632.2). The only variable associated with remission of symptoms was the presence of typical biliary colic with an OR of 7.8 (95% CI, 1.8–34; p=0.006). No complications associated with EUS were recorded. One patient (2%) suffered haemoperitoneum and 18% (9/50) suffered diarrhoea following cholecystectomy.
ConclusionsEUS is a very useful technique for the indication of cholecystectomy in patients with minilithiasis/sludge and typical symptoms of biliary colic.
La ecoendoscopia (USE) presenta mayor sensibilidad que la ecografía abdominal para el diagnóstico de litiasis biliar. Esta mayor sensibilidad, sobre todo en diagnóstico de microlitiasis/barro biliar, facilitaría una colecistectomía en pacientes con clínica digestiva de probable origen biliar, aunque podría inducir su sobre indicación.
ObjetivosEvaluar el papel de la USE en el diagnóstico de minilitiasis-barro biliar en pacientes con clínica digestiva de probable origen biliar y ecografía normal mediante la resolución de los síntomas después de colecistectomía. Analizar los factores relacionados con la remisión de la sintomatología tras colecistectomía.
Pacientes y métodoEstudio retrospectivo, longitudinal, en un centro, sobre base de datos prospectiva de 1.121 pacientes sometidos a USE. Setenta y cuatro pacientes cumplían criterios inclusión-exclusión (realización USE para estudio de minilitiasis/barro por síntomas digestivos de probable origen biliar, sin historia de colelitiasis complicada). Se realizó cuestionario telefónico de síntomas a los pacientes colecistectomizados. Los factores relacionados con buena evolución se analizaron con análisis de regresión logística.
ResultadosDe los 74 pacientes, 50 fueron colecistectomizados (67,5%), edad media 49 años (ESM 2,26) (41 mujeres). El 70% de pacientes (35/50) presentó remisión de la sintomatología (mediana de seguimiento 353,5 días) (IC 95%, 270-632,2). La única variable asociada con una remisión de la sintomatología fue la presencia de cólico biliar típico con una OR de 7,8 (IC 95%, 1,8-34; p=0,006). No se registró ninguna complicación asociada a la USE. Un paciente (2%) sufrió hemoperitoneo y un 18% (9/50) presentaron diarrea post-colecistectomía.
ConclusionesLa USE es de gran utilidad para la indicación de colecistectomía en los pacientes con minilitiasis-barro biliar y clínica típica de cólico biliar.
Cholecystectomy is one of the most common surgical procedures in clinical practice. Its indication is clear in patients with cholelithiasis and complications such as acute cholecystitis, biliary pancreatitis, obstructive jaundice, and abdominal pain of supposedly biliary origin. However, its indication is more doubtful in the case of cholelithiasis and dyspeptic symptoms attributed to a probable biliary aetiology. Indeed, it has been reported that 10–41% of these patients persist with the same symptomatology post-cholecystectomy, suggesting that cholelithiasis was not the cause of the symptoms.1–4
Between 5 and 22% of the western adult population have gallstones,5,6 and while most of them are asymptomatic, it is estimated that between 13 and 22% of cases could have associated symptoms.7,8 Most studies carried out on European populations with abdominal ultrasound have identified an incidence rate of gallstones of 0.60–1.39% per year.9,10
The terms minilithiasis and biliary sludge (also known as biliary sediment, microcrystalline disease, pseudolithiasis, and reversible cholelithiasis) are used interchangeably despite being technically different. In general, the term minilithiasis is considered to correspond to the presence of stones less than 3mm in diameter, while biliary sludge is the mass of crystals, mucin, glycoproteins, cell debris, and protein material in suspension within the bile.11 Minilithiasis and biliary sludge share the same risk factors as cholelithiasis, and some authors consider them to have the same clinical significance.12
For the study of biliary colic, abdominal ultrasound, with a diagnostic accuracy of 95% for the diagnosis of gallstones,13 is the technique of choice, although its diagnostic accuracy decreases in the case of obese patients, meteorism, gallstones<5mm, and cystic stones. When there is a firm clinical suspicion of gallstones and a negative abdominal ultrasound, the performance of an endoscopic ultrasound (EUS) is recommended.14–18 This technique provides greater sensitivity than abdominal ultrasound due to the proximity of the transducer to the gallbladder and because it works at a higher frequency. These facts improve the resolution of abdominal ultrasound and avoid the interference of abdominal gas and subcutaneous tissue. The role of EUS in the case of acute pancreatitis of unknown aetiology is well established, since, in global terms, it is capable of identifying biliary pathology as the cause of acute pancreatitis in up to 80% of patients for whom an abdominal ultrasound is negative.18–20 Furthermore, a recent meta-analysis comparing EUS and MRI cholangiography confirmed a diagnostic accuracy of 64% versus 34% in aetiological study, respectively, in cases of acute biliary pancreatitis (cholelithiasis, choledocholithiasis, minilithiasis, and biliary sludge).20 Previous studies assessing the efficacy of EUS in patients with biliary colic and normal abdominal ultrasound suggest that EUS may be a useful tool for detecting lesions in these patients. However, these are studies with limited numbers of patients which do not detail the characteristics of the clinical symptoms and they evaluate not only minilithiasis and/or biliary sludge, but also cholelithiasis and/or choledocholithiasis.14,15
Therefore, the objectives of the present study were to (1) evaluate the role of EUS in the diagnosis of minilithiasis/biliary sludge in patients with clinical symptoms of probable biliary origin and normal abdominal ultrasound and resolution of symptoms after cholecystectomy, and (2) analyse the factors related to the remission of symptoms following cholecystectomy.
Patients and methodsStudy designThis was a retrospective, longitudinal, single-center study, using a prospective database of 1.121 patients who underwent EUS between April 2014 and April 2018. Consecutive patients older than 18 years of age, referred due to digestive symptoms of possible biliary origin, with negative findings on abdominal ultrasound and other imaging techniques, and diagnosed with minilithiasis and/or biliary sludge by EUS, were included. Patients with a history of complicated cholelithiasis (choledocholithiasis, acute cholecystitis, percutaneous biliary drainage, biliary pancreatitis, and cholangitis) and asymptomatic patients were excluded.
A review of the clinical records of all patients was conducted, as well as of a telephone questionnaire with all operated patients concerning their pre- and post-cholecystectomy clinical symptoms that was made.
The following data were collected during the review of the medical records: (1) clinical data (typical biliary colic, pain in upper right quadrant, epigastralgia, nausea and vomiting, diffuse abdominal pain, and abdominal distension); (2) analytical data (total bilirubin, aspartate amino transferase (AST), alanine transferase aspartate (ALT), alkaline phosphatase (ALP), and gamma glutamyl transpeptidase (GGT)), and (3) imaging techniques performed prior to EUS (abdominal ultrasound, CT scan, and MRI). We also collected all the findings from the upper gastrointestinal endoscopy (UGE) when it had been performed. The need for emergency care or hospital admission and the use of analgesics and spasmolytics as a marker of the intensity or clinical impact of the symptoms were also recorded. We recorded other findings from the EUS, in addition to those specific to the bile duct, as well as complications resulting from the EUS and cholecystectomy.
A structured telephone questionnaire of symptoms before and after cholecystectomy was conducted by a specialist physician. The collection of clinical data was therefore retrospective for the pre-cholecystectomy assessment and prospective for the follow-up assessment. In addition, questions were asked about possible cholecystectomy-related complications that had been overlooked in the clinical record.
All examinations were performed by two medical experts in EUS under deep sedation done by anaesthesiologists at the Digestive Endoscopy Unit of the Hospital Universitari Mutua Terrassa. The Aloka Alpha 7 ultrasound console and Olympus radial GF-UE160 and/or linear GF-UCT180 echoendoscope were used.
The study protocol was approved by the ethics committee of Hospital Universitari Mútua de Terrassa.
DefinitionsClinical remission: Total disappearance of digestive symptoms following cholecystectomy.
Follow-up time: Time period between the cholecystectomy and the phone call made to assess symptoms.
Typical biliary colic: the presence of episodic abdominal pain of sudden and intense onset in the area of the upper right quadrant or epigastrium, with nausea and/or vomiting.
Minilithiasis and/or biliary sludge: the presence of isoechoic and/or hyperechoic focus without an acoustic shadow less than 5mm, which could be viewed with or without a massage in the epigastrium or right hypochondrium.
Statistical analysisResults are expressed as mean±standard error of mean (SEM), median and its 95% confidence interval (CI), and percentages and their CIs when appropriate. Univariate and multivariate statistical analyses were used to assess the variables associated with remission of symptoms following cholecystectomy. The χ2 test and the Fisher exact test were used to compare proportions, and the Student t test or its non-parametric equivalents were used to compare quantitative variables when necessary. A binary logistic regression analysis was used for the multivariate analysis, including those variables with a p<0.05 in the univariate analysis. A result was considered significant when p<0.05. The SPSS statistical program (version 15.0; SPSS, Chicago, IL) was used.
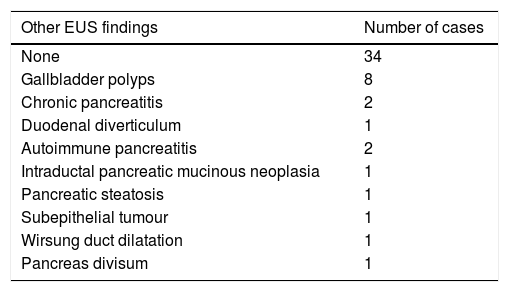
ResultsDemographic and clinical variables of the study populationA total of 74 patients in whom the EUS identified sludge and/or biliary minilithiasis, to study digestive symptoms of probable biliary origin, were identified. Of these patients, 50 were cholecystectomized (67.5%) (mean age 49±2.3 years; 41 women, 82%). Fig. 1 is a flowchart depicting patient inclusion. Table 1 describes other findings found in the EUS.
Findings of the EUS other than minilithiasis – biliary sludge (n=50 cholecystectomized patients).
| Other EUS findings | Number of cases |
|---|---|
| None | 34 |
| Gallbladder polyps | 8 |
| Chronic pancreatitis | 2 |
| Duodenal diverticulum | 1 |
| Autoimmune pancreatitis | 2 |
| Intraductal pancreatic mucinous neoplasia | 1 |
| Pancreatic steatosis | 1 |
| Subepithelial tumour | 1 |
| Wirsung duct dilatation | 1 |
| Pancreas divisum | 1 |
Fig. 2 shows liver biochemistry patterns of cholecystectomized patients, which were normal in 67% of the cases (n=33). Increased bilirubin levels were detected in 6% (n=3) and increased levels of cholestasis and/or aminotransferases were detected in 20–25% of cases (n=22). In all cases except for one, a hepatic disease was responsible for the alteration, including 10 cases of non-alcoholic steatohepatitis, one case of chronic alcohol-related liver disease, 3 cases of toxic hepatitis, 1 case of autoimmune pancreatitis, and 1 case of Gilbert's syndrome.
Liver biochemistry results of the analysis performed in the year prior to the diagnosis of biliary-sludge minilithiasis. Footnote: 4% (1/50) of patients did not have a blood test performed in the year prior to the diagnosis of minilithiasis and/or bile sludge. 6% (3/50) of patients did not have bilirubin level results prior to surgery.
Regarding the imaging technique previously performed, all patients had undergone an abdominal ultrasound, 20% (10/50) had undergone an abdominal CT scan, and 30% (15/50) had undergone an MRI. No patients presented pathological findings suggestive of a biliary pathology, which is why an EUS was requested.
In 50% of the patients (25/50), an UGE had been performed in the year prior to the diagnosis of minilithiasis and/or bile sludge, though without relevant pathological findings that could explain the clinical picture.
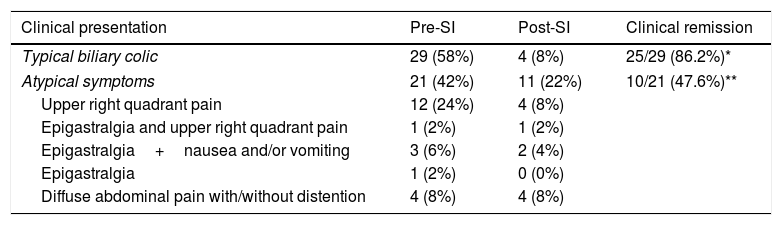
Remission of digestive symptoms and related factorsSeventy percent of cholecystectomized patients (35/50) achieved remission of clinical symptoms at the end of follow-up. There was no statistically significant difference in the follow-up time between patients who achieved and those who failed to achieve remission of symptoms: 344 days (95% CI; 257–581.7) vs 637 days (95% CI; 95.7–867.5), respectively; p=0.664. Table 2 lists clinical symptoms before and after surgery. Fifty-eight percent (n=29) of patients presented typical clinical signs of hepatic colic, while 42% (n=21) presented atypical symptoms. There were significant differences in the frequency of clinical remission after cholecystectomy between the two groups of patients, namely 86.2% (n=25) of patients with typical biliary colic versus 47.6% (n=10) with atypical symptoms (p=0.003). Of the patients with atypical symptoms who achieved remission, 67% (n=8) had pain in the upper right quadrant while 22% (n=2) presented other digestive symptoms. In the group of patients with atypical symptoms who achieved remission, 59% (n=10) experienced pain in the upper right quadrant or epigastrium with or without nausea. No patient with symptoms of diffuse abdominal pain with or without abdominal distension achieved clinical remission (p=0.09 vs. other atypical symptoms).
Frequency of clinical symptoms before and after cholecystectomy.
| Clinical presentation | Pre-SI | Post-SI | Clinical remission |
|---|---|---|---|
| Typical biliary colic | 29 (58%) | 4 (8%) | 25/29 (86.2%)* |
| Atypical symptoms | 21 (42%) | 11 (22%) | 10/21 (47.6%)** |
| Upper right quadrant pain | 12 (24%) | 4 (8%) | |
| Epigastralgia and upper right quadrant pain | 1 (2%) | 1 (2%) | |
| Epigastralgia+nausea and/or vomiting | 3 (6%) | 2 (4%) | |
| Epigastralgia | 1 (2%) | 0 (0%) | |
| Diffuse abdominal pain with/without distention | 4 (8%) | 4 (8%) | |
SI: surgical intervention.
Regarding the severity of digestive symptoms, as measured by the need for hospital care, 52% of patients (26/50) required emergency care and 12% (6/50) required hospital admission, with no significant differences between patients with typical and those with atypical symptoms.
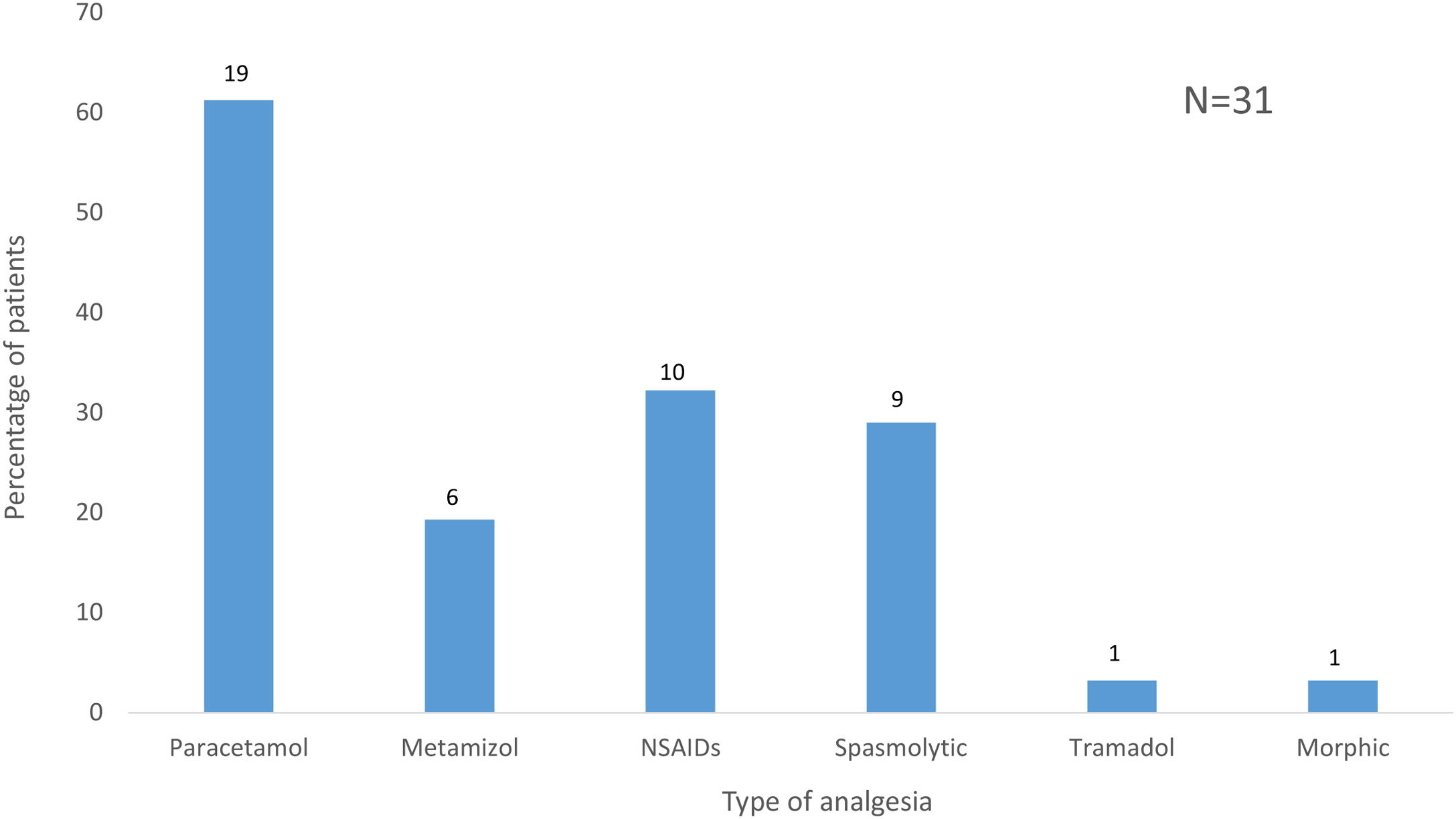
Sixty-two percent (31/50) of cholecystectomized patients required analgesia for the control of symptoms prior to surgery. The group of patients with typical biliary colic required analgesia with a greater frequency than the group of patients with atypical symptoms (75.9% vs. 42.9%; p=0.018). Fig. 3 details the type of analgesia used both on an outpatient basis and during admissions to the emergency ward and hospitalization.
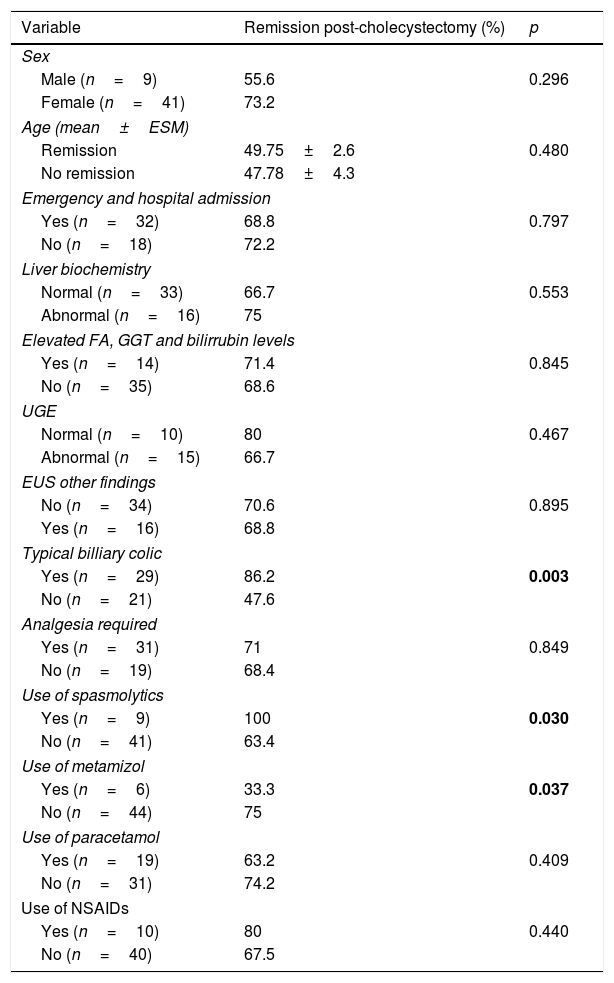
Table 3 shows the factors related to remission of symptoms following cholecystectomy. In the univariate analysis, these factors were the presence of typical biliary colic (86.2 vs 47.6%; p=0.003) and the use of spasmolytics (100 vs 63.7%; p=0.030). In contrast, the use of metamizole (33.3% vs 75%; p=0.037) was significantly associated with failure to achieve remission of symptoms. In the multivariate analysis, the only variable associated with remission of symptoms following cholecystectomy was the presence of typical biliary colic, with an OR of 7.8 (CI, 1.8–34; p=0.006).
Variables related to the remission of symptoms post-cholecystectomy. Univariate analysis. N=50.
| Variable | Remission post-cholecystectomy (%) | p |
|---|---|---|
| Sex | ||
| Male (n=9) | 55.6 | 0.296 |
| Female (n=41) | 73.2 | |
| Age (mean±ESM) | ||
| Remission | 49.75±2.6 | 0.480 |
| No remission | 47.78±4.3 | |
| Emergency and hospital admission | ||
| Yes (n=32) | 68.8 | 0.797 |
| No (n=18) | 72.2 | |
| Liver biochemistry | ||
| Normal (n=33) | 66.7 | 0.553 |
| Abnormal (n=16) | 75 | |
| Elevated FA, GGT and bilirrubin levels | ||
| Yes (n=14) | 71.4 | 0.845 |
| No (n=35) | 68.6 | |
| UGE | ||
| Normal (n=10) | 80 | 0.467 |
| Abnormal (n=15) | 66.7 | |
| EUS other findings | ||
| No (n=34) | 70.6 | 0.895 |
| Yes (n=16) | 68.8 | |
| Typical billiary colic | ||
| Yes (n=29) | 86.2 | 0.003 |
| No (n=21) | 47.6 | |
| Analgesia required | ||
| Yes (n=31) | 71 | 0.849 |
| No (n=19) | 68.4 | |
| Use of spasmolytics | ||
| Yes (n=9) | 100 | 0.030 |
| No (n=41) | 63.4 | |
| Use of metamizol | ||
| Yes (n=6) | 33.3 | 0.037 |
| No (n=44) | 75 | |
| Use of paracetamol | ||
| Yes (n=19) | 63.2 | 0.409 |
| No (n=31) | 74.2 | |
| Use of NSAIDs | ||
| Yes (n=10) | 80 | 0.440 |
| No (n=40) | 67.5 | |
UGE: upper gastrointestinal endoscopy; EUS: endoscopic ultrasound; NSAIDs: non-steroidal anti-inflammatory drugs.
In bold is marked the significative values with a p < 0.05.
Of the 50 cholecystectomised patients, one (2%) presented an immediate complication related to the cholecystectomy, consisting of haemoperitoneum and surgical bed haematoma, requiring laparotomy and peritoneal lavage.
Eighteen percent (9/50) of the patients experienced diarrhoea after cholecystectomy, and 66.6% (6/9) of those patients required treatment with cholestyramine, which met with a good clinical response. Of the remaining 3 patients, 2 did not require treatment for occasional and self-limited diarrhoea, and in the case of one patient, diarrhoea was successfully treated with Plantago ovata.
No complications were recorded in relation to the EUS technique.
DiscussionTo the best of our knowledge, this is the first study to evaluate the role of EUS indication of cholecystectomy after the diagnosis of minilithiasis and/or biliary sludge not diagnosed by other imaging techniques. The diagnostic usefulness of EUS was assessed by means of the remission of digestive symptoms after cholecystectomy. Surgical treatment is generally indicated in patients with uncomplicated symptomatic gallstones. According to the latest EASL clinical practice guidelines, published in 2016, cholecystectomy should be performed in patients diagnosed with cholelithiasis, depending on the intensity and number of symptomatic episodes.21 This indication leaves a wide margin of decision and there is no clear consensus on the best criteria for the correct selection of patients for surgical treatment.22–24 Furthermore, in most studies the diagnosis of gallstones is made by abdominal ultrasound, and it is not clear whether minilithiasis and/or bile sludge plays the same pathogenic role as stones as an indication for cholecystectomy. All of the patients in our study had normal imaging techniques prior to EUS, and most patients had normal liver biochemistry. In patients with abnormal liver tests, another intrahepatic or non-biliary cause of the disorder was found, suggesting that they were patients with an uncomplicated cholelithiasis.
Overall, up to 70% of patients presented remission of symptoms at the end of follow-up, which is a similar rate to the data published in the literature regarding lithiasis detected by abdominal ultrasound.1–4 Therefore, 30% of patients did not experience relief of their digestive symptoms despite cholecystectomy, which means they underwent an unnecessary cholecystectomy with the associated risks of complications and health care costs. An adequate assessment of symptoms is key to establishing a correct aetiological relationship. The main characteristics of pain of biliary origin are its sudden onset and the fact that it is generally of great intensity, located in the area of the right upper quadrant or epigastrium and generally associated with nausea and vomiting. The onset of these attacks is unpredictable and they begin approximately one hour after meals and in most cases are resolved spontaneously. Episodes of pain recur after a first episode of biliary colic in around 50% of patients.25 In our study, we found that a typical clinical picture of biliary colic in patients diagnosed with minilithiasis-sludge by EUS was associated with clinical remission after cholecystectomy in 86% of the cases.
These results are even better than those obtained in patients diagnosed with symptomatic cholelithiasis by abdominal ultrasound (60–70%), and, therefore, lend support to cholecystectomy in patients with typical symptoms and minilithiasis-biliary sludge diagnosed by EUS.1–4,23 The greater remission of the symptomatology observed in our study is probably due to the fact that our patients were selected due to high clinical suspicion, and it also supports the idea that accurate clinical assessment is very important prior to performing such an examination. Previous studies have suggested that the clinical presentation is not always so specific, as 45% of patients with colic pain of probable biliary origin did not have gallstones detected by abdominal ultrasound.26,27 But these percentages would probably have been lower with the use of EUS since abdominal ultrasound under-diagnoses lithiasis. The results of the present study, with a positive response to cholecystectomy in symptomatic patients with biliary minilithiasis-sludge in a high percentage of cases, support this hypothesis. Furthermore, this high percentage of clinical remission also indicates that the technique did not lead to overdiagnosis and a consequently higher rate of unnecessary cholecystectomies.
In this cohort we detected a group of patients who presented only some of the clinical symptoms of billiary colic and who had a good response to cholecystectomy in a high percentage of cases (59%). Fundamentally, these were patients presenting with pain in the right upper quadrant or epigastrium with or without nausea or vomiting. The retrospective nature of the study does not allow for further refinement regarding the specific clinical characteristics predictive of a good response to cholecystectomy in this subgroup of patients with a ‘minor’ form of biliary colic. Finally, there was a small group of patients with non-specific diffuse abdominal pain with or without associated bloating who failed to respond to cholecystectomy, suggesting that the symptoms in these cases were not clearly biliary in origin.
Prospective studies featuring large series of patients with minilithiasis and/or biliary sludge detected by EUS should delve into the characteristics of the individual symptoms predictive of a good response in order to identify all patients who may benefit from cholecystectomy.
Regarding the immediate and late complications associated with surgery, it should be noted that one patient had a hemoperitoneum and 18% of patients post-cholecystectomy diarrhoea. These data are very similar to those reported in the literature, with the frequency of diarrhoea due to malabsorption of bile acids varying, depending on the study, from 9% to 20%.28,29 It is therefore of the utmost importance to perform an accurate aetiological study with this type of patient in order to avoid a surgical intervention that not only fails to resolve the clinical picture but also carries associated complications.
Despite being an invasive, high-cost technique, EUS has a very low complication rate30 (0% in the present series). Its advantage, in cases that are clinically compatible and in which other imaging techniques yield negative results, is its greater sensitivity in the detection of bile sludge and minilithiasis.18–20 This greater sensitivity is due to the proximity of the transducer to the gallbladder and the possibility of massaging the epigastric-hypogastric area. It therefore allows one to achieve an indication for cholecystectomy based on objective morphological data.
One limitation of our study, apart from its retrospective nature, with the biases that this entails, is that we do not have information at our disposal regarding those patients who were suspected of having symptoms of biliary origin and whose EUS result was normal. This creates the need for a prospective study with an accurate assessment of pre- and post-cholecystectomy symptoms, which is particularly important in atypical forms of suspected biliary colic.
These results confirm that minilithiasis and/or bile sludge have the same pathological significance as lithiasis and should therefore be considered to be an aetiological factor, especially in cases presenting a typical clinical picture of biliary colic, since it is associated with an OR>7 of long-term clinical remission.
In conclusion, EUS is a useful technique for the diagnosis of biliary minilithiasis-sludge in patients presenting with symptoms suggestive of a biliary origin but with a normal abdominal ultrasound, and it allows for the indication of surgical treatment by cholecystectomy, which is associated with a high percentage of long-term clinical remission. A clinical presentation in the form of typical biliary colic compared to other forms of presentation is associated with a seven times greater likelihood of long-term clinical remission. Prospective studies with a larger number of patients are needed to evaluate whether there is an attenuated clinical presentation of biliary colic due to minilithiasis/sludge which may also benefit from cholecystectomy.
Authorship statementGuarantor of article: C. Loras.
Specific author contributions: A. Montenegro and C. Loras performed the research; A. Montenegro, X. Andújar, and C. Loras collected and analysed the data; C. Loras designed the research study; A. Montenegro, C. Loras, M. Esteve, and F. Bañares wrote the paper; and A. Montenegro, C. Loras, X. Andújar, M. Esteve, and F. Bañares contributed to the design of the study.
ALL authors approved the final version of the article, including the authorship list.
Conflict of interestDrs. Montenegro, Andújar, Fernández-Bañares, Esteve, and Loras have no conflicts of interest or financial ties to disclose.