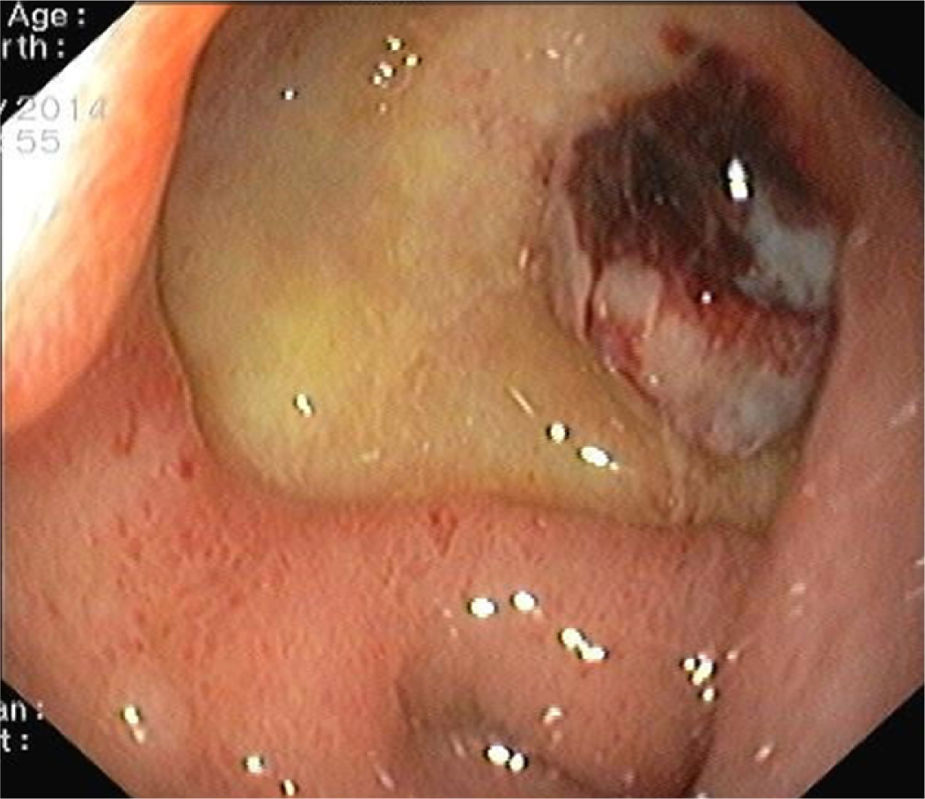
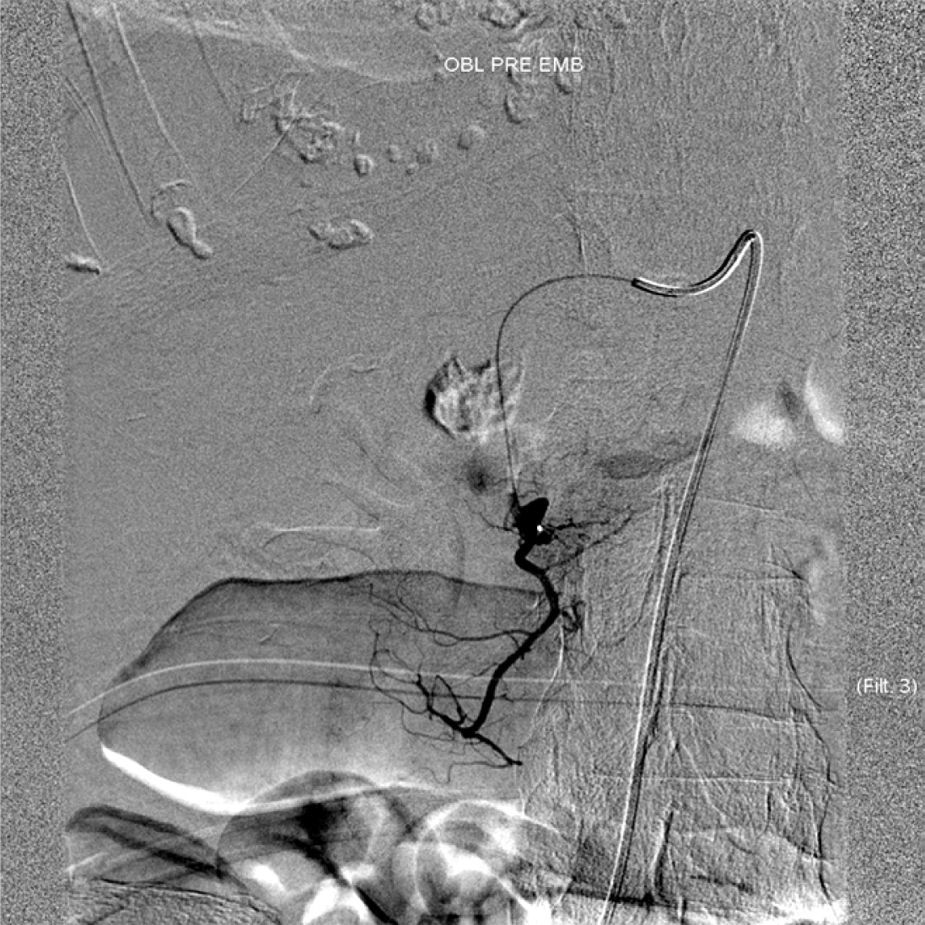
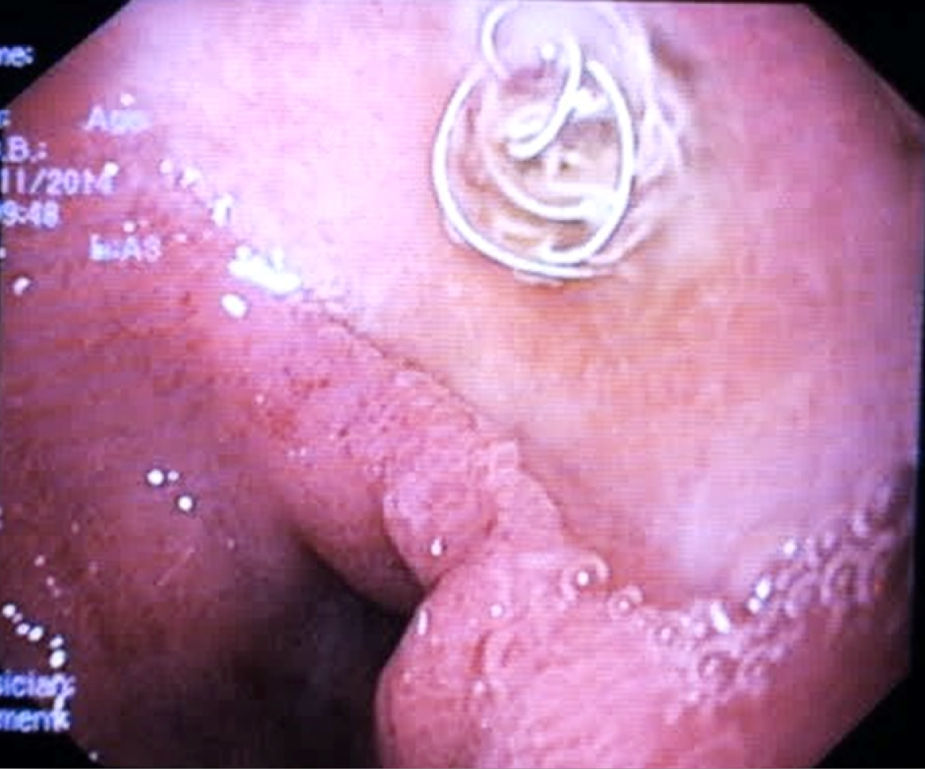
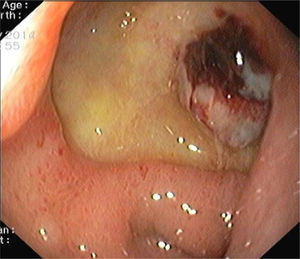
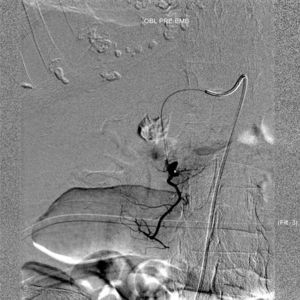
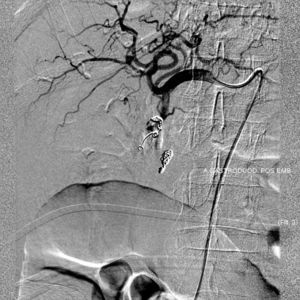
A 81-year-old woman with previous history of ulcerative colitis under corticotherapy was admitted to the emergency room with a two-day history of melena with orthostatic hypotension and severe anemia (hemoglobin level of 5.2g/dL). Emergency upper endoscopy was performed and a large deep ulcer with a pulsatile visible vessel was seen along the posterior aspect of the duodenal bulb (Fig. 1). Hemostatic therapy with injection of 6mL of epinephrine (100μg/mL) was carried out. Due to its large size, posterior location, and associated risk of recurrent bleeding in this high-risk patient, no further endoscopic therapeutic maneuvers were performed. The patient underwent mesenteric angiography with selective embolization of the superior pancreaticoduodenal artery. The anterior branch had a pseudoaneurism that was selectively embolized with 3–5mm platinum coils (Figs. 2 and 3). The patient underwent endoscopy 72h later which showed a coil protruding into the lumen from the visible vessel at the ulcer site (Fig. 4). There was no active bleeding or oozing. No bleeding event was detected within 30 days after the performed treatment.
The embolization of the gastroduodenal artery is a safe and effective technique in bleeding duodenal ulcer in patients with high surgical risk. The endoscopic view of arterial embolization coils is a rare but known complication.1–5 Due to the small number of described cases, the prognostic value of this finding with regard to rebleeding incidence remains unclear.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.