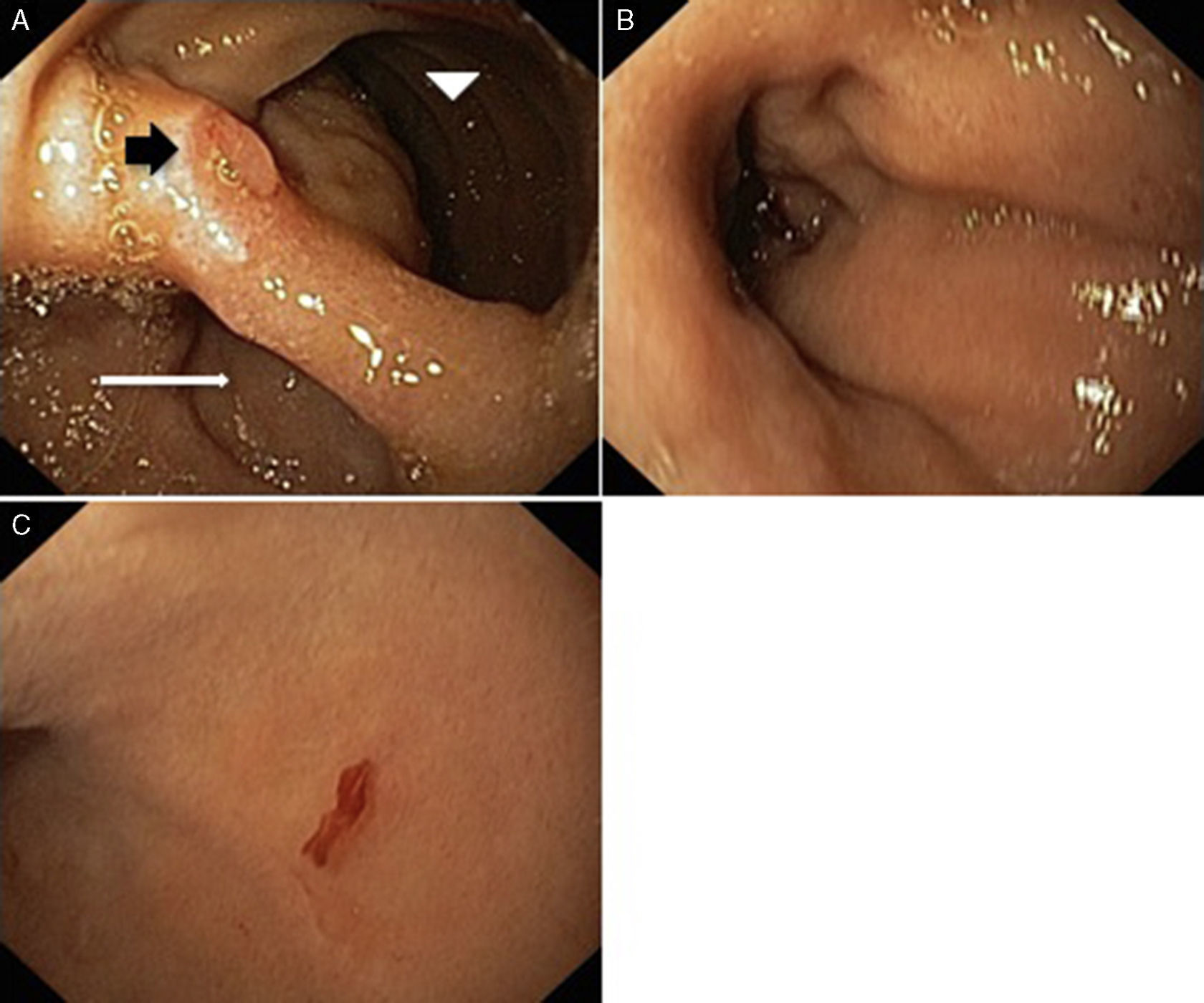
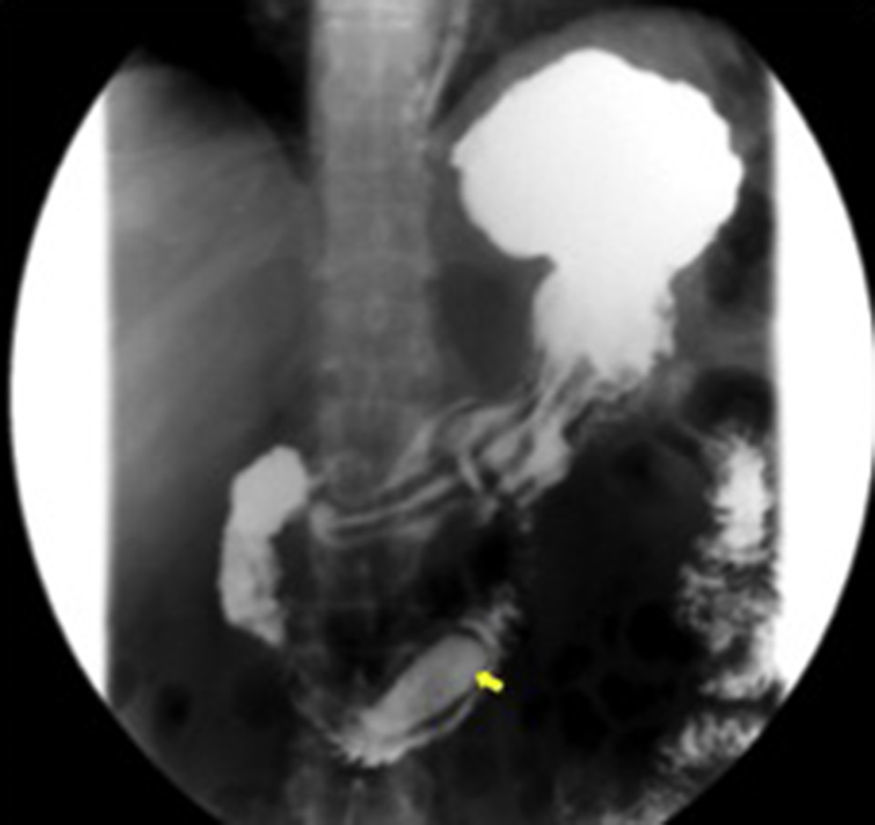
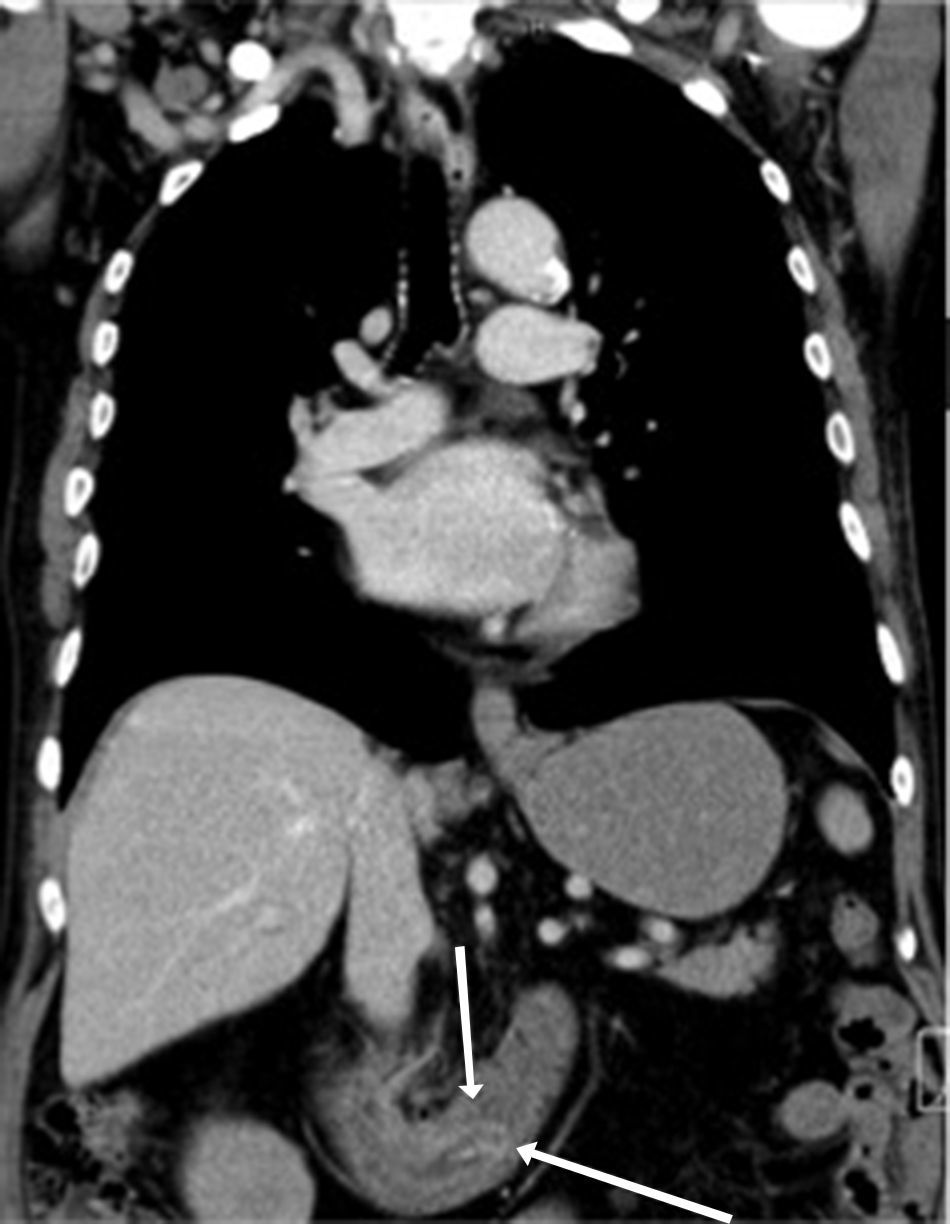
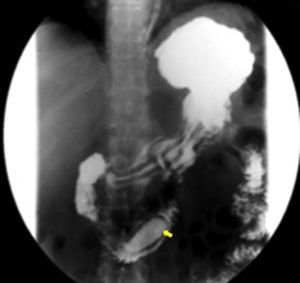
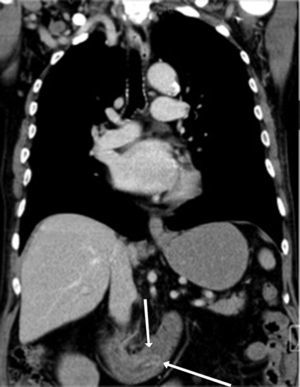
A 67-year-old man was admitted to the emergency department with a recent history of melena and progressive fatigue. He had a past medical history of hypertension, dyslipidemia, ischemic heart disease, chronic renal failure and was on antiaggregation therapy. Physical examination showed pallor and hemodynamic stability. Laboratory work-up revealed normocytic anemia (hemoglobin 9g/dL; normal: 13–17), elevated blood urea nitrogen (35mg/dL; normal: 8.4–25.7) and worsened renal failure (creatinine 3mg/dL from a baseline of 2.2mg/dL; normal: 0.7–1.3). Upper gastrointestinal endoscopy demonstrated a double lumen in the second portion of the duodenum corresponding to a large saccular structure surrounded on both sides by duodenal mucosa. Spontaneous oozing of fresh blood was seen from a punctiform, non-ulcerated lesion located in the diverticular mucosa (Fig. 1). No other lesions were endoscopically seen in the upper digestive tract. We admitted a vascular lesion within the diverticulum and argon plasma coagulation was then applied without recurrent bleeding. Subsequent esophagogastroduodenal transit was performed showing a barium filled saccular structure in the second portion of the duodenum extending to the third portion and surrounded by a radiolucent line. These findings confirmed the endoscopic suspicion of a “windsock” diverticulum (Fig. 2). Computed tomography evidenced a bowel loop within another loop consistent with the previous findings and excluded other “major” lesions (Fig. 3). Patient was discharged and did not present further episodes of bleeding, however due to complications of his comorbid disease he died 4 months later.
Endoscopic images of an intraluminal duodenal (“windsock”) diverticulum within the second portion of the duodenum. (A) Duodenum with a double lumen: white arrow – diverticular lumen; arrow head – true duodenal lumen; black arrow – septum with major papila. (B) Diverticular lumen with apical fresh blood oozing. (C) Punctiform lesion with oozing bleed in the diverticular mucosa.
Intraluminal duodenal diverticulum (IDD), also known as “windsock” diverticulum, is a rare congenital abnormality that seems to result from an incomplete recanalization of the foregut lumen.1,2 Symptoms usually do not appear until the third decade of life.3,4 When symptomatic, clinical manifestation is nonespecific and consists mainly of epigastric pain, early saciety, nausea or vomiting.3,5 Less commonly, IDD may complicate with gastrointestinal bleeding,1,3,4 pancreatitis or duodenal obstruction.3 Endoscopic appearance may be challenging: IDD may be collapsed and pass unnoticed, a long sac may be mistaken for the duodenal lumen3 and an inverted diverticulum may resemble a large polyp.1 Furthermore, it may be confusing if the endoscopist is not familiar with this rare entity.1 There are some key elements concerning IDD, which may help to distinguish from extraluminal duodenal diverticulum: (1) both sides of the IDD are lined by duodenal mucosa; (2) there is a diaphragm that crosses the duodenal lumen and forms the intraluminal septum of the diverticulum; (3) there is a separate opening in the diaphragm corresponding to the true lumen.2
Definitive treatment has been proposed in symptomatic IDD due to the high recurrence rate of symptoms, except in poor risk patients in whom conservative treatment is an option.3 Surgical intervention was the traditional treatment, however, endoscopic management has been advocated with a satisfactory outcome.1,2 Several endoscopic techniques have been described namely diverticulectomy using snare excision or diverticulotomy (using needle devices, argon plasma coagulation or Nd:YAG laser).2
Given the rarity of this lesion and its form of presentation, the authors present iconography that highlights the characteristic endoscopic findings of this entity that may prompt direct diagnosis.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors have no conflicts of interest to declare.