A 68-year-old male was admitted to the Gastroenterology department for elective percutaneous endoscopic gastrostomy (PEG) tube placement. The patient had neurologic dysphagia secondary to amiotrophic lateral sclerosis, recurrent low respiratory tract infections and was receiving nutricional support from a nasogastric tube since the previous four months.
A 20Fr PEG tube (Covidien®) was placed by “pull-on-string” technique, with the external bumper on the 3.5cm mark. There were no complications during the procedure or after a 24-hour surveillance period. Enteral feeding with the PEG tube was successfully started. Oral and written educational support was provided to the caregivers.
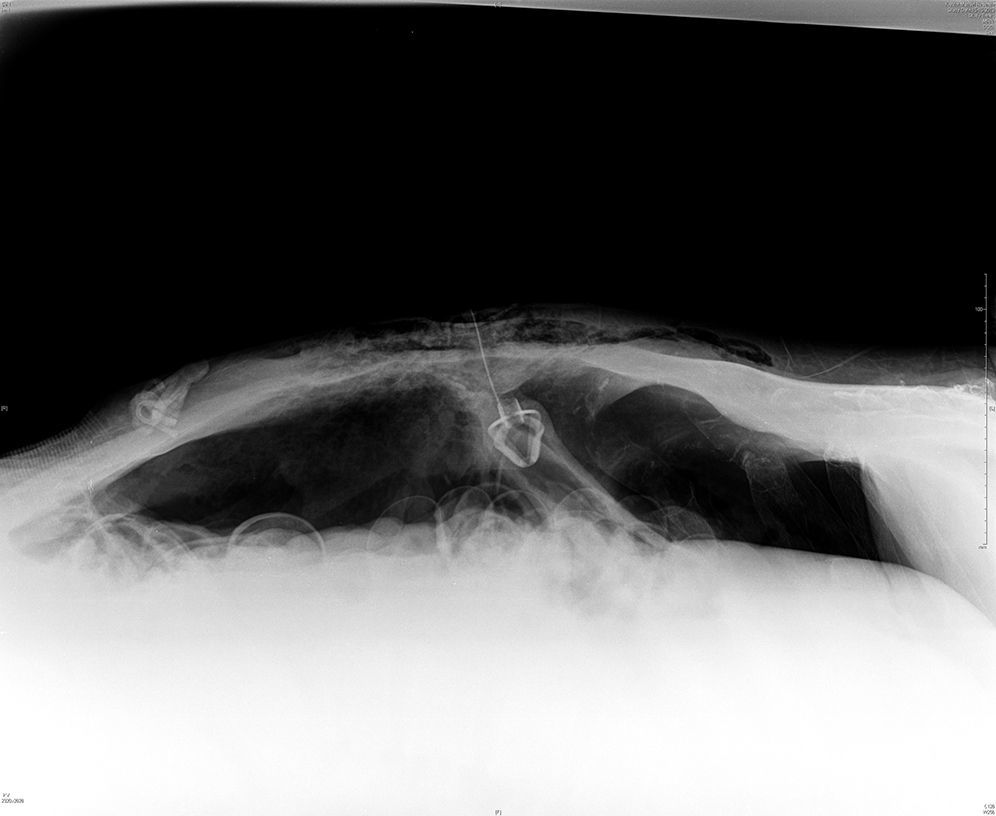
Four days after PEG tube placement, the patient developed abdominal distension and dyspnea. Complications with feeding, hygiene and PEG tube mobilization were denied by the caregivers. Polypnea and subcutaneous emphysema in the upper and lower left quadrants were noticed, as well as abdominal distension and diffuse tenderness with peritoneal signs. Abdominal plain radiography demonstrated pneumoperitoneum and the internal bumper of the PEG tube in intraperitoneal location (Fig. 1). An exploratory laparotomy was undertaken and a perforation site in the gastric greater curvature was identified, although it was covered by epiplon with engaging fibrin. Surgical washing, raphy with epiplonoplasty and an Witzel feeding jejunostomy were done. The patient recovered successfully after surgery.
2DiscussionPEG tube placement is a safe and effective method allowing the enteric nutritional support when oral ingestion is compromised.1
Pneumoperitoneum complicates the procedure in 5–16%,3,4 occurring during the tube placement or after early tube mobilization, before fistula path is definitely created (the first 14–20 days).2 The presence of a small amount of air in the peritoneal cavity is a benign finding due to air inflated into the gastric lumen during endoscopy.1 In 85–91% of these cases the course is benign, with spontaneous and quick recovery (mean time to resolution was 2.7 days).1,3 However, pneumoperitoneum can be a sign of a more severe complication, as intestinal perforation. The clinical challenge is the distinction between these two entities.
Thus, the suspicion of pneumoperitoneum requires evaluation and must not always be assumed as benign. The asymptomatic and stable patient should be kept under surveillance and usually no intervention is needed.1,5 However, in the presence of abdominal pain, tenderness, rigidity, progressive distension, fever, hemodynamic instability, leucocytosis or evidence of free fluid in the peritoneal cavity in addition to free air, a surgical attitude must be strongly considered.1,5
In our current case, excessive traction of the tube with release of the internal bumper into the peritoneal cavity and consequent flow of air from the gastric lumen was the probable cause of the pneumoperitoneum. A surgical approach was taken due to the presence peritoneal signs and ventilatory compromise secondary to the severe abdominal distention.
In conclusion, checking for pneumoperitoneum routinely is pointless in the absence of peritoneal signs. Clinical signs of peritonitis are a much more accurate marker of acute complication than the presence of pneumoperitoneum in a postprocedure radiograph.3
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.