Biliary obstruction is usually caused by choledocholithiasis. However, in some circumstances, alternative or concurring unusual ethiologies such as portal hypertensive biliopathy (PHB) must be considered.
Clinical caseWe present the case of a 36-year-old female complaining of jaundice and pruritus. Liver function tests were compatible with biliary obstruction and the ultrasound scan of the abdomen showed dilatation of the intrahepatic biliary ducts, a dilated common bile duct (CBD) and biliary calculi. The computed tomography of the abdomen revealed a portal cavernoma encasing the CBD.
DiscussionPortal cavernoma, the hallmark of extrahepatic portal venous obstruction, can cause PHB. When symptomatic, chronic cholestasis is present if a dominant stricture exists whereas biliary pain and acute cholangitis occur when choledocholithiasis prevails. Management must be individualized and usually includes endoscopic therapy to address choledocholithiasis and shunt surgery for definitive treatment.
A causa mais comum de icterícia obstrutiva é a coledocolitíase. No entanto, no contexto clínico adequado, devem ser consideradas etiologias alternativas ou concomitantes, nomeadamente a biliopatia hipertensiva portal (BHP).
Caso clínicoApresentamos o caso de uma doente do sexo feminino com 36 anos de idade com icterícia e prurido. O estudo bioquímico era compatível com icterícia obstrutiva e o estudo ecográfico do abdómen revelou dilatação das vias biliares intra-hepáticas e do colédoco associados a litíase biliar. A tomografia computorizada abdominal realizada mostrou a existência um cavernoma da veia porta a envolver o colédoco.
DiscussãoO cavernoma da porta, no contexto de obstrução portal venosa extra-hepática pode complicar-se com BHP. Quando sintomática manifesta-se por colestase crónica caso exista uma estenose dominante ou dor biliar e/ou colangite aguda quando predomina a litíase. O tratamento definitivo é individualizado, incluindo terapêutica endoscópica visando a litíase associada e uma derivação cirúrgica venosa porto-sistémica.
Jaundice is the most frequent presentation of liver and biliary disease and the diagnosis of obstructive jaundice can usually be established with simple laboratory tests and ultrasonography.1 Choledocholithiasis is by far the most common cause of biliary obstruction but other important conditions to consider are biliary or extrabiliary malignancy, pancreatitis, non-neoplastic biliary strictures and parasites.2 However, as evidenced by our case report, imaging investigations may bring to light an uncommon cause of biliary obstruction such as portal hypertensive biliopathy (PHB) that requires not only the relief of the obstructive jaundice but also the diagnosis of the cause of portal hypertension and its management.3
2Clinical caseA 36-year-old woman presented to the emergency department due to jaundice that had first become apparent three days earlier. She also reported pruritus for the last week, pale stools and dark discoloration of the urine. While denying any abdominal pain, the patient did complain of nausea and vomiting.
At the time of presentation the patient did not recall any significant past medical history including blood transfusions and was taking no prescription or over-the-counter drugs. She also denied unprotected sexual intercourse.
Physical examination was notable for marked jaundice and scratch induced excoriations. The gallbladder was not palpable but a nontender hepatomegaly extending 2cm below the ribcage was noted. The remaining of the physical examination was unremarkable.
The initial laboratory test results consisted of a normal complete blood count and a normal prothrombin time of 10.2s (control 12.0s). Total bilirubin was elevated at 9.9mg/dL (0.3–1.2mg/dL) with a conjugated bilirubin of 8.7mg/dL. Alkaline phosphatase was also raised at 237IU/L (35–105IU/L) as was aspartate aminotransferase with a value of 170IU/L (<32IU/L).
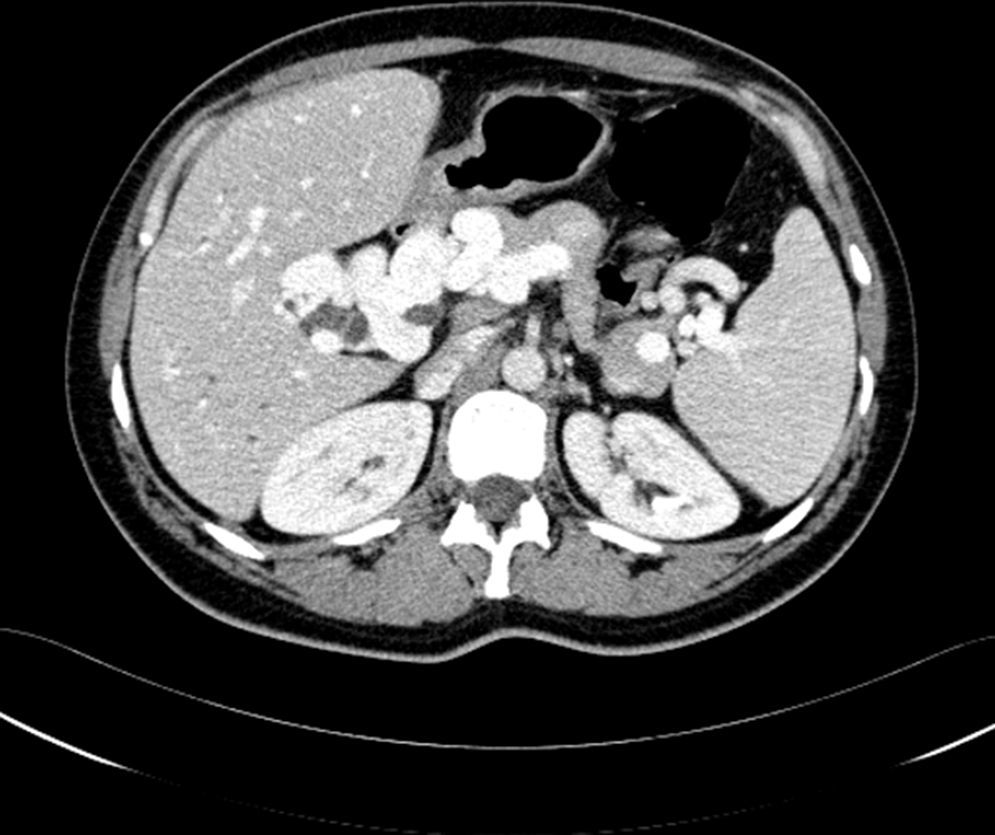
An ultrasound scan of the abdomen was performed and showed dilatation of the intrahepatic biliary ducts as well as a dilated common bile duct measuring 8.5mm in diameter with at least one biliary calculus in its lumen. Gallstones were also present and mild hepatomegaly and splenomegaly were reported. Due to the concern of portal hypertension raised by the presence of splenomegaly, a computed tomography (CT) of the abdomen was ordered and revealed an extensive portosystemic collateral circulation and a portal cavernoma encasing the common bile duct.
At this time the patient's mother reported to the attending physician that her daughter had suffered from neonatal sepsis secondary to omphalitis two weeks after birth (Fig. 1).
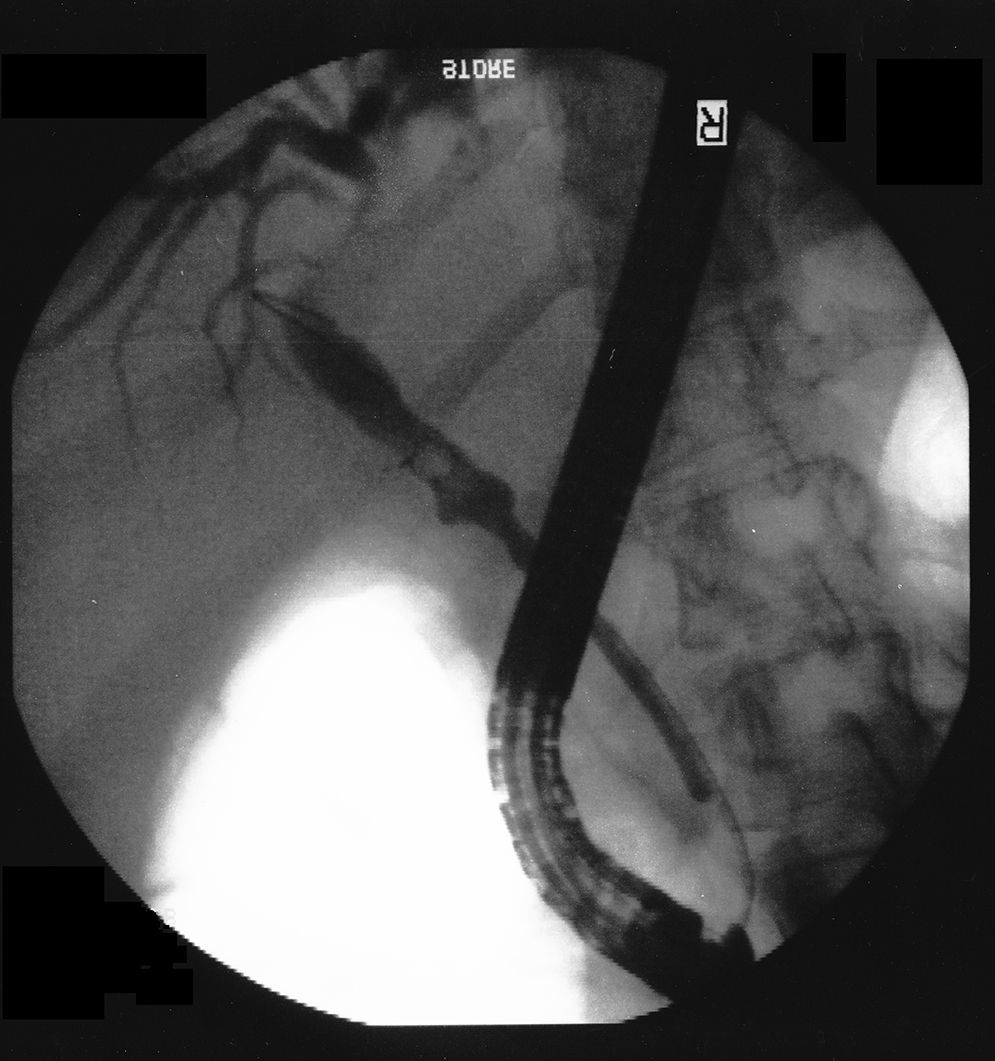
After appropriate informed consent was obtained, an endoscopic retrograde cholangiopancreatography (ERCP) was performed to relieve the biliary obstruction. The cholangiogram showed that while the common bile duct had a normal diameter in its distal half, the proximal portion was dilated at 10mm and subtraction images compatible with calculi were present. In the transition between these two segments of the common bile duct a saccular dilation was formed and also contained calculi. After sphincterotomy calculi removal was ensued requiring mechanical lithotripsy and a plastic stent was left in the common bile duct since it was not possible to remove all calculi.
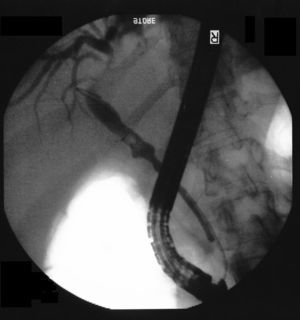
In order to investigate conditions contributing for the cavernoma's development, a thrombophilia screen was ordered and its results were negative. Further anatomic definition was attained with the help of a magnetic resonance cholangiography that revealed, in addition to the persistence of calculi in the biliary ducts, an anatomical variant with the biliary drainage of the posterior segments of the right hepatic lobe being done to the left hepatic duct (Fig. 2). An esophagogastroduodenoscopy was performed and was unremarkable, showing no signs of portal hypertension namely esophageal varices.
The patient had an excellent outcome after biliary stenting with total remission of symptoms, jaundice and normalization of biochemical markers of cholestasis. The case was presented to a hepatobiliary surgeon and the patient is currently waiting for portosystemic shunt surgery.
3DiscussionIn this clinical report we present the case of a patient with biliary obstruction caused by PHB which in turn resulted from extrahepatic portal venous obstruction (EHPVO).
Portal cavernoma, also designated as portal vein cavernomatous transformation, consists in the formation of varicose collaterals around an occluded segment of the portal vein and is the hallmark feature of EHPVO.4 This compensatory but pathological phenomenon represents an important cause of portal hypertension, especially in developing countries where it accounts for 40% of portal hypertension cases.5 In most instances it presents in children as major upper gastrointestinal bleeding.6 However, in a minority of individuals from which our patient is an example, EHPVO may only manifest itself in adulthood as a cause of chronic liver disease, PHB or an incidental finding.7 The etiology of the portal cavernoma itself is only identified in about half the cases, being omphalitis and intra-abdominal sepsis the leading causes in the pediatric population while in adults a wide array of conditions such as thrombophilia, intra-abdominal infection or malignancy, myeloproliferative disorders and cirrhosis have been implicated.7,8 In this case we believe that the driving force for the portal cavernoma development was the omphalitis episode that occurred in the patient's infancy. Concurring conditions such as thrombophilia, abdominal sepsis or malignancy were excluded due to clinical observation, evolution and appropriate laboratory testing and imaging.
PHB, also commonly named pseudosclerosing cholangitis, portal ductopathy or simply portal biliopathy, is used to describe the abnormalities observed in the full extent of the biliary tract including intrahepatic and extrahepatic bile ducts, gallbladder and cystic duct in patients with portal hypertension.3 This condition is mainly a feature of EHPVO where radiological evidence of PHB is present in 81–100% of patients but it can be found in a small proportion of individuals with other causes of portal hypertension.9
The pathogenesis of PHB is based on three mechanisms that may act individually or simultaneously: compression of the pliable common bile duct by the collaterals that form the portal cavernoma and the connective tissue that develops with time and encases this duct; ischemia induced by portal thrombosis and subsequent sclerosis of the vessels that drain the bile ducts resulting in the formation of biliary strictures; inflammation and deposition of connective tissue caused by bacterial cholangitis.9
Choledocholithiasis is a common feature of PHB and can be present in as much as 84% of patients even though this high value may represent a selection bias.10 The increased occurrence of biliary stones in PHB is likely justified by chronic cholestasis and changes in the constituents of bile while reduced portal flow and liver dysfunction may also play a role.11
The proportion of patients with EHPVO that experience symptoms related to PHB ranges between 5% and 38%.12,13 When symptoms do occur, the clinical presentation is usually either one of chronic cholestasis when strictures dominate or of biliary pain or acute cholangitis when choledocholithiasis is the main culprit.3 In this case, while there was no complaint of significant pain or features of acute cholangitis, we believe that the presentation was dominated by acute obstruction of a dominant stricture of the common bile duct by a biliary stone. This view is not only supported by the radiological diagnosis of choledocholithiasis but also by the fast resolution of jaundice and cholestasis following biliary stenting. Individuals who do present with symptoms of PHB tend to do so at an older age when compared with children presenting with upper gastrointestinal bleeding or splenomegaly as features of EHPVO, and at a mean age of 36 years old, the same age as our patient.14
In this case the suspicion of biliary obstruction elicited by appropriate clinical signs and symptoms, biochemical abnormalities and abdominal ultrasonography findings justified obtaining a CT scan than in its turn diagnosed portal cavernoma as the cause of jaundice and associated biliary calculi which further drove testing and therapy.
ERCP has been the traditional method of investigating PHB and was pivotal in the recognition of this condition. Several characteristic findings have been described and include smooth strictures of variable lengths, degrees and number, saccular dilations, indentations, dilated intrahepatic bile ducts, as well as filling defects mainly in the common bile duct that may represent calculi or varices.14,15 While its diagnostic use has been hindered by the availability of non-invasive and equally accurate alternatives, ERCP still has a major role when therapy is anticipated.
With magnetic resonance it is now possible to couple cholangiography and portography thus allowing the evaluation of all components of PHB with a single noninvasive test.4 Since several studies corroborate that magnetic resonance cholangiography has a similar sensitivity to ERCP in this setting, it has become the first line imaging test in this condition.16
Endoscopic ultrasonography does not yet have a defined role in PHB and its use is limited to the cases where other imaging tests are unable to give a clear answer, namely in the differential diagnosis of common bile duct stones, calculi or tumors.17
Therapy is currently not recommend for asymptomatic individuals with normal liver function tests. However, patients presenting with symptoms require an integrated management addressing not only biliary obstruction but also portal hypertension. Endoscopic treatment is the therapy of choice when there is choledocholithiasis, acute cholangitis or if shunt surgery is not possible.3,18–21 ERCP is usually effective in stone extraction and treatment of dominant strictures.3,14,18 However, the relief of biliary obstruction with balloon dilation and stenting is only a temporary measure and mandates the construction of a portosystemic venous shunt or regular sessions of endotherapy since stents tend to become clogged over time.14 Increased risk of bleeding is also an issue due to presence of venous collaterals.22
Patients that have a shuntable vein should be offered portosystemic shunt surgery since this procedure effectively addresses portal hypertension and may be the only treatment needed for dominant biliary strictures.23–25 Transjugular intrahepatic portosystemic shunt may be a valid alternative, albeit with less supporting evidence, and may be considered in selected cases when surgery is not feasible or is declined.3 In some cases additional biliary bypass surgery or cholecystectomy may be required.
Since our patient exhibited biliary stones in association with PHB she was initially managed endoscopically with great success and is now awaiting shunt surgery without any symptoms. The need for an effective management of portal hypertension in this patients, even when jaundice has resolved, is emphasized by the diagnosis of secondary biliary cirrhosis and liver dysfunction in patients with longstanding and untreated PHB.16,18
In summary, PHB is an uncommon entity that seldom causes symptoms. However, when symptomatic, the management must be tailored individually and should include shunt surgery. Magnetic resonance is the imaging modality of choice and ERCP is very useful when biliary stones, acute cholangitis or contraindications for surgery are present.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestThe authors declare that there are no conflicts of interest.