There is no consensus on the timing and management of emergency overt obscure gastrointestinal bleeding. Emergency capsule endoscopy and balloon-assisted enteroscopy have a high diagnostic and therapeutic yield in these situations. Most lesions detected by small bowel endoscopy are amenable to endoscopic haemostasis, although some lesions still require surgery or interventional radiology. The management of these patients is varied, and doubt persists about which technique should be preferred as first-line treatment. This narrative review analyses the usefulness and impact of small bowel endoscopic techniques in the emergency setting for severe overt obscure gastrointestinal bleeding.
Não existe consenso sobre a melhor estratégia e respetivos tempos na abordagem urgente da hemorragia digestiva obscura manifesta. A cápsula endoscópica e a enteroscopia assistida por balão de urgência têm elevada rentabilidade diagnóstica e terapêutica nesta indicação. A maioria das lesões detetadas na endoscopia do intestino delgado são passíveis de hemostase endoscópica, apesar de algumas ainda necessitarem de tratamento cirúrgico ou de técnicas de radiologia de intervenção. A abordagem destes pacientes é variada e persistem dúvidas sobre qual deverá ser a técnica de primeira linha. Este artigo de revisão analisa a utilidade e o impacto das técnicas endoscópicas do intestino delgado em contexto urgente na abordagem da hemorragia digestiva obscura manifesta severa.
The small bowel (SB) is unreachable by conventional flexible endoscopy, except for the duodenum and terminal ileum by upper endoscopy and colonoscopy, respectively. Emergency clinical situations that may require SB endoscopy mainly arise from acute SB bleeding, but other possible indications include foreign body removal or SB stenosis, which is manageable with balloon dilation or stent placement.
SB bleeding originating between the papilla and the ileocaecal valve is referred to as mid-gastrointestinal bleeding (MGIB). This concept overlaps with obscure-gastrointestinal bleeding (OGIB) of unknown origin. OGIB is categorized in occult-OGIB, defined by recurrent iron-deficiency anaemia and/or recurrent positive faecal blood tests; overt-OGIB (OOGIB) is defined by a persistent or recurrent exteriorization of melena or haematochezia after negative upper endoscopy, colonoscopy and other radiological examinations. The proportion of overt and occult forms varies in the different series to date but the most common presentation is occult-OGIB. However, emergency procedures in on-going OOGIB are rare, accounting for 1.79%–28.3%1–4 of all patients reported. Most studies to date concerning emergency SB endoscopy have been retrospective series with a small number of patients and a few prospective randomized controlled trials. In addition, the concept of “emergency OGIB” is not consistent among different authors.
The emergence of two recent techniques – capsule endoscopy (CE) and device-assisted enteroscopy (DAE), fundamentally balloon-assisted enteroscopy (BAE) – have enabled us to study the source of MGIB, improving the management of SB diseases.
CE is recognized to have a role as a first-line procedure in non-massive OGIB patients, guiding the insertion route for further endoscopic approaches by BAE when needed, such as for biopsy sampling or therapeutic procedures. BAE, by oral and/or anal routes, may be guided by CE as well as by radiological techniques. BAE can be performed using two systems: double or single balloon enteroscopy (DBE, SBE). The length of the working channel is similar, approximately 2000mm, but the channel diameter and insertion technique differ according to the type of enteroscope.5 Thus, the choice of an enteroscope should be based on the location and nature of the lesion and its availability. For example, a big channel enteroscope (with 3.2mm diameter) (double balloon enteroscope EN 580T, Fuji Film, Japan) may be required to allow a greater amount of aspiration volume (blood, air, CO2) and to pass accessories such as clips through more easily. Although a diagnostic enteroscope with a 2.2mm channel (double balloon enteroscope EN 450P5, Fuji Film, Japan), could provide greater insertion depth if adhesions are encountered, it is limited by its channel, which does not allow passage of clips or conventional argon proves and injection needles (1.8mm diameter accessories are required). These accessories sometimes are difficult to pass until reaching the SB lumen. Using a double balloon colonoscope (EN 450 P5, Fuji Film, Japan) by the oral route can be a good choice if lesions are in the proximal jejunum because it has an acceptable channel (2.8mm diameter) with a shorter length (1520mm), which allows the passage of conventional accessories more easily. The therapeutic enteroscopes 2.8mm and 2000mm in length are, however, the standard instruments (single balloon enteroscope SIF Q180, Olympus, Japan and double balloon enteroscope EN 450 T5, Fuji Film, Japan).
Although there is a well-established management algorithm in OGIB patients, there is no consensus on the timing of emergency endoscopy procedures in severe acute cases. Emergency management of patients with OOGIB is particularly challenging. Furthermore, patients presenting with acute OOGIB require a specific decision making strategy to perform an emergency endoscopic technique, surgery or interventional radiology. This decision may be difficult and is mainly based on the local experience and resources but also on the availability of skilled endoscopists at the moment of presentation as well as individual patient characteristics. In this sense, local emergency protocols may be crucial to quickly identify these selected patients and choose the best approach in each case. Specific healthcare circuits in small bowel endoscopy units experience challenges in terms of staff and endoscopic resources when quick management of these patients is necessary.
BAE not preceded by CE or angiography have been proposed as first-line procedures for those patients who present with massive bleeding. The oral insertion route is generally preferable when flexible enteroscopy is elected.6,7 However, other studies have reported that emergency CE is a feasible technique that may have higher diagnosis yields than angiography.8 The European Society of Gastrointestinal Endoscopy (ESGE) suggests that emergency CE and DAE should be considered equally in these patients.9 In addition, emergency CE has been reported to be a useful procedure in patients with severe acute GI bleeding after negative upper endoscopy without a previous colonoscopy.10
The goal of this review is to assess the usefulness of SB endoscopic techniques in the emergency setting of acute OGIB.
2ConceptsThere is no consensus regarding timing in emergency SB procedures for OGIB. Emergency DAE has been defined by different authors as performance within 24–72h of clinical presentation.3,11 Severe OOGIB has been widely described as that occurring with haemodynamic instability and transfusion requirements.
Concerning emergency CE performed in severe OOGIB cases, the time interval between admission/clinical presentation and CE administration ranges from 24h to 4.1 days.2,12 Most studies to date considered image reading and interpretation performed 12–24h after the completion of the procedure and imaging.
It is important to note that the comparability among the different studies may be influenced by many prognostic factors. The shorter the time interval between the last episode of on-going/active severe OGIB and the endoscopic examination, the higher the DAE/CE diagnostic yields.13–15 In addition, the bleeding severity and previous transfusion requirements may influence results.16
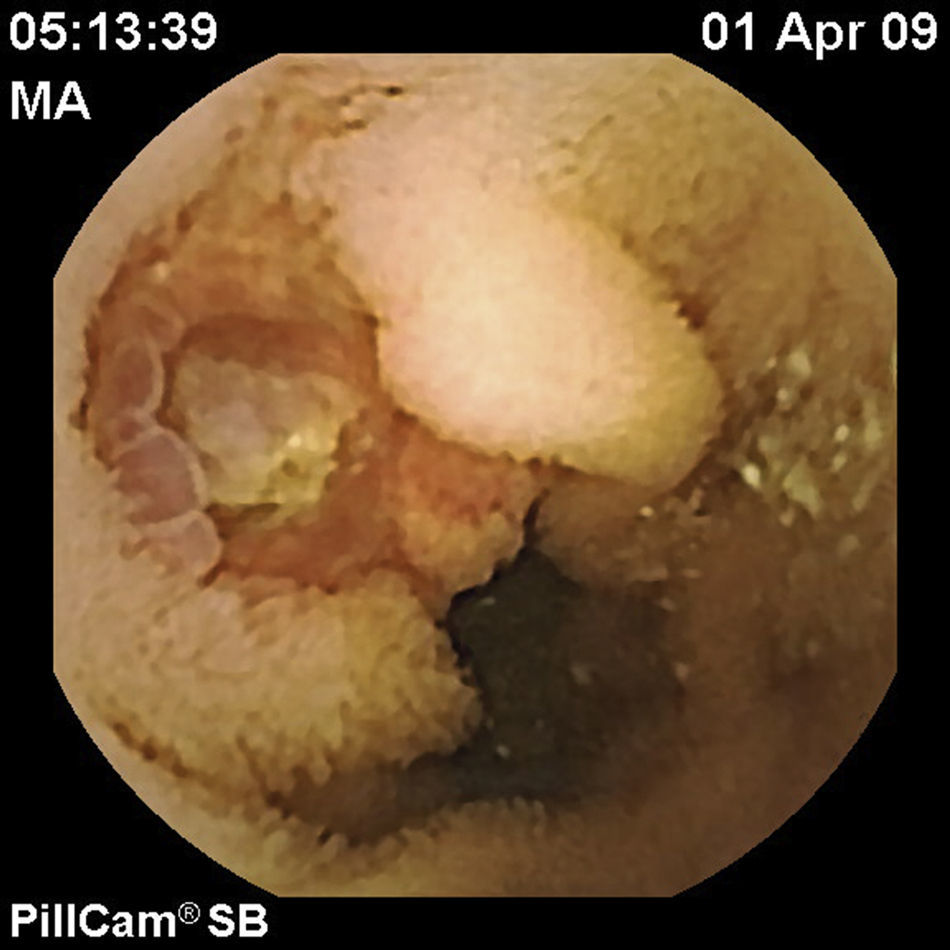
3Emergency capsule endoscopyCE has a controversial role in the emergency setting because it lacks therapeutic capabilities. It is known that the diagnostic yield of CE increases in patients with acute overt OGIB (Fig. 1) when it is performed closer to the bleeding episode.17 Hartmann et al.,18 in a prospective German study of 47 patients, reported that the diagnostic yield for positive findings in on-going OOGIB, previous-overt OGIB and occult OGIB were 100%, 67% and 67%, respectively, whereas Ribeiro et al.,19 in a retrospective study of 203 patients, reported diagnostic yields of 93%, 46.8% and 31.2%, respectively. According to Singh et al.,20 early deployment of CE within 3 days of admission results in a higher diagnostic yield and therapeutic intervention rate and an associated reduction of length of stay. Moreover, emergency CE has been found to achieve higher diagnostic yields and comparable long-term outcomes when compared with angiography.8
The lesion-specific diagnostic yield for emergency CE reported by different authors ranged between 60 and 73.3%, with only fresh blood without identifiable lesions detected in 6.7–27% of cases.2,11,12 Vascular lesions are the most common finding but ulcers and tumours (Fig. 2) have also been reported. It is interesting to note that CE may also detect factors responsible for the bleeding event outside the SB, notably colonic lesions, with the resulting optimization of resources and management of these patients who will avoid BAE. Notably, the false positive CE rate may be much lower in an emergency setting.
However, the main aim of CE should be to guide further management and approach, in addition to accurately diagnosing the culprit lesion. In this sense, real-time viewing by CE has been reported to be a useful approach in emergency OOGIB, providing the endoscopic approach21 and even modifying the initial route of DBE based on only clinical data in 25% of cases.22 Different CE systems allow real time viewing of images (PillCam, Covidien plc, Dublin, Ireland; Endocapsule, Olympus Optical Co, Tokyo, Japan; Miro-Cam, IntroMedic, Seoul, Korea; and OMOM capsule, Jinshan Science and Technology Group, Chongqing, China). A period of 100–150min after passing the pylorus appears to reliably indicate an oral route of insertion if the bleeding is detected in this time frame by the real-time viewer. In addition, this device can be used at the same time as the BAE is performed, therefore reducing the time from CE to BAE.
In a 3-year retrospective study, Almeida et al.2 reported 15 patients presenting with severe OOGIB and CE enabled accurate lesion detection and location, contributing to subsequent specific therapeutic measures in 73.3% of the cases. Specific diagnostic and therapeutic procedures were undertaken in 78% of patients (endoscopy: 54%, surgery: 22%, radiology: 2%) in the study by Lecleire et al.12
4Emergency device-assisted enteroscopyDAE includes DBE, SBE, spiral enteroscopy, and balloon-guided endoscopy. Most data to date concerning emergency DAE reported BAE (DBE, SBE); therefore, we mainly analyzed these two procedures.
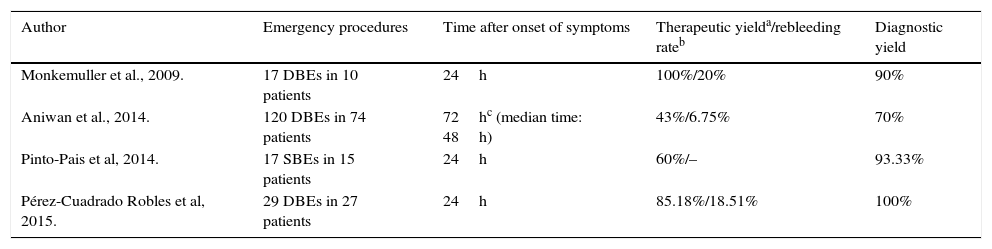
As for CE, the diagnosis yield of BAE in acute OOGIB has been reported to be higher than previous-OGIB or occult GI bleeding. Mönkemüller et al.3 described in a retrospective series a total of 17 emergency DBEs for OOGIB carried out in ten patients. The final diagnoses were two actively bleeding Dieulafoy lesions (22.2%), four bleeding tumours (44.4%), two vascular lesions (22.2%), two ulcers (22.2%) and one patient without an endoscopic diagnosis. Pinto-Pais et al.4 analyzed the impact of emergency SBE on OGIB in 15 patients who underwent 17 procedures with a therapeutic yield of 60% in active overt OGIB (Table 1). The bleeding source was detected in most of cases (93.3%): angioectasia (n=5, 35.7%), ulcers/erosions (n=3, 21.4%), bleeding tumours (n=4, 28.6%) and eroded polyps (n=2, 14.3%). Another study22 reporting 27 patients with overt severe bleeding who underwent 29 emergency DBEs achieved a diagnostic yield of 100%. Patients were diagnosed with the following: Dieulafoy's lesion (n=11, 40.7%), angioectasia (n=7, 25.9%), tumours (n=4, 14.8%), diverticulum (n=3, 11.1%) and ulcers (n=2, 7.4%).
Emergency Balloon-assisted endoscopy in small bowel bleeding.
| Author | Emergency procedures | Time after onset of symptoms | Therapeutic yielda/rebleeding rateb | Diagnostic yield |
|---|---|---|---|---|
| Monkemuller et al., 2009. | 17 DBEs in 10 patients | 24h | 100%/20% | 90% |
| Aniwan et al., 2014. | 120 DBEs in 74 patients | 72hc (median time: 48h) | 43%/6.75% | 70% |
| Pinto-Pais et al, 2014. | 17 SBEs in 15 patients | 24h | 60%/– | 93.33% |
| Pérez-Cuadrado Robles et al, 2015. | 29 DBEs in 27 patients | 24h | 85.18%/18.51% | 100% |
DBE, double-balloon enteroscopy, SBE, single-balloon enteroscopy.
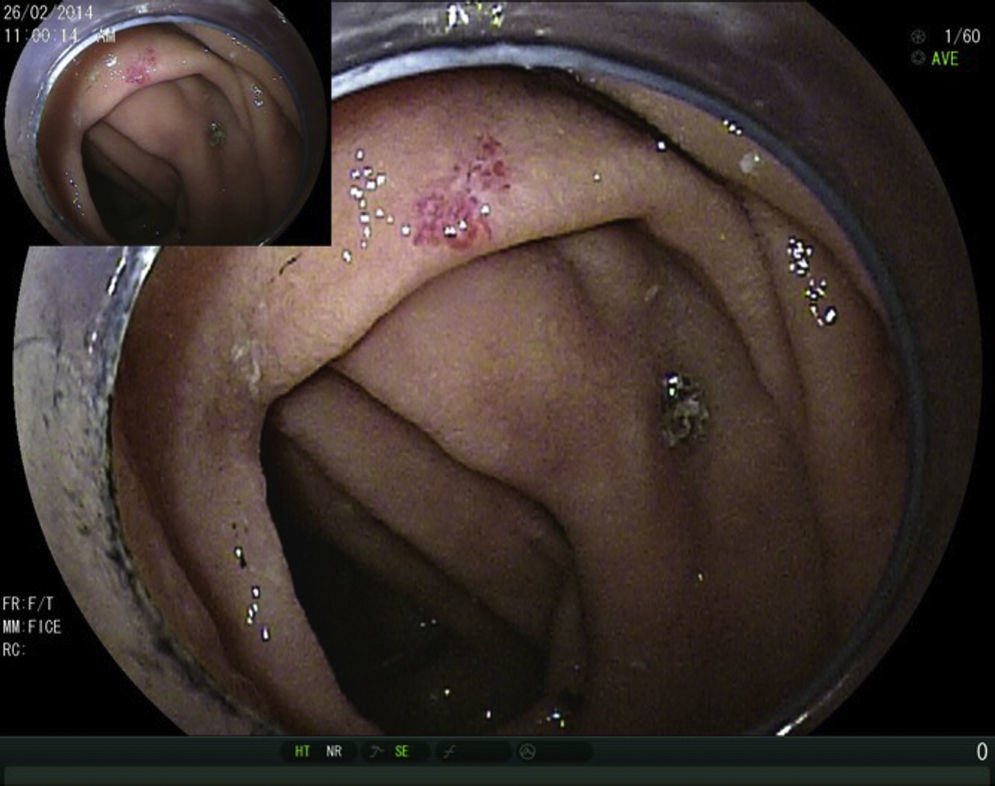
The endoscopic approach was mainly based on clinical data such as stool characteristics and previous endoscopic procedures performed in previous episodes in case of recurrent bleeding. Emergency CE and real-time viewing by CE were also considered in some cases. The most common lesion location was the proximal SB (jejunum). Most lesions reported in the studies to date were amenable to endoscopic treatment, and the most frequent bleeding source was a vascular lesion. In addition, many patients required several procedures and/or multiple haemostatic therapies to definitely stop the bleeding, especially for angioectasia and Dieulafoy's lesion. The current trend for BAE treatment is to use a mixed method (injection and thermal or injection and mechanical treatment) in case of vascular lesions and aggressive treatment, particularly in Dieulafoy's lesion because of high re-bleeding risk. A cap-assisted enteroscopy (Fig. 3) may be useful because the cap improves the visualization in case the lesion is located behind a fold or angled loop and the cap facilitates and stabilizes the rapprochement to the lesion if therapy is required. In addition, the cap allows the aspiration of a lesion internally for certain therapeutics, such as the endoloop.
CO2 insufflation instead of room air is also recommended because of its benefits in depth of insertion and in the amount of residual gas retention (it is an interesting aspect of long-lasting BAE as may occur in mid-bleeding indications).
Therefore, vascular lesions deserve special consideration. These patients usually have recurrent GI bleeding with a history of many endoscopic procedures previously performed,23 including false-negative BAE and/or CE because the intermittent bleeding characteristics of these lesions may hinder the diagnosis. Aniwan et al.11 categorized patients in emergency and non-emergency DBE, considering previous OOGIB and on-going OOGIB as previously described.24 In this study, vascular lesions (24% vs. 9%, p<0.05) and tumours were diagnosed more frequently in the emergency DBE group with a global re-bleeding rate of 10%.
Dulic-Lakovic et al.,25 in a multicentre retrospective study involving 284 patients, reported that in 10 cases of Dieulafoy's lesion with active bleeding, initial endoscopic haemostasis was successful, but the re-bleeding rate was 20%, and one surgical intervention was necessary. It is interesting to note that, in these two studies reporting 21 Dieulafoy's lesions, more than one BAE was required for diagnosis and/or treatment in many cases, and the vascular lesion was mainly located in the proximal jejunum, but they have also been described in the distal ileum.26 Thus, endoscopic haemostasis should preferentially use combined methods in these cases, and the oral route should be considered first if this entity is suspected. In SB tumours, BAE has been reported to be useful to plan further management including surgery through tattooing and tissue sampling, even in emergency cases.27
In general, most lesions found by emergency BAE are amenable to endoscopic haemostasis, and the therapeutic yield of DAE in the emergency setting is high within different studies. However, some patients with vascular lesions and particularly Dieulafoy's lesions may require several BAEs to stop the bleeding.
Intraoperative enteroscopy may also be an option in some cases with a high diagnostic yield (94%) and enabling endoscopic and/or surgical treatment (77.8%). However, this is an invasive procedure with non-negligible morbidity and mortality rates. In addition, the re-bleeding rate (21.4%) was similar to that of patients with vascular lesions not submitted to this type of invasive approach, as reported in other studies. Therefore, this approach should only be considered in specific cases after multidisciplinary evaluation.28
5DiscussionThe present review analyzed the various management methods of severe OOGIB by emergency SB endoscopy. As a rule, CE is recommended as the first-line investigation in patients presenting with OGIB.6,9 In case of non-massive OOGIB, CE should be performed as soon as possible after the bleeding episode – optimally within 14 days – to maximize the diagnostic yield. A routine performance of second-look endoscopy prior to CE is not recommended, but this should be decided on a case-by-case basis. After positive CE, BAE has been reported to have a higher diagnostic yield and should be indicated29 in emergency and non-emergency cases. However, there is no consensus on timing and management in severe OOGIB with different studies reporting different approaches and recommendations.
The burning question is which technique to choose as the first-line procedure in each case. There is no probable general answer to this question. In patients with significant active SB bleeding and unsuitable for flexible endoscopy, computed tomography (CT)-angiography or angiography may also be considered.9 Recently, the American College of Gastroenterology guidelines30 strongly recommended angiography and CT scan as first-line procedures in unstable and stable patients presenting with massive OOGIB, respectively.
Regarding emergency CE and BAE management, most studies to date agree on the high diagnostic yield and increased therapeutic options compared to non-emergency procedures. The accurate and quick management by an expert endoscopist, either performing first-line BAE or preceded by CE, appears to be a key point in these patients. No evidence of the superiority of one over the other in the initial management has been found,1 although there are specific cases that can benefit more from each technique. It makes sense to perform BAE initially in cases of previous OOGIB with a known bleeding source location (for example, previous CE reporting the location of vascular lesions or the level of the bleeding in recurrent patients), but its use in the emergency setting is still uncommon.31 In addition, emergency BAE should be preferred in patients with surgically altered anatomy.32 CE may not be able to explore the whole length of the SB in some cases, as in patients with concomitant intestinal obstruction and haemorrhage.
In circumstances in which there is a very high risk of deep sedation, CE may be considered initially, especially if real-time viewing is available. This device might modify the endoscopic approach and outcome in up to 25% of cases.22 Notably, both techniques may overlap in time, especially if CE detects a proximal bleeding source accessible by oral BAE. Endoscopic CE placement in the duodenum should also be considered to save time.
Emergency SB endoscopy is clinically required for severe but selected cases.2,10 After stabilization of the patient, the timing to perform emergency BAE may be crucial. First, it is very important to individually assess the severity of the patient, considering transfusion requirements, recurrent bleeding and procedures already performed. It is important to analyze the clinical presentation, current medical therapy (anticoagulants, antithrombotic, NSAIDs), personal/family history or any factor that may guide the clinical suspicion of specific SB lesions. Vascular lesions such as angioectasia or Dieulafoy's lesion may cause severe self-limited intermittent OOGIB, which may improve even with conservative management. In these cases, to keep the urgent indication or delay further procedures until complete resolution of the bleeding episode should be discussed by a multidisciplinary team. A SB endoscopy second look can be performed with CE after deep enteroscopy to confirm bleeding cessation (Fig. 4). Emergency BAE has also shown to be useful in SB lesions not amenable to endoscopic haemostasis, such as large bleeding SB tumours. Tattoo injection at the bleeding source and histological sampling when possible may be performed systematically to guide further management.
Thus, in most cases, both techniques (CE and BAE) might be performed first, with the final decision based on local experience and availability. In this sense, a flexible local protocol for severe OOGIB is needed to optimize the emergency management of these patients, taking into consideration the need of overtime working hours. Moreover, these patients may consume many diagnostic and therapeutic resources, including transfusions and long hospital stays, and have high morbidity and mortality. Prospective studies with longer follow-up are needed to compare the impact of both techniques on patient outcomes.
In conclusion, emergency SB endoscopy (CE and BAE) is a safe technique in severe OOGIB, with high diagnostic and therapeutic yields. The choice of one over the other as first-line procedures should be based on local experience and patient characteristics, keeping in mind that the key point is quick management following the bleeding presentation to optimize and improve the outcome of these selected patients.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.