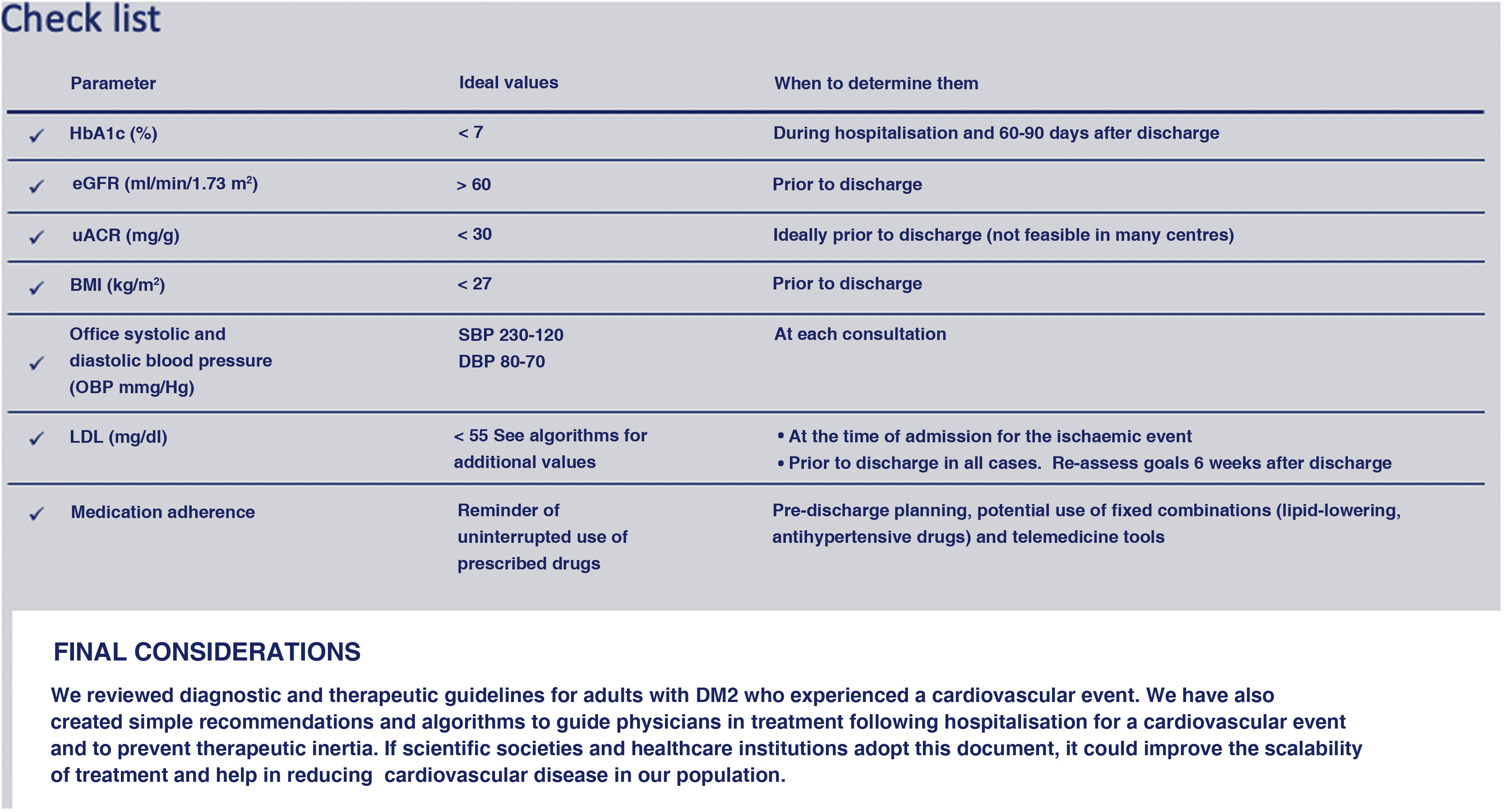
The document outlines recommendations for the management of patients with type 2 diabetes (T2D) at hospital discharge following an ischaemic cardiovascular event. Diabetes significantly increases the risk of cardiovascular events, and a high proportion of patients in coronary units have this condition. The discharge process is crucial for optimising treatments and reducing the risk of recurrent complications such as reinfarction, stroke, and hospitalisations for heart failure.
Strategies include rigorous control of lipid levels, recommending potent statins combined with ezetimibe and, if necessary, other drugs such as inclisiran, evolocumab, alirocumab, or bempedoic acid. Optimal antihypertensive treatment is also suggested as secondary prevention.
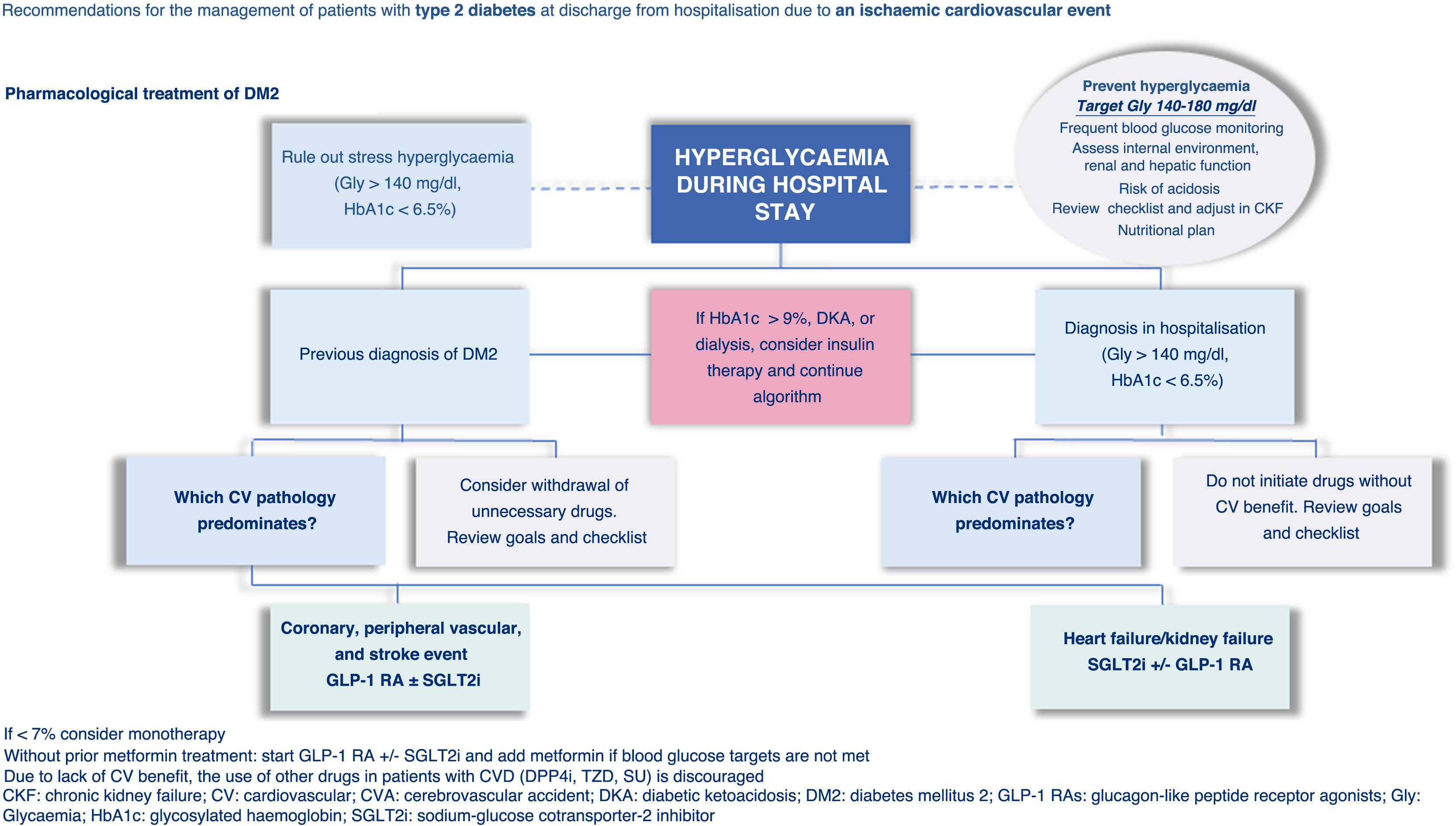
For patients already on insulin, it is essential to adjust the dosage when adding SGLT-2 inhibitors (SGLT2i) or GLP-1 receptor agonists (GLP-1RA) to avoid hypoglycaemia, with structured glucose monitoring. In cases where HbA1c is not available during hospitalisation, the algorithm guides treatment, highlighting that GLP-1RA and SGLT2i do not cause hypoglycaemia. The combination of these drugs is safe and effective, improving several cardiovascular risk factors.
The document emphasises the importance of education on nutrition and healthy habits, as well as the follow-up and adjustment of pharmacological treatments to achieve adequate metabolic control and reduce cardiovascular risks. Nutritional evaluation and control are essential, considering obesity as a critical factor in T2D and its association with the risk of recurrent cardiovascular events.
El documento aborda las recomendaciones para el manejo de los pacientes con diabetes mellitus tipo 2 (DM2) al egreso hospitalario tras un evento cardiovascular isquémico (considerando principalmente cardiopatía isquémica e ictus isquémico). La diabetes incrementa significativamente el riesgo de eventos cardiovasculares, y una alta proporción de pacientes en las unidades coronarias presenta esta condición. El proceso de alta es crucial para optimizar los tratamientos y reducir el riesgo de complicaciones recurrentes como reinfarto, accidente cerebrovascular y hospitalizaciones por insuficiencia cardiaca.
Las estrategias incluyen un control riguroso de los niveles lipídicos, recomendando estatinas potentes combinadas con ezetimiba y, si es necesario, otros fármacos como inclisirán, evolocumab, alirocumab o ácido bempedoico. También se sugiere el tratamiento antihipertensivo óptimo como prevención secundaria.
Para los pacientes que ya reciben insulina, es fundamental ajustar la dosis al agregar iSGLT-2 o arGLP-1 para evitar hipoglucemias, con un monitoreo estructurado de glucosa. En casos donde no se dispone de HbA1c durante la internación, el algoritmo guía el tratamiento, destacando que los arGLP-1 e iSGLT2 no causan hipoglucemia. La combinación de estos fármacos es segura y efectiva, mejorando varios factores de riesgo cardiovascular.
El documento enfatiza la importancia de la educación en nutrición y hábitos saludables, así como el seguimiento y ajuste de tratamientos farmacológicos para lograr un control metabólico adecuado y reducir riesgos cardiovasculares. La evaluación y control nutricional son esenciales, considerando la obesidad como un factor crítico en la DM2 y su asociación con el riesgo de eventos cardiovasculares recurrentes.
One in 8 adults in Argentina has type 2 diabetes mellitus (DM2).1 Diabetes increases the risk of cardiovascular (CV) events 1.7-fold.2 It is estimated that 3 out of every 10 people discharged from coronary units have diabetes3. There is an unmet need in the medical community for simple documents and algorithms to coordinate between inpatient and outpatient guidelines. The discharge process after an acute cardiac event is a window of opportunity for treatment optimisation, with a focus on reducing the risk of recurrent events or complications such as reinfarction, cerebrovascular accident (CVA), lower limb ischaemic event, hospitalisation for heart failure (HF), or CV death.
Therefore, we formed a group of experts to review the updated control and treatment criteria for people with DM2 and established CVD, covering general goals of metabolic control, hypertension, and dyslipidaemia.
Diagnosis of DM2 and differential diagnosesThe prevalence of hyperglycaemia is close to 40% in patients with coronary events during hospitalisation, which is an independent marker of mortality. This is directly related to short- and long-term outcomes, and to increased healthcare costs.4–10 It is important to determine whether hyperglycaemia (defined as fasting plasma glucose (FPG) >140mg/dl or a random level >180mg/dl) corresponds to known diabetes mellitus (DM), previously undiagnosed DM, or stress hyperglycaemia. It is recommended to order an HbA1c test to make this differential diagnosis. Also, regardless of diagnosis, the recommended blood glucose level for hospitalised patients is 140-180mg/dl.4–10
- a.
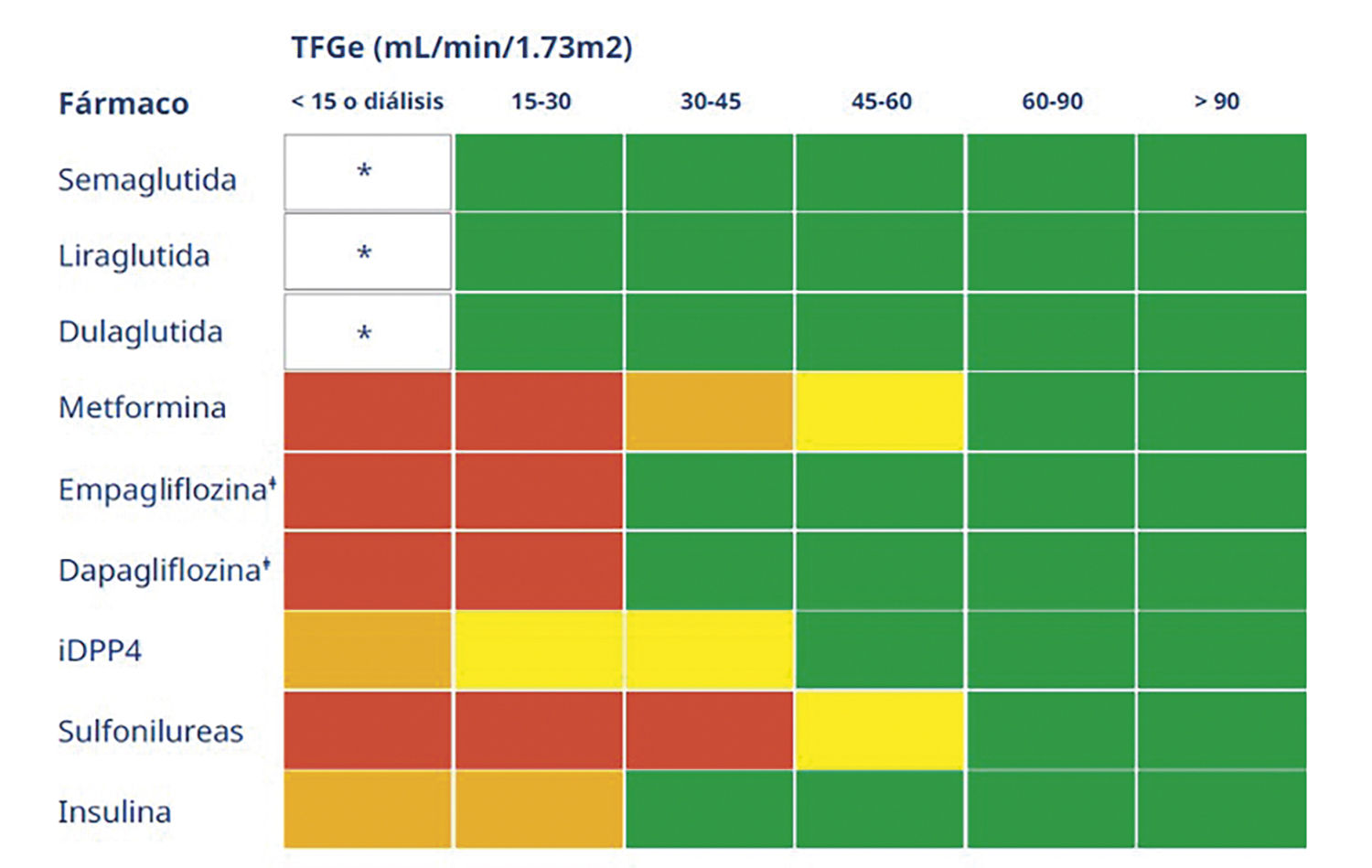
Previously known DM2: Act according to institutional protocol. It is recommended to adjust insulin therapy and withdraw oral hypoglycaemic agents (sulfonylureas, meglitinides) to reduce the risk of hypoglycaemia. Caution with drugs with adjusted doses according to glomerular filtration rate (Table 1) or with adverse CV effects (saxagliptin, rosiglitazone). Consider continuing GLP-1 receptor agonists (GLP-1 RAs) and/or SGLT-2 inhibitors (SGLT2i) according to clinical status and criteria (Fig. 1).
Table 1.Indication for drugs for DM2 according to glomerular filtration rate28,29
* Limited data on eGFR<15.28,29
¿ Bear in mind that the efficacy in the glycaemic control of SGLT2is declines in correlation to the fall in glomerular filtration rate estimated from 45ml/min.
Source: 2022 KDIGO Guideline: https://www.kidney-international.org/issue/S0085253822X00021?dgcid=raven_jbs_etoc_email.
Figure 1.Recommendations for the management of DM2 during hospital stay and at discharge. If HbA1c <7% consider monotherapy. Without prior treatment with metformin: start GLP-1 RA ± SGLT2i and add metformin if glycaemic targets are not achieved. Due to the lack of CV benefit, the use of other drugs in patients with CVD (DPP4i, TZD, SU) is discouraged. CKF: chronic kidney failure; CVA: cerebrovascular accident; CV: cardiovascular; DKA, diabetic ketoacidosis; DM2: diabetes mellitus 2; GLP-1 RAs: Glucagon-like peptide-1 receptor agonists; Gly: glycaemia; HbA1c: glycosylated haemoglobin; SGLT2i: sodium-glucose cotransporter-2 inhibitor.
(0.6MB). - b.
Newly diagnosed DM2: (HbA1c >6.5%). It is recommended to follow institutional insulin therapy protocols, preventing hypoglycaemia. The addition of other DM2 drugs during hospitalisation should be analysed on an individual basis. GLP-1 RAs and/or SGLT2i at discharge should be started according to the algorithm.
- c.
Stress hyperglycaemia: (HbA1c <6.5%). These patients do NOT have DM2, they have high vulnerability to hypoglycaemia (caution with starting insulin therapy). Recategorize the case 30-60 days after discharge, using an oral glucose tolerance test and HbA1c test.
Note: Repeat HbA1c measurements are not recommended for inpatient follow-up.
Inpatient glycaemic management4–10Perform capillary controls frequently, 4 to 5 times per day, to adjust the insulin therapy protocol. In any case, their frequency should be determined on an individual basis:
- a.
Perform an exhaustive control of the internal environment. In cases of stress hyperglycaemia, rule out acute complications such as diabetic ketoacidosis or non-ketotic hyperosmolar coma.
- b.
Prevent hypoglycaemia. The most predisposed populations are:
- •
Age >65 years
- •
Long disease course
- •
eGFR<45ml/min
- •
Cognitive impairment
- •
Previous CVD
- •
Visceral neuropathy
- •
- c.
In patients with controlled clinical situations, low risk, and low probability of hypoglycaemia, a lower target of between 100-140mg/dl is advised.
- d.
In patients with DM1 or DM2 with highly variable intensified schemes, hyperglycaemia secondary to corticosteroids or associated with parenteral nutrition, it may be necessary to use a continuous subcutaneous glucose monitor.
- a.
Evaluate the attached algorithm (Fig. 1).
- b.
After discharge, ensure referral to a physician for DM2 follow-up within 7 to 30 days.
- c.
The following should be considered in the hospital discharge process:
- 1.
Internal environment and renal function: adjust treatments dynamically (Table 1).
- 2.
Type of CV event.
- 3.
Hepatic and renal function and risk of acidosis (determinants for metformin use). If the patient was on metformin treatment and at low risk of acidosis, they can continue. If additional glycaemic control is needed and not on metformin treatment, consider starting it.
- 4.
Do not initiate therapies with drugs with a higher risk of hypoglycaemia (sulfonylureas, meglitinides).
- 5.
Thiazolidinediones are not recommended until clinical picture stabilisation and multidisciplinary evaluation.
- 6.
In patients with HbA1c >9% titrate insulin therapy with patient education on appropriate use and management of hypoglycaemia. Prefer insulin analogues with low risk for hypoglycaemia (glargine, degludec).
- 7.
In insulinised patients, monitoring is recommended within 72h/7 days of discharge (face-to-face or telemedicine), evaluate institutional protocols, and consult with diabetes team.
- 1.
- d.
It is advisable to send the patient for whom clinical analysis has been ordered for control in the following 7 to 30 days (according to the type of event and clinical status at discharge).
- e.
It is important that the patient with de novo DM2 who is discharged with insulin therapy has a capillary measurement system or continuous monitor, insulin for the first days, needles (32G, 4mm), and ensure that they have correct prescriptions for DM2 drugs.
- f.
Nutritional evaluation and control are recommended; obesity is one of the underlying causes of DM2 and is associated with an additional increased risk of recurrent CV events.11,12 It is recommended that BMI (height/weight2), cervical circumference, and waist-hip ratio are determined and recorded prior to discharge: in order to set outpatient treatment goals.
- g.
Set nutrition and physical activity guidelines prior to discharge, which should be individualised according to the type of CV event, haemodynamic status, degree of obesity, and concomitant diseases.13 Consider referral to specialists and assess drugs to treat DM2, combined with weight reduction and CV safety.
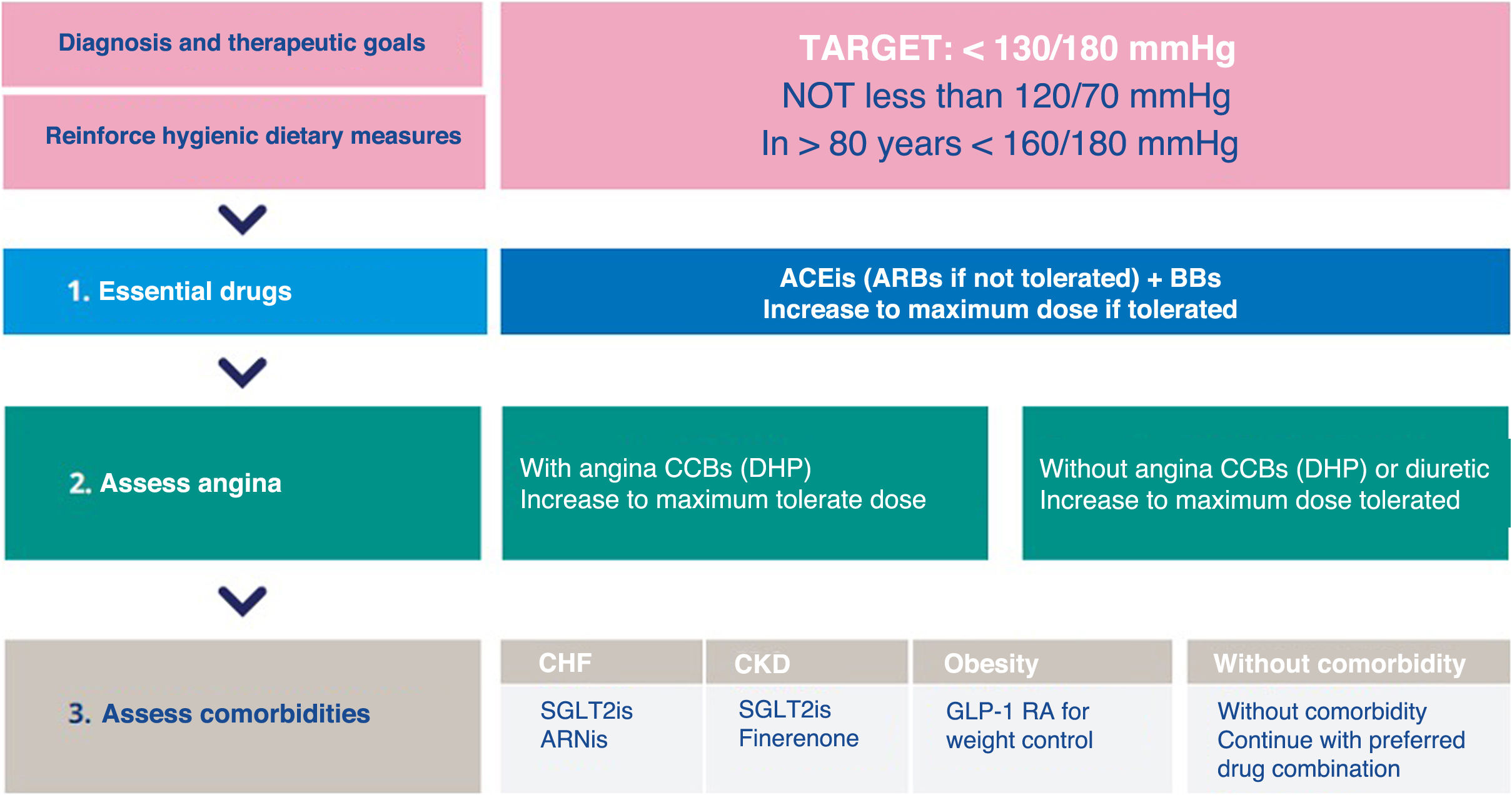
There is overwhelming evidence to support the benefits of blood pressure (BP) reduction in people with hypertension (HT) and DM2, both in reducing macrovascular events and mortality, and in preventing microvascular complications, such as nephropathy and retinopathy14:
- a.
Drug treatment should be initiated when systolic BP is ≥140mmHg or diastolic BP is ≥90mmHg, to reach, if well tolerated, a target of <130/80mmHg (not <120mmHg). These values have been shown to offer incremental protection, compared with higher BP readings, particularly against stroke. This recommendation extends to a diastolic BP <80mmHg, but not lower than 70mmHg. The presence of ischaemic vascular disease places the patient at very high CV risk. Although international guidelines recommend starting antihypertensive treatment at readings ≥130/80mmHg, the Argentine consensus recommends doing so at readings above 140/90mmHg.
- b.
Consider that patients with chronic atherosclerotic disease (CAD) are almost invariably under treatment with BP-lowering drugs, such as renin angiotensin aldosterone system agents (RAAS), beta-blockers (BBs), or calcium channel blockers (DHP-CCBs and non-DHP-CCBs), which are part of the therapeutic strategy for this disease. Treatment should include a RAAS, to prevent the onset and progression of renal complications of diabetes more effectively than other antihypertensive drugs.
- c.
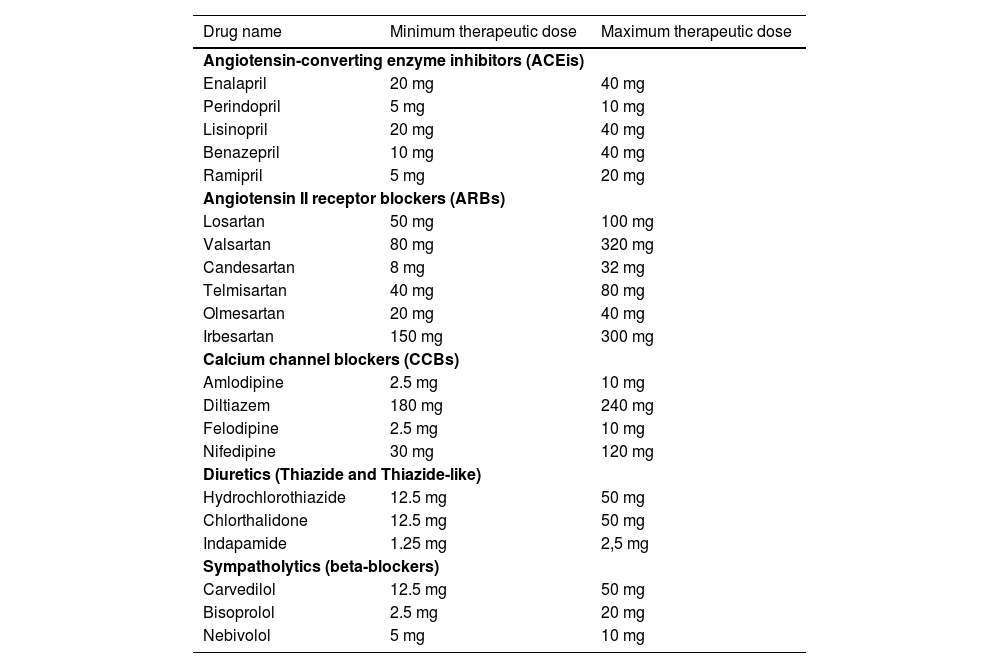
BBs, DHP-CCBs, and non-DHP CCBs are the drugs of choice to treat HTN in patients with symptomatic coronary artery disease and angina; if necessary, combination therapy with a DHP-CCB and a BB is recommended (e.g., after an infarction). In the context of stroke, prioritise CCBs15 (Table 2).
Table 2.Antihypertensive drugs in maximum and minimum doses.
Drug name Minimum therapeutic dose Maximum therapeutic dose Angiotensin-converting enzyme inhibitors (ACEis) Enalapril 20 mg 40 mg Perindopril 5 mg 10 mg Lisinopril 20 mg 40 mg Benazepril 10 mg 40 mg Ramipril 5 mg 20 mg Angiotensin II receptor blockers (ARBs) Losartan 50 mg 100 mg Valsartan 80 mg 320 mg Candesartan 8 mg 32 mg Telmisartan 40 mg 80 mg Olmesartan 20 mg 40 mg Irbesartan 150 mg 300 mg Calcium channel blockers (CCBs) Amlodipine 2.5 mg 10 mg Diltiazem 180 mg 240 mg Felodipine 2.5 mg 10 mg Nifedipine 30 mg 120 mg Diuretics (Thiazide and Thiazide-like) Hydrochlorothiazide 12.5 mg 50 mg Chlorthalidone 12.5 mg 50 mg Indapamide 1.25 mg 2,5 mg Sympatholytics (beta-blockers) Carvedilol 12.5 mg 50 mg Bisoprolol 2.5 mg 20 mg Nebivolol 5 mg 10 mg Source: Adapted from Kaplan's Clinical Hypertension, 11th edition.
- d.
The new antidiabetic agents: SGLT2is and GLP-1RAs, have been shown to reduce macrovascular and microvascular complications in DM2.16 GLP-1RAs have demonstrated a reduction in CV events and considerable weight loss.17 An important additional aspect of the action of these drugs is that they can significantly reduce blood pressure independently of the use of conventional antihypertensives.18,19 Therefore, both therapeutic classes may help to improve BP control, which is especially difficult in DM.
- e.
Positive results have recently been shown for finerenone (mineralocorticoid receptor antagonist) in patients with DM2 and chronic kidney disease. Although finerenone has significant benefits in reducing CV events and the progression of renal disease in patients with DM2 and CKD, its impact on BP is relatively small (Fig. 2).20
Figure 2.Recommendations for the management of HTN in patients with DM2 and a recent ischaemic CV event. ACEis: angiotensin-converting enzyme inhibitors; ARBs: angiotensin II receptor blockers; BBs: betablockers; CCBs: calcium channel blockers; CKF: chronic kidney failure; CHF: chronic heart failure; CV: cardiovascular; DHP, dihydropyridines; DM2: type 2 diabetes mellitus; HTN: hypertension.30
(0.3MB).
- a.
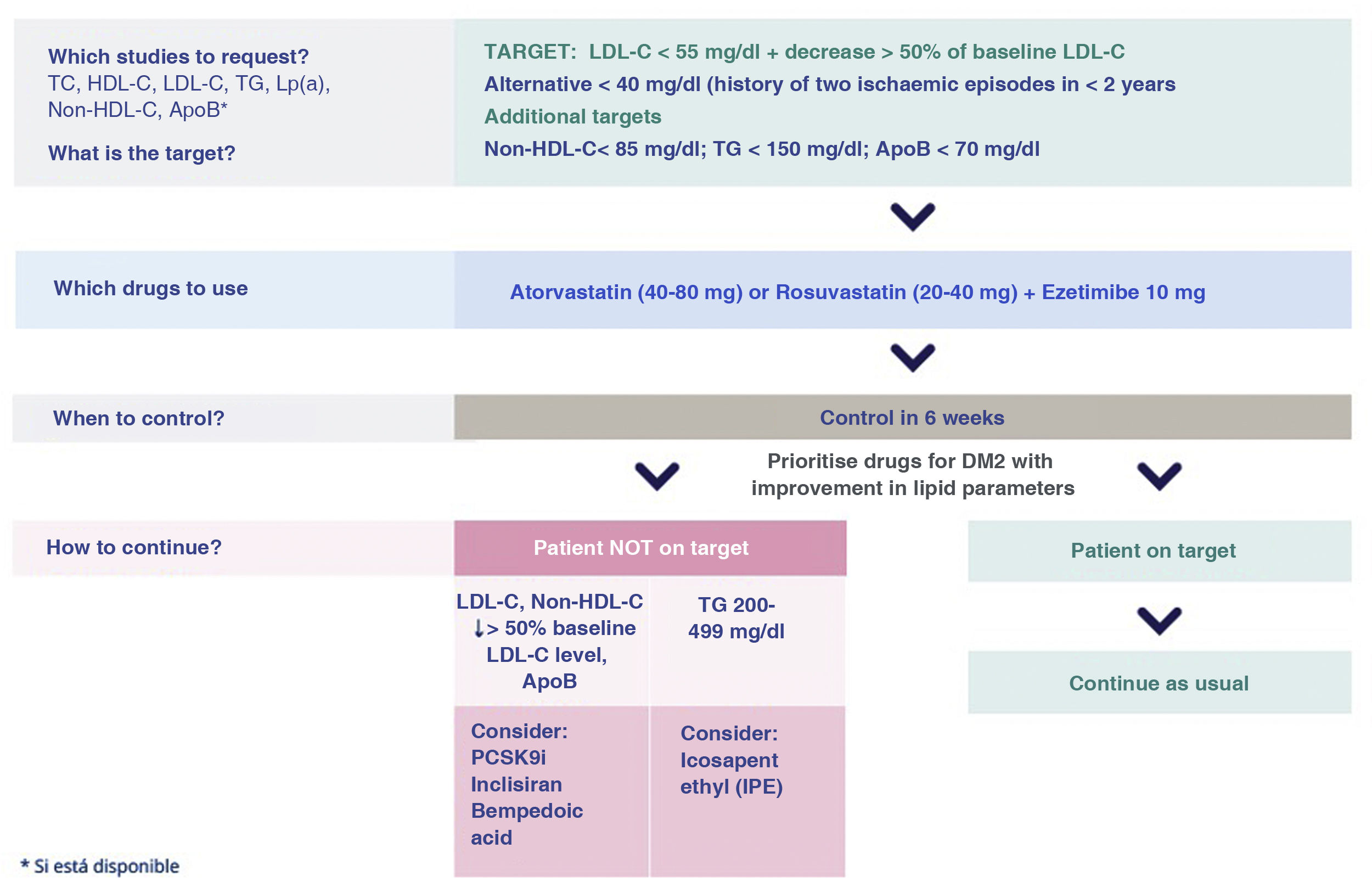
A vascular ischaemic event in patients with DM2 places them at “very high CV risk”.20,21 According to the different national and international treatment guidelines and recommendations, this group of patients has a target LDL cholesterol (LDL-C)<55mg/dl and should achieve a baseline LDL-C reduction of at least 50%.22
- b.
As additional targets, non-HDL cholesterol <85mg/dl, triglycerides <150mg/dl, and ApoB<70mg/dl need to be achieved.
- c.
In turn, based on evidence from recently published large studies, if the patient, who is on target lipids, has a history of 2 ischaemic CV events in a 2-year period, the recommendation is to lower LDL-C levels to <40mg/dl.23
- d.
The initial strategy is to combine high-dose, potent statins (atorvastatin 40-80mg or rosuvastatin 20-40mg) with ezetimibe 10mg to reduce baseline LDL-C levels by at least 60% and achieve the above-mentioned targets.
- e.
A target LDL-C target of less than 40mg/dL should be considered in patients who have had 2 ischaemic events (not necessarily in the same territory) within 2 years.
- f.
When the triglyceride value is between 200-500mg/dl, if the patient is at target LDL-C, consider adding omega-3 fatty acids (specifically purified eicosapentaenoic acid [IPA], icosapent ethyl).
- g.
Lipid levels should be monitored at 6 weeks and if targets are achieved, it is recommended to continue with the same therapeutic regimen (Fig. 3).
Figure 3.Recommendations for the management of dyslipidaemia in patients with DM2 and CV ischaemic event. #Existing evidence with GLP-1 RA.17 ApoB: apolipoprotein B; HDL-C: HDL cholesterol; LDL-C: LDL cholesterol; TC: total cholesterol; CV: cardiovascular; DM2: type 2 diabetes mellitus; Lp (a): lipoprotein a; Non-HDL-C: non-HDL-cholesterol; TG: triglycerides.24,25
(0.27MB).
- 1.
If the patient was already on insulin, what to do at discharge? If we add an SGLT2i or GLP-1RA to the treatment, it is important to reduce the total insulin dose by 20%-25%, especially if HbA1c is <7%, in order to prevent hypoglycaemia. Structured glucose monitoring by capillary monitoring or continuous interstitial sensor is necessary.26
- 2.
What if we do not have HbA1c during hospitalisation? The algorithm can be followed, remembering that GLP-1RA and SGLT2i do not cause hypoglycaemia. It is also recommended to re-categorise the case after discharge.
- 3.
Can iSGLT2 be combined with GLP-1 RA? Yes, they complement each other, and each has its own specific recommendations. Both groups of drugs reduce CV events. No significant adverse interactions or risk of hypoglycaemia have been reported with this combination. Both reduce CV risk factors: blood pressure, HbA1c, body weight, and have renal benefits.
- 4.
What is the dose titration of GLP-1RA? Slow escalation of doses has been associated with better gastrointestinal tolerance. Liraglutide, daily doses with weekly escalation. Semaglutide and dulaglutide, weekly doses with monthly escalation.
- 5.
What should I be aware of when starting GLP-1RA? The most frequently associated adverse events are gastrointestinal (GI) in nature and are characteristically transient and mild to moderate (nausea, vomiting, diarrhoea, and constipation). It is important to follow the titration suggested in the package leaflet. Food education and healthy habits are essential.27
- 6.
What should I bear in mind when starting SGLT2i? Caution due to volume depletion with diuretics (e.g. loop diuretics) and risk of genital infections in patients with predisposition and poor metabolic control (generally does not require discontinuation of the drug, only hygienic measures and standard treatment of mycosis, which should be assessed on an individual basis).
- 7.
Is it possible to combine DPP4i with GLP-1 RA? No. They should not be combined as DPP4i acts by increasing endogenous GLP1 levels without demonstrating additional benefits in reducing CV events.
- 8.
Are there any relevant drug interactions between DM2 drugs and CV drugs? No relevant interactions with antithrombotics, lipid-lowering drugs, hypertensive drugs, antianginal drugs, diuretics have been found. Caution when combining sulphonylureas with vitamin K antagonists and loop diuretics with SGLT2i.
- 1.
What are the potent statins and what dose is considered high? Atorvastatin 40-80mg or rosuvastatin 20-40mg.
- 2.
Which lipid-lowering combinations are considered safe and can be indicated at discharge? Dual therapies: Statins with ezetimibe, PCSK9i or inclisirane, bempedoic acid, icosapent ethyl. Triple therapies: Statins with ezetimibe and PCSK9i.
- 3.
Which lipid-lowering drug combinations are considered potentially risky? Statins with certain fibrates, such as gemfibrozil.
We have reviewed the diagnostic and therapeutic guidelines for adults with DM2 who have experienced a CV event. In addition, we have created simple recommendations and algorithms to guide clinicians in management after hospitalisation for a CV event and to prevent therapeutic inertia.
In patients who have suffered an ischaemic event, the administration of antiplatelet drugs at hospital discharge is crucial to prevent recurrences and CV complications. Antiplatelet agents such as aspirin or P2Y12 receptor inhibitors (clopidogrel, prasugrel, and ticagrelor) is recommended in appropriate doses according to international clinical guidelines and individual assessment of bleeding risk. In some cases, especially in the presence of atrial fibrillation or deep vein thrombosis, it may be necessary to add direct oral anticoagulants (DOACs) or vitamin K antagonists (warfarin, acenocoumarol), with strict monitoring of INR levels. It is essential to personalise treatment considering factors such as renal function, drug-drug interactions, and patient adherence.
Lifestyle interventions for diabetic patients are essential in secondary prevention to prevent or delay complications. A balanced diet is essential, recommending carbohydrate control, increased fibre intake and unsaturated fats (olive oil, avocado, nuts) over saturated and trans fats. Regular exercise, with at least 150min per week of moderate aerobic activity or 75min of vigorous activity, together with resistance training and flexibility activities such as yoga or tai chi, improves glycaemic control and reduces CV risk.
Stress management through relaxation techniques (meditation, deep breathing, yoga), cognitive behavioural therapy, and social support is crucial. Smoking cessation and reducing alcohol consumption are also important, with options such as nicotine replacement therapies, medications (bupropion, varenicline) and support programmes. These integrated and personalised interventions improve quality of life and prevent serious complications in diabetic patients29 (Fig. 4).
Societal endorsementsThese recommendations are endorsed by the Argentine Society of Arterial Hypertension and the Argentine Society of Lipids.
FundingThis document was funded by Novo Nordisk Pharma Argentina S.A. The authors take full responsibility for the content and conclusions expressed in this document.
Conflict of interestsThe authors have no conflict of interests to declare.
This paper was jointly developed by Hipertensión y Riesgo Vascular, Revista Argentina de Lípidos, Revista de la Federación Argentina de Cardiología and jointly published by Elsevier España S.L.U., Sociedad Argentina de Lípidos and Federación Argentina de Cardiología. The articles are identical except for minor stylistic and spelling differences in keeping with each journal's style. Either citation can be used when citing this article.