A longitudinal study was conducted to assess the presence of beliefs about symptoms related to hypertension and the time since diagnosis in which they appear. A randomly selected sample of hypertensive patients (67% women, mean age 53.27 years and range 20-65) was divided into four groups according to the time from diagnosis. All patients (N=171) were interviewed at the beginning (initial assessment) and 12 months later (final assessment) and the patients (n=75) who did not report beliefs about symptoms at the initial assessment were interviewed in a follow-up schedule. The results showed that 56% of patients reported beliefs about symptoms at the initial assessment, and this percentage increased to 77% at the final assessment (p < .001) finding significant differences between the two groups with a more recent diagnosis and the two groups of long-standing patients. Longitudinal analysis of the group with the recent diagnosis showed that the critical period for the emergence of beliefs was the first year from diagnosis. This period could be decisive in order to prevent them. Healthcare professionals should pay attention to the emergence of these beliefs, as they could negatively affect treatment adherence.
Se realizó un estudio para evaluar creencias sobre síntomas relacionados con la hipertensión y el tiempo transcurrido desde el diagnóstico. Una muestra elegida al azar de pacientes con hipertensión (media de edad 53,27 años, rango 20-65; 67% mujeres) se dividió en cuatro grupos de acuerdo al tiempo transcurrido desde el diagnóstico. Se entrevistó a todos los pacientes (N=171) al comienzo del estudio (evaluación inicial) y 12 meses después (evaluación final). A los pacientes que no informaron creencias en síntomas (n=75) se les entrevistó cada tres meses de acuerdo a un programa de seguimiento. Los resultados indicaron que en la evaluación inicial el 56% de los pacientes informó creencias en síntomas, elevándose al 77% en la evaluación final (p < .001), y diferencias significativas entre los grupos con menor y mayor tiempo desde el diagnóstico. El análisis longitudinal del grupo de pacientes de reciente diagnóstico mostró que el primer año es el período crítico para la emergencia de creencias en síntomas, información que resulta clave para planear la prevención. Los profesionales de la salud deberían prestar atención a la emergencia de creencias en síntomas dado que pueden afectar negativamente a la adherencia al tratamiento.
Arterial hypertension is one of the main risk factors for cardiovascular and cerebrovascular events and one of the main causes of death and disability in developed countries (Arrebola-Moreno et al., 2014; Lloyd-Jones et al., 2010; Sharp, Aarsland, Day, Sønnesyn, & Ballard, 2011). Arterial hypertension is defined as values >140mmHg of systolic blood pressure and/or >90mmHg of diastolic blood pressure (Mancia et al., 2013). Although effective treatment is available, a large number of studies show that treatment is poorly followed by hypertensive patients (Chobanian, 2009; Egan, Zhao, & Axon, 2010; Márquez, Granados, & Roales-Nieto, 2014; van Onzenoort et al., 2010). Many factors related to patients’ beliefs and perceptions about the illness and its treatment have been explored as variables related to poor treatment adherence (AlGhurair, Hughes, Simpson, & Guirguis, 2012; Alhalaiqa, Deane, Nawafleh, Clark, & Gray, 2012; AlHewiti, 2014; Marshall, Wolfe, & McKevitt, 2012; Rajpura & Nayak, 2013, 2014; Ross, Walker, & McLeod, 2004; Ruppar, Dobbels, & De Geest, 2012).
Even though hypertension is considered an asymptomatic condition, several studies have been oriented to explore patients’ beliefs about hypertension since the seventies. The association of symptoms with hypertension has been explored in several studies. Some studies (Baumann & Leventhal, 1985; Brondolo, Raymond, Rosen, John, & Kostis, 1999; Kottke, Tuomilehto, Puska, & Salome, 1979) have not found any relationship between symptoms reported and blood pressure (BP), arguing that hypertension has no specific symptoms that could be useful to the patient for an estimation of his/her blood pressure. As well, some studies (Baumann & Leventhal, 1985; Brondolo et al., 1999; Kottke et al., 1979) have not found any significant relationship between reported symptoms, mood states and fluctuations in systolic pressure.
Other studies (Kruszewski, Bieniaszewski, & Krupa-Wojciechowska, 2000; Meyer, Leventhal, & Gutman, 1985) have found that a high percentage of hypertensive patients reported symptoms which they believed that were associated to high blood pressure and, consequently, they used them to estimate their blood pressure and to make decisions about the treatment followed. This pattern of behaviour can be considered as beliefs about false symptoms that could interfere with treatment, that is, it would be a mistaken generalization of what Leventhal and his associates called “common sense use of symptoms” as indicators of disease (Meyer et al., 1985). Studies that have explored the presence of these beliefs in hypertensive patients and their role in estimating blood pressure show that the percentage of patients who use symptoms to estimate their blood pressure varies from 50% to 92% (Cantillon et al., 1997; Kjellgren et al., 1998).
Beliefs about symptoms associated with hypertension can negatively affect adherence to treatment, as several studies have shown (Alison, Leventhal, & Leventhal, 2013; Cantillon et al., 1997; Granados & Gil Roales-Nieto, 2005, 2007; Granados, Roales-Nieto, Moreno, & Ybarra, 2007; Kjellgren et al., 1998; Marshall et al., 2012; Ross et al., 2004) and knowledge of the variables associated with their development and maintenance could be of interest to improve adherence. Most patients showing this type of beliefs interpret the perception of symptoms as a sign that their BP is high, which could have the risk of changing their treatment themselves. And vice versa, they interpret the absence of symptoms as a sign that their BP is controlled. For example, in a study with 163 hypertensive patients with pharmacological treatment, we found that 55.5% of the patients with beliefs about symptoms reported failures in their treatment adherence, while this only happened in 25.7% of the patients that did not report beliefs about symptoms (Granados et al., 2007). This relationship between non-adherence to treatment and symptom beliefs was statistically significant (χ2=9.74, p < .01; CI 95%=1.56 - 8.28), with a relative risk of 2.15 (CI 95%=1.20 - 3.86) that the presence of beliefs was associated with failures in treatment adherence.
Also, a recent study has shown that the modification of beliefs about false symptoms, using a feedback procedure, brought an improvement on treatment adherence (Roales-Nieto, Granados, & Márquez, 2014).
Nonetheless, the emergence of these beliefs and their maintenance over time has not been sufficiently explored. Only one study provided longitudinal data, reporting that 71% of 65 newly treated hypertensive patients already showed beliefs about symptoms (e.g., headache, feeling their face burning, or their heart pounding) at the beginning of treatment, while in a six-month follow-up, the number of patients who reported beliefs had risen to 92%. However, the time since each patient was diagnosed as hypertensive was not considered (Meyer et al., 1985).
To the best of the authors’ knowledge, no prior research exists that directly addresses the objectives of the present study. The main purpose of this study was to explore, in a longitudinal design, the presence of beliefs about symptoms in a sample of hypertensive patients, and the relationship between time since diagnosis and the report of beliefs about symptoms. Information related to the moment in which these beliefs emerge could be useful for health-care teams attending patients with hypertension.
MethodDesign and participantsA descriptive survey study according to the classification of Montero and León (2007) involving patients with hypertension who were receiving regular medical care in one Primary Care Centre in the city of Almería (Spain). Eligible patients could not be over 65 years old or under 18. Patients with other disorders (e.g., diabetes, asthma, cardiovascular disease and dyslipidaemias) or a diagnosis of mental disorder (e.g., depression, anxiety disorder) were excluded. The study sample was selected from among the total group of patients with diagnosis of hypertension (342) stratified by time since diagnosis of hypertension. The final sample was composed of 171 eligible patients that accepted to participate, 33 eligible patients refused to participate. All patients were informed that the purpose of the study was to “get a better understanding of the experiences of patients with the disease”.
The study was approved by the Ethics Committee of the University of Almeria and the Research Committee of the Health District of Almeria. Informed Consent by each participant was obtained. Participants were told that the data would be treated in a manner that respected the confidentiality and the anonymity.
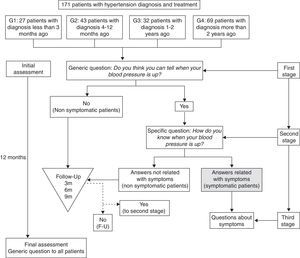
ProcedureParticipants were distributed in four groups according to time since diagnosis: Group 1 (G1) patients with a recent diagnosis (in the previous 3 months); Group 2 (G2) patients who had been diagnosed in the previous 4 to 12 months; Group 3 (G3) patients who had been diagnosed between 13 months and 2 years before; and Group 4 (G4) patients diagnosed over two years before.
A longitudinal study was conducted by way of interviews with patients over time to evaluate the presence of beliefs about symptoms. The initial and final reports of beliefs in the total sample were evaluated at two different stages: at the beginning of the study (Initial assessment) and the other one 12 months later (Final assessment). Belief in symptoms associated with high blood pressure was defined as the report and identification of symptoms that the patient believes are associated to his/her high blood pressure.
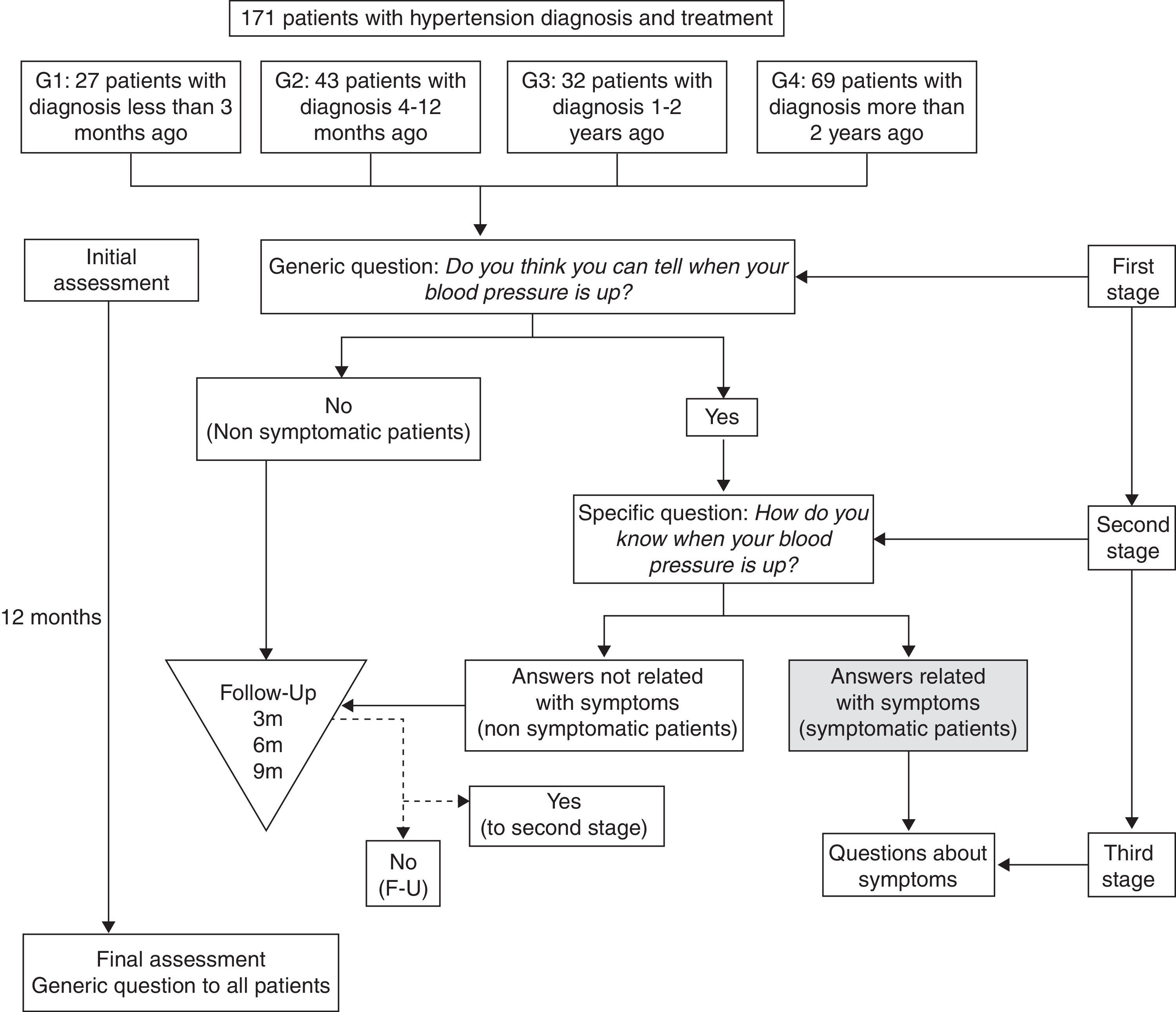
The procedure was implemented according to a three-stage protocol (see Figure 1). In the first stage, patients were asked about their blood pressure with the general question by Meyer et al. (1985): “Do you think you can tell when your blood pressure is up?”. If the answer was negative, the patient was classified as “non-symptomatic”, and no more questions were asked about this. In the second stage, the patients who had given a positive answer to the general question were asked: “How do you know if your BP is high?”. If the answer was not related with symptoms (e.g., “Because I measure it”), the patient was classified as “non-symptomatic” and no more questions about it were asked. The third stage was only carried out with patients who considered their blood pressure to be high because they had perceived some symptoms (patients classified as “symptomatic”). In these cases, new questions were added about their symptoms (i.e., type, frequency, intensity…).
Patients who did not report beliefs about symptoms at the Initial Assessment were interviewed again during a follow-up period (usually every three months when they came to the scheduled visits to the general practitioner). Those patients who reported symptoms any time during the follow up were classified as “symptomatic” according to the third stage of the study protocol.
All patients were evaluated at the Final Assessment.
We contacted with all patients with a diagnosis of hypertension assigned to the Cañada de San Urbano Primary Care Centre (Almeria, Spain). Participants were patients that accepted to take part of the study and met the two criteria of eligibility. The first author, who was not the treating physician neither the attending nurse, informed the participants about the aim of the study.
Data analysisQualitative variables were described as number and percentage. Quantitative variables were described as mean and standard deviation. Statistical differences on age between patients that reported symptoms and those who did not were evaluated using Student test, and statistical differences on sex were evaluated using Chi-square test. A univariate analysis was carried out using a Chi-square test to detect significant differences in the percentage of patients who reported symptoms, both in the initial and final assessments. The McNemar Test was used for intra-group comparisons. We considered a level of statistical significance of .05 (p value). Analyses were carried out using the program SPSS 19.0 (Mac-iOS version).
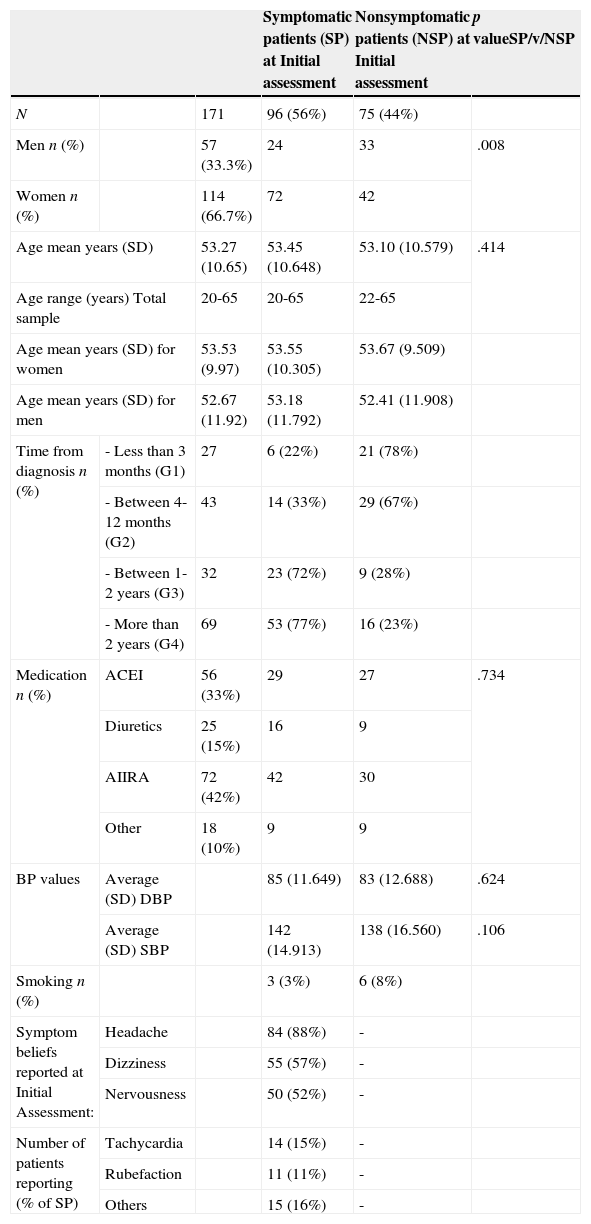
ResultsThe sample was composed of 171 patients with hypertension, 67% women, with a mean age of 53.27 years (SD=10.65), and ranging from 20 to 65. All patients were treated with antihypertensive drugs. The main characteristics of the sample as well as its distribution over time since diagnosis are summarized in Table 1.
Patients’ characteristics.
| Symptomatic patients (SP) at Initial assessment | Nonsymptomatic patients (NSP) at Initial assessment | p valueSP/v/NSP | |||
|---|---|---|---|---|---|
| N | 171 | 96 (56%) | 75 (44%) | ||
| Men n (%) | 57 (33.3%) | 24 | 33 | .008 | |
| Women n (%) | 114 (66.7%) | 72 | 42 | ||
| Age mean years (SD) | 53.27 (10.65) | 53.45 (10.648) | 53.10 (10.579) | .414 | |
| Age range (years) Total sample | 20-65 | 20-65 | 22-65 | ||
| Age mean years (SD) for women | 53.53 (9.97) | 53.55 (10.305) | 53.67 (9.509) | ||
| Age mean years (SD) for men | 52.67 (11.92) | 53.18 (11.792) | 52.41 (11.908) | ||
| Time from diagnosis n (%) | - Less than 3 months (G1) | 27 | 6 (22%) | 21 (78%) | |
| - Between 4-12 months (G2) | 43 | 14 (33%) | 29 (67%) | ||
| - Between 1-2 years (G3) | 32 | 23 (72%) | 9 (28%) | ||
| - More than 2 years (G4) | 69 | 53 (77%) | 16 (23%) | ||
| Medication n (%) | ACEI | 56 (33%) | 29 | 27 | .734 |
| Diuretics | 25 (15%) | 16 | 9 | ||
| AIIRA | 72 (42%) | 42 | 30 | ||
| Other | 18 (10%) | 9 | 9 | ||
| BP values | Average (SD) DBP | 85 (11.649) | 83 (12.688) | .624 | |
| Average (SD) SBP | 142 (14.913) | 138 (16.560) | .106 | ||
| Smoking n (%) | 3 (3%) | 6 (8%) | |||
| Symptom beliefs reported at Initial Assessment: | Headache | 84 (88%) | - | ||
| Dizziness | 55 (57%) | - | |||
| Nervousness | 50 (52%) | - | |||
| Number of patients reporting (% of SP) | Tachycardia | 14 (15%) | - | ||
| Rubefaction | 11 (11%) | - | |||
| Others | 15 (16%) | - | |||
The results showed that in the Initial Assessment, 96 patients out of 171 (56%) were classified as symptomatic, as they reported to be able to know when their BP was high because of the presence of symptoms. The rest of the sample, 75 patients (44%), reported not to know the state of their BP and were classified as non-symptomatic. There were no significant differences between belief in symptoms and age and gender of the patients. In the Final assessment, the number of patients classified as symptomatic rose to 132 (77%), as during the follow-up period 36 more patients reported being able to know when their BP was high due to the presence of symptoms. All patients classified as symptomatic in any of the previous assessments were also classified as symptomatic in the Final assessment. Significant differences in the number of symptomatic patients between the Initial and Final assessments were found (p < .001). The main symptoms reported by patients included headache (reported by 88% of symptomatic patients), dizziness (57%), nervousness (52%), tachycardia (15%), and rubefaction (11%). All patients reported more than one symptom.
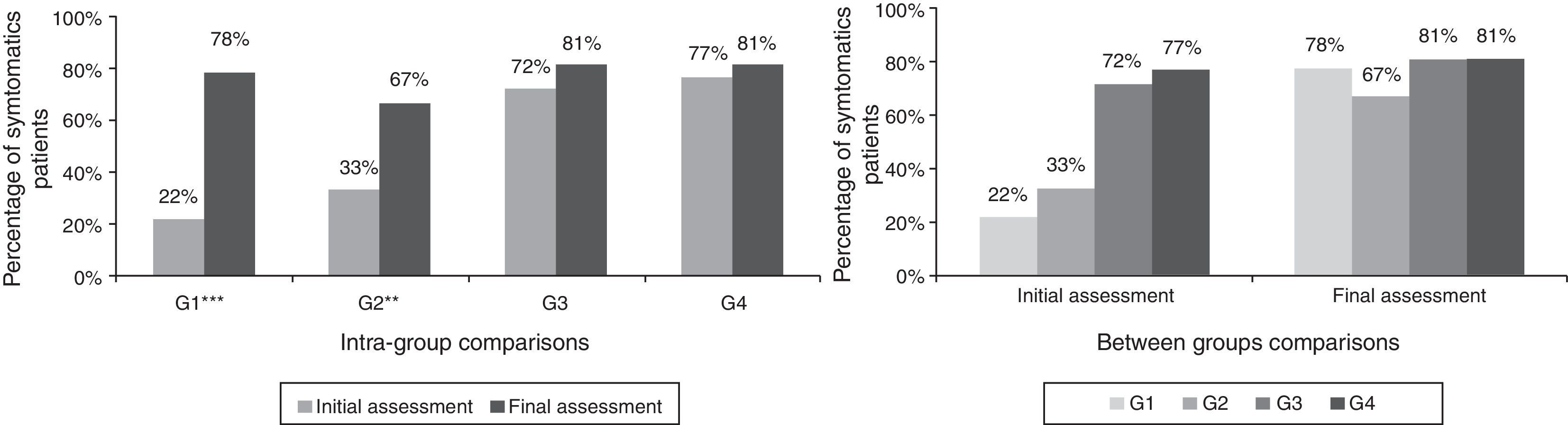
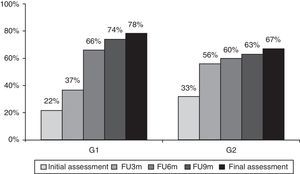
The analysis of the results according to time since diagnosis shows important differences. Figure 2 shows the percentages of symptomatic patients in the Initial and Final assessments for the different groups. The biggest changes are found in G1 and G2, those with a shorter time period since diagnosis. In G1 only 22% of the patients were classified as symptomatic in the Initial assessment, but this figure increases to 78% in the Final assessment, with significant differences (p < .001). In G2 the initial percentage of symptomatic patients was 33%, increasing to 67% in the Final assessment, also displaying statistically significant differences (p < .01). In groups G3 and G4 those with a longer time period since diagnosis, the changes were much smaller and no statistical significance was found.
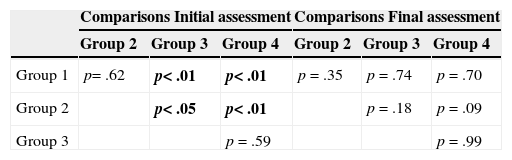
Between-group comparisons of the Initial assessment (see Table 2 and Figure 2) indicated significant differences between G1 and G3 (p < .01), and between G1 and G4 (p < .01), but not among G1 and G2 (p=.62). Also, significant differences were found between G2 and G3 (p < .05), and between G2 and G4 (p < .01). In the Final assessment, no group showed significant differences in comparison with the others. In summary, most of the patients reported beliefs about symptoms at the final assessment.
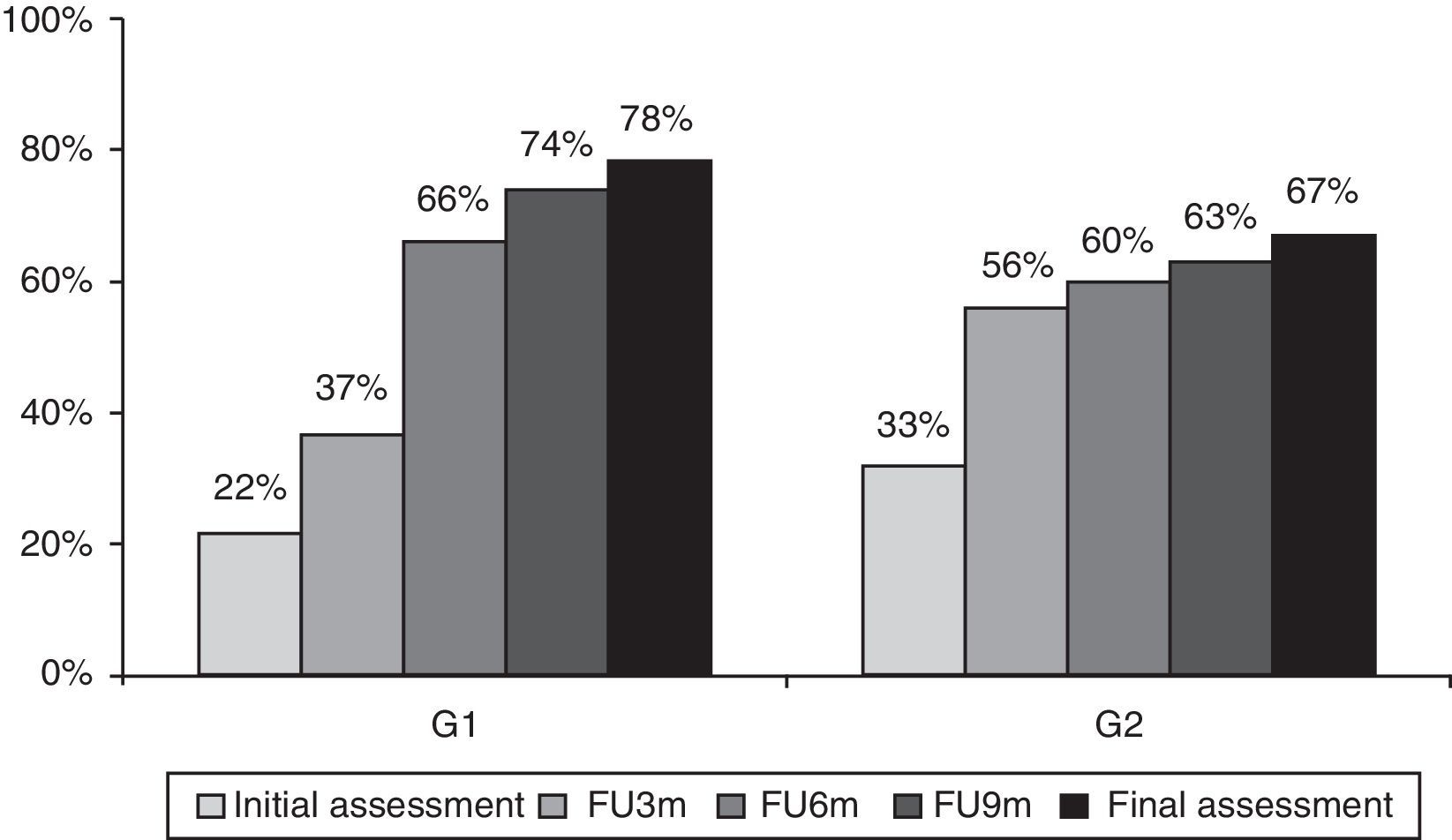
In order to obtain information related to the moment at which beliefs about symptoms appear, a longitudinal analysis of symptomatic patient percentages was carried out only for G1 and G2, using the Initial, 3 months follow-up (FU-3m), 6 months follow-up (FU-6m), 9 months follow-up (FU-9m) and Final assessments. Figure 3 shows the development of the percentage of symptomatic patients in G1 and G2. A progressive increase in the percentage of symptomatic patients was observed in G1, going from 22% at the Initial assessment, to 66% at the follow-up (FU-6m), and reaching 78% in the Final assessment. There were significant differences between the Initial and FU-3m (p < .05) and FU-6m assessments (p < .001), but not between the FU-6m and Final assessments. G2 also showed a change in the percentage of symptomatic patients over time. There were significant differences only between the Initial and FU-3m assessments (p < .05).
Evolution of the percentage of symptomatic patients throughout assessments. Note: FU6m, FU3m and FU9m percentages were calculated from the total number of patients in each group, including as symptomatic the ones that were classified as such in the previous assessments and the patients that emerge as symptomatic in that specific follow-up assessment.
This study presents a longitudinal analysis of the emergence of beliefs about symptoms related to blood pressure. Compared to previous studies it is innovative as it allows the moment at which these beliefs appear to be ascertained. The patients were classified as symptomatic or non-symptomatic based on their reports of beliefs about symptoms (mainly headache, nervousness, dizziness, and rubefaction). Those patients who were classified as non-symptomatic were evaluated every three months over a total period of one year. The results indicate that new symptomatic patients emerged and the percentage of symptomatic patients rose during the study, mainly in groups 1 and 2 (those with a more recent diagnosis).
The results are consistent with previous studies (e.g., Kjellgren et al., 1998; Kruszewski et al., 2000) indicating the importance of this phenomenon, one which affects a high percentage of hypertensive patients that believe they are able to estimate their BP level based on certain signs that they consider to be indicative symptoms of high blood pressure. This gives said patients a false sense of control which could negatively affect their treatment adherence (Cantillon et al., 1997; Granados & Gil Roales-Nieto, 2005, 2007; Granados et al., 2007; Kjellgren et al., 1998), especially as other studies have found that symptomatic patients establish a conflicting generalization, i.e. “the absence of symptoms means that the BP is normal”, irrespective of their adherence to treatment (Granados & Roales-Nieto, 2005, 2007).
Our results indicate that time elapsed since diagnosis could be a very important variable in the formation of beliefs about symptoms, as it is shown by the progressive increase in the percentage of symptomatic patients as time passes after diagnosis.
The results of the Initial assessment already show a pattern between the groups in the reporting of symptoms according to time since diagnosis, confirming that a longer history of hypertension is related to a higher probability of belief in symptoms. The percentage of symptomatic patients in the initial assessment is significantly less in the groups with a shorter time since diagnosis (G1 and G2), and the bigger the difference in time since diagnosis, the bigger the differences between the groups in relation to the presence of symptoms.
Particularly, an analysis of G1 allows to establish that the first year since diagnosis is a critical time period for the emergence of beliefs about symptoms. Data from groups 3 and 4 (those with a longer time since diagnosis) indirectly confirm the idea that the majority of patients that generate symptoms beliefs do it during the first months since diagnosis, as in these groups very few symptomatic patients appear during the follow up period. In fact, the total percentage of symptomatic patients shown at the end of the study in groups 1 and 2 is similar to that of groups 3 and 4 at the beginning of the study, and the time passed since diagnosis in groups 1 and 2 at the end of the study is the same as group 3 at the beginning. This could indicate that after one year since diagnosis, the emergence of beliefs about symptoms is almost incidental. Therefore, the first year since diagnosis seems to be a critical period for the emergence of new cases of symptomatic patients, as during this period nearly all patients who come to generate beliefs about symptoms emerge.
The reasons why the majority of symptomatic patients emerge during this critical period are not clear, and studies that analysed this phenomenon would be needed. In any case, the association of symptoms to pathological processes is a common and natural human experience, so that for a patient it could be “natural” or “logic” to believe that their pathological state (being diagnosed as hypertensive) is associated with signs of that condition (symptoms). According to the hypothesis of the “common sense” use of symptoms as indicators of disease, people are likely to assume that they can detect illness by monitoring body symptoms and to use symptoms to guide and evaluate their body state (Leventhal, Nerenz, & Steele, 1984). As Baumann and Leventhal (1985) established this “common sense” use of symptoms as indicators of disease, it is most probably the product of a history of acute illness episodes throughout their life and the corresponding social learning. The presence of symptoms usually accompanied medical visits, diagnoses, prescriptions, and social relationships with other people about one's and other's physical states. These experiences produce a set of learned illness prototypes or schemata about the occurrence of a symptom and the effect of the verbal label “hypertensive” meaning “I’m ill.”
When considering these results, the methodological conditions of the study should be taken into account. Firstly, patients responded to open questions in the context of a structured interview, without help or guidance, which could have led them to form beliefs related to hypertension. This sets the study apart from previous ones in which patients responded to surveys, questionnaires or checklists which asked about the occurrence and intensity of specific symptoms, without controlling the possible effects of suggestion or considering that the patients could have subsequently derived a possible “relationship” between symptoms and blood pressure (Brondolo et al., 1999; Cantillon et al., 1997; Kjellgren et al., 1998; Meyer et al., 1985). Secondly, the participants in this study represent a large amount of the total number of hypertensive patients in the area where the study took place, and as such, it may be able to represent the heterogeneity of that population. However, the final composition of some groups had reduced number of participants, which could be a limitation for the generalization of the results, and is an aspect which requires further studies with larger samples.
Another possible limitation of the study is the disparity in numbers of male and female participants. However, this is a frequent occurrence in studies with hypertensive patients and the analyses indicate that no significant differences were found related to the reporting of symptoms according to gender.
The results of our study allow some important conclusions related to the treatment of hypertension in Primary Health Care service to be drawn. Firstly, the majority of patients who participated in the study reported beliefs in the form of false symptoms related to high BP, and as such, we are dealing with a phenomenon which affects a significant percentage of patients and requires the necessary attention in treatment protocols and monitoring. Currently, these beliefs are neither evaluated nor considered in treatment protocols, even though the data clearly show their importance as a risk factor for adherence (e.g., Aroian, Peters, Rudner, & Wase, 2012; Cantillon et al., 1997; Chen, Tsai, & Chou, 2011; Granados & Gil Roales-Nieto, 2005, 2007; Granados et al., 2007; Kjellgren et al., 1998).
Secondly, the results indicate that the passing of time is a very important aspect, with a critical period for the emergence of these beliefs. As such, new studies to investigate whether preventive action during the first year could stop or reduce the formation of these beliefs are vital. Any type of preventive intervention with the aim of avoiding the formation of these beliefs and preventing them from becoming risk factors in treatment adherence should take these data into account and be conducted within one year from diagnosis.
Finally, in their short but intense review of the role of perceptions and behaviour of hypertensive patients, the conclusion stated by Langman, Lyons, and Lip (2001) that “comprehensive investigation of the behaviour types of patients, and types of perceptions patients hold about their illness and treatment is required” gains importance with the results of this study, indicating that the patient's behaviour can be a relevant factor in hypertension care and should be deeply explored.
FundingThis study was funded by the Spanish Ministry of Economía y Cmpetitividad, National Research Plan (Research Grants BS022-2002 and PSI2008-00287 to Dr. Roales-Nieto as Chief Investigator of the project). The sponsor of the study had no role in the study design, data gathering, data analysis, and data interpretation, or writing of the report.
We gratefully acknowledge the excellent and continued commitment of the physicians and nurses from the Primary Care Centre that made this study possible. We are indebted to all participating patients involved in this study.