Men do not use external condoms for several reasons, which can result in public health problems. One of these is related to Condom-Associated Erectile Problems. This study aimed to examine the sexual arousal response of heterosexual men when using an external condom made of synthetic resin type AT-10.
MethodA total of 82 Colombian young men (Mage = 23.17 years, SD = 3.04, age range = 18–30) participated in this experimental study. Two random groups (experimental and control; n = 41 each) were compared. The experimental group used condoms, whereas the control group did not. Fit and feel condom perceptions, initial erectile scores, age, and substance use were controlled for. Erection was measured while viewing a sexual video by using penile plethysmography and subjective arousal.
ResultsThe results, obtained from comparing the experimental group (using pre-erection condoms) with the control group (not using condoms), revealed no significant difference in both subjective and physiological sexual arousal. This suggests that pre-erection condoms do not have an effect on the erectile response.
DiscussionMore research is needed in this area to provide treatment and clinical interventions or sexual and reproductive education to mitigate the occurrence of sexual dysfunction, unplanned pregnancies, or sexually transmitted infections. Also, research addresses public health issues related to the prevention and/or intervention of sexual risk behaviors and sexual dysfunctions, highlighting their significance in sexual education and clinical practice.
As a barrier protection method, the external condom (formerly referred to as the male condom) has been effective in preventing unintended pregnancy and Sexually transmitted infections (STIs; Beksinska et al., 2020), including HIV. In general, this barrier method is predominantly made of rubber latex (80 %) and can come in various types, sizes (ranging from snug to long), materials, internal and external variations, colors, textures, odors, and flavors. Additionally, it may include spermicides and special lubricants (Mahdy et al., 2023). According to the WHO (2023), consistent and correct use can enhance the effectiveness of preventing STIs and unplanned pregnancies. Therefore, it is crucial to complement its use with a lubricant that should be compatible with the material the condom is made of (UNAIDS, 2014). Despite being a highly effective latex barrier for preventing such infections (Steiner et al., 2021) and its availability, men worldwide do not use it consistently and/or correctly for several reasons, such as individuals, groups, or cultures (Bjekić et al., 2018; Coast, 2007; Etowa et al., 2021). Thus, STIs and unintended pregnancies remain among the most relevant public health problems today (WHO, 2022a, 2022b). Condom-associated erectile problems (CAEP) are one of the reasons for inconsistent and incorrect condom use in men (D.H. Li et al., 2020). CAEP has been proven to influence the occurrence of risky sexual behaviors (by reducing the motivation to use condoms; Adam et al., 2010; Graham et al., 2006; D.H. Li et al., 2020; Pinchoff et al., 2017) and the effectiveness of campaigns and programs that seek to prevent them (Sanders et al., 2014). Two types of CAEP have been described (Hill et al., 2015; Sander et al., 2015): 1) CAEP during condom application (CAEP-Application), and 2) CAEP while wearing a condom during intercourse (CAEP-Intercourse). CAEP is relevant to the study of sexual health because it is associated with condom use consistency and incomplete condom use (D.H. Li et al., 2020), and unprotected sex lowers self-efficacy (Graham et al., 2006). CAEP appears to occur more frequently in men with weak erectile function without falling into the dysfunctional category (Janssen et al., 2014). The reported prevalence varies from 9 % to 47 % (Adam et al., 2005; Crosby & Sanders, 2017; Li et al., 2020b; Graham et al. 2006; Hill et al., 2015; Janssen et al., 2014; Sanders et al., 2012, 2014, 2015).
Male sexual arousal has been described as a state in which physiological (i.e., objective), motivational, and emotional (i.e., subjective) responses interact to initiate sexual and/or reproductive behavior (Sachs, 2007); however, it can be influenced by various mechanisms ranging from individual to contextual factors. To date, some studies have examined the possible interactions between external condoms and physiological arousal response. Some studies have found that men may experience a decrease in penile blood flow and erectile response when using a condom (Jozkowski & Sanders, 2014). In a study conducted among young heterosexual men, more vibrotactile stimulation was required to achieve erection with condom use (Hill et al. 2014). The scarcity of studies assessing erection with condom use may be due to the implicit need for erection to wear the condom. Given the above, inquiring about the possible impact of external condoms on arousal response—subjective and/or objective—is crucial, as it is one of the main reasons for men to stop using condoms. Thus, it is possible to ascertain whether CAEP is primarily physiological in origin (due to the barrier provided by the condom) or more psychological (a cultural or social attribution). Therefore, the technical aspects of the condom or psychological components should be addressed in sexual health promotion programs and campaigns (Crosby et al., 2018; Jozkowski & Sanders, 2014; Sanders et al., 2014). Thus, the aim of this experimental study, which included a control group, was to examine the sexual arousal response of heterosexual men when using an external condom made of synthetic resin type AT-10. It is expected that erectile functioning has an inversely proportional relationship with CAEP (Janssen et al., 2014), that this is related to self-reported sexual functioning, and that the external condom interferes with the male sexual arousal response.
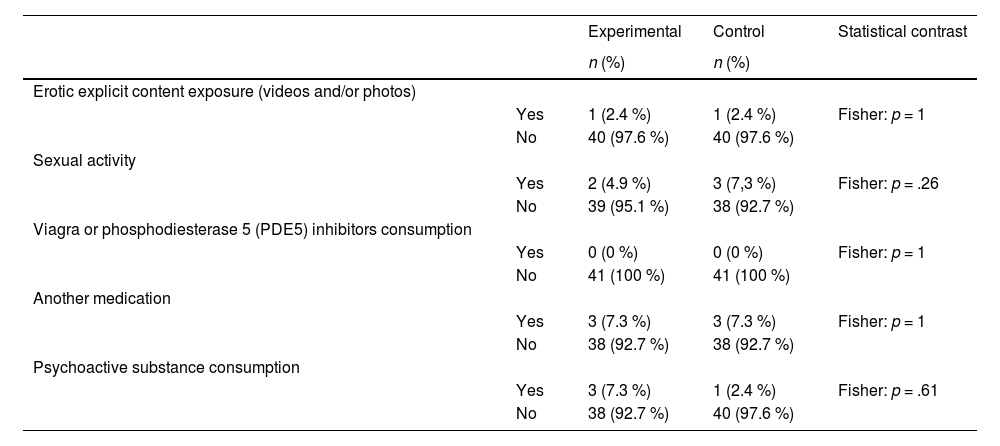
MethodParticipantsEighty-two healthy, young Colombian men (Mage = 23.17 years, SD = 3.04, age range = 18–30) participated in this study. All participants were randomly assigned to one of the two experimental conditions (i.e., experimental and control group). Thus, 50 % (41) of the participants were assigned to each group. Inclusion criteria for participation in the study were as follows: being male, being of legal age (i.e., 18 years old in Colombia), residing in the city of Bogota, being exclusively or mainly heterosexual (Kinsey et al., 2003), absence of or at least mild erectile dysfunction (Rosen et al., 1999), absence of CAEP (i.e., never, or occasionally having presented CAEP in the past three months), and not having undergone fertilization treatment in the past three months. None of the participants assigned to the experimental group had to have used the Smart pre-erection condom. approximately 14 individuals (17.07 %) of the total sample reported having a disease in the past that could affect erectile functioning (i.e., thyroid condition, anxiety, psychoactive substance abuse, depression, coronary heart disease, and herpes; Rosen et al., 1999). Only nine individuals (10.97 %) reported currently having some of these diseases (i.e., thyroid condition, anxiety, alcohol abuse, and urological impairments; Rosen et al., 2005). Regarding psychoactive substances that could alter erectile functioning, approximately 5.4 % (4) of the sample reported using cocaine at some time during the year, 97.6 % (80) alcohol, 4.1 % (3) opioids, 46.1 % (37) tobacco, 46.2 % (37) cannabinoids, and 1.2 % (1) other substances (Rosen et al., 2005). Only three individuals (3.65 %) reported having consumed drugs in the last 15 days (i.e., hypertensives, sleeping pills, and antidepressants; Santini et al., 2014). For further details, see Table A.1. To standardize the experimental sessions, participants were instructed to avoid exposure to erotically explicit photos and videos (i.e., heterosexual pornography), sexual activity (i.e., masturbation, vaginal, anal, and/or oral intercourse), use of Viagra or phosphodiesterase 5 (PDE5) inhibitors (Sandner et al., 2008) or other medications, and use of psychoactive substances, including alcohol, 24 h before the session. Only 45 % of individuals reported using an external condom in at least 90 % of their sexual encounters. See Table B.1 for more specifications on the variables controlled for 24 h before the experimental session. All participants provided verbal and written consent. This study was approved by the Ethics Committee of Konrad Lorenz University. All the procedures followed the ethical guidelines required for research on human subjects.
InstrumentsSocio-Psychodemographic informationSociodemographic and psychosexual information, including age, gender, city of residence, exposure to fertility treatment, current and past illnesses, medications consumed, psychoactive substance use, and sexual orientation (Kinsey et al., 2003) of the participants, were collected through semi-structured interviews. Additionally, during the experimental session, another semi-structured interview was used to determine the participant's condition 24 h before the session (i.e., psychoactive substance use, exposure to explicit erotic content, etc.).
Erectile functioning self-reportThe International Index of Erectile Function (IIEF-5; Rosen et al., 1999) was used to assess sexual functioning. We used the Colombian version (Vallejo-Medina et al., 2022). It is a short questionnaire that evaluates sexual functioning on a five-point Likert scale, which changes according to the item. The score varies between 5 and 25 points, with 21 being the cut-off point (i.e., higher scores indicate the absence of erectile dysfunction). An example of an item would be “How would you rate your confidence in achieving and maintaining an erection?” The estimated kappa coefficient of this index for the current study is 0.85.
Condom-Associated erectile problems (CAEP)To assess both types of CAEP (i.e., application and intercourse), the same questions used in previous studies (Sanders et al., 2014) were translated and adapted to Colombian Spanish. For CAEP-A, men were asked the following: “How often did you lose or start to lose your erection while putting the condom on before vaginal or anal intercourse?” For CAEP-I, the following was asked: “How often did you lose or start to lose your erection while wearing a condom during vaginal or anal intercourse?” For both questions, the alternative answers were “never,” “occasionally,” “less than half the time,” “most of the time,” and “always.” When the participants answered “never” and “occasionally,” they identified themselves as men without CAEP.
Condom fit and feelThe Condom Fit and Feel Scale (Reece et al., 2011) was used to assess the Smart Pre-erection Condom's level of fit and feel. It measures fit, length (i.e., how long or short the condom is), and feel (i.e., tight or loose) with respect to the penis. It consists of 14 items answered on a four-point Likert scale (1 = never applies to me; 4 = always applies to me). An example item is “Condoms fit my penis well.” The previously reported Cronbach's alpha is 0.60 for the Fit scale and 0.89 for the Feel scale (Reece et al., 2011) current sample size is too small for calculating the alpha.
Sexual subjective arousal (SSA)The Spanish version of the Multiple indicators of subjective sexual arousal (MISSA; Mosher et al., 1988; Sierra et al., 2017) was used to measure SSA. This scale uses the dimensions of subjective sexual arousal and subjective genital sensations. The first dimension used a 5-item version, that was answered on a 7-choice Likert-type response scale. The second dimension used only one item, which referred to a self-evaluation of the intensity of genital sensations. Again, this dimension used a 7-choice Likert-type scale instead of the 11 typically used as the orgasm alternatives were suppressed. Both dimensions are considered global indicators of SSA. Cronbach's alpha for this study was 0.85.
Sexual physiological arousalPhysiological signals were collected using the Biopac MP150 data acquisition central module and the Acknowledge IV software, version 4.4.0 (Biopac Systems, Inc. USA). This arousal was assessed as the change in penile circumference increased due to blood supply and was recorded with a penile plethysmograph using a strain gauge of Indium Gallium (I-G), which was connected to the DA100C module. The first assessment was performed using an 85–95 mm circumference plethysmograph. If the basal circumference exceeded 110 mm, the sensor was replaced by a larger one. Each participant applied the sensor according to previously standardized instructions.
Sexual stimulusThe stimuli used in the present study were validated for Colombian men, who were exclusively or mainly heterosexual (Vallejo-Medina et al., 2017). Six videos are edited and available in our laboratory. Three of these videos had neutral content (NS: e.g., plants, water, forests, clouds, landscapes, etc.), while the other three had explicit sexual content (SS). All videos were three minutes and fifteen seconds long. For the SS, the first 15 s showed non-genitalized scenes that allowed the participant to prepare for the video and decide whether to participate. The next minute corresponds to the cunnilingus scene, the following minute to fellatio, and the remaining minute to vaginal intercourse. The six videos were presented in an alternating sequence (i.e., NS1 - SSx - NS1 - SSx - NS3 - SS3; Vallejo-Medina et al., 2017) that were previously set and balanced to guarantee their presentation to the same number of participants.
Smart pre-erection condomThe Smart Pre-erection Condom by Unique was used in this study. It is a condom manufactured in Colombia with sanitary registration (it is also authorized in other countries). It is made of AT-10 Synthetic Resin with a nominal width of 60 mm and is transparent in color. The Smart Pre-erection Condom should be inserted when the penis is in a flaccid or basal state. When an individual's penis begins to develop an erection, the condom is molded according to its size and shape. Instructions on how to insert a condom into the package. For information on how to use or purchase condoms, please consult the following links: https://www.youtube.com/watch?v=mykdJl96V8g
ProcedureScreeningBoth screening and experimental processes were simultaneously conducted. All screening questionnaires (i.e., sociodemographic and psycho-sexual information) were mapped using the SurveyMonkey© platform to obtain a survey. This survey was published and promoted on our institutional SexLabKL Facebook page. The participants voluntarily signed the screening questionnaire. To safeguard the anonymity and confidentiality of participants, a coding system was implemented during the recruitment phase. Each participant was assigned a code composed of their initials and three numbers from their identity cards. No information that could reveal their identities was solicited, ensuring the preservation of their confidentiality, anonymity, and autonomy throughout the study. Eligible participants were then contacted through WhatsApp©, and the experimental sessions were scheduled based on their availability and willingness to participate. To prevent duplication of participant information, control measures were implemented, including checks on IP addresses, age, and WhatsApp© numbers, following similar protocols as described in other studies (Vallejo-Medina et al., 2017).
Experimental sessionPrior to the participants’ visit, all equipment was prepared together with plethysmograph calibration. All the participants were randomly assigned to each group (i.e., experimental and control). Once the participants arrived at the laboratory, we explained to them the instruments to be used and the stimuli to be seen and guided them to the laboratory. The SexLab KL is made up of two rooms: 1) the control room, which houses the computers and the central modules to collect physiological signals, and 2) the experimental room, equipped with a monitor to present the stimuli and the MISSA and a chair. Both rooms were separated by a door that was closed during the experimental session. The experimental room was acoustically isolated and had temperature conditions varying from a minimum range of 20.21 °C to a maximum of 20.24 °C. An intercom was used to communicate between the rooms. Once the participant had cleared any doubts, they signed the informed consent form and were asked questions about their situation 24 h before the session (i.e., substance use, exposure to explicit erotic content, etc.). All participants then put on the penile plethysmograph and the condom, and the experimental group performed this action by themselves (the Smart Pre-erection Condom before the plethysmograph). All participants watched sequences of six videos; the erotic videos were randomly alternated. It took three minutes to stabilize the signal and detect any irregularities at the beginning of each session. At the end of each SS, MISSA was presented to assess its SSA. Each session lasted approximately one hour. When the third MISSA was presented, the participants were asked to remove the penile plethysmograph and put their clothes back on. The participant then met with the evaluator in the control room and was asked to complete the Fit and Feel Scale if they were in the experimental group, while also receiving feedback on their physiological responses. All participants received another smart protection condom packet containing three condoms and a copy of the informed consent form at the end of the session. All participants were informed of their willingness and freedom to participate in the research and could decide whether to continue or stop the session at any time they wished.
Data analysisAfter concluding the experimental session and obtaining the penile plethysmograph report (i.e., changes in penile circumference due to increased blood supply), we collected data on four erection properties: 1) the average percentage of circumference increase (i.e., average percentage increase obtained during the visualization of each SS of penile girth); 2) the maximum percentage of penile circumference increase (i.e., maximum percentage of penile girth increase reached in each SS); 3) the latency (i.e., the time it takes to obtain an increase in girth greater than 5 % from the time the SS is initiated); and 4) the duration (i.e., the time at which penile girth remains above the 5 % increase at each SS) of erection. We conducted Mann-Whitney U tests due to the non-normality of the sample data in each group and its size. Additionally, we selected this test because of its robustness in small samples and its ability to handle non-parametric data. Measures of effect size were not computed in this study. Comparisons were carried out between the experimental and control groups at one temporal points: after the evaluation. We performed regressions on the descriptive data of the sample. We use R software for data analysis (Team R, 2013). Additionally, we used the ggplot2 (Wickham et al., 2021) package of the same software with the R programming language to plot the results of this research, and the ggExtra (Attali, 2016) package was used to group these graphs.
ResultsNon-Latex smart pre-erection condom® fit and feelOverall, participants in the experimental group reported feeling a good fit on the Condom Fit and Feel Scale for the Smart Pre-erection Condom to their penis (M = 3.243; SD = 0.681; maximum possible score is 4) and not feeling too long (M = 1.853; SD = 0.709), short (M = 1.524; SD = 0.734), tight (M = 1.524; SD = 0.734), or loose (M = 1.548; SD = 0.691), with 1 being the lowest possible score in these three categories.
Differences between groups by sexual arousal variablesThe erection was conceptualized based on four variables (average percentage of circumference increase, maximum percentage of circumference increase, erection latency, and erection duration) assessed during the experimental session (see the Methods section for more experimental details). Data analysis showed no significant differences between the groups (with and without condoms) and the erection variables: average percentage of circumference increase (Mann-Whitney U test; z = −0.450, p = .653, two-sided), maximum percentage of circumference increase (Mann-Whitney U test; z = −0.116, p = .908, two-sided), erection latency (Mann-Whitney U test; z = −1.275, p = .202, two-sided), and duration of erection (Mann-Whitney U test; z = −0.552, p = .581, two-sided). For further information, please refer to Fig. A.1.
Sexual subjective arousalSimilar to the erection variables, subjective sexual arousal showed no statistical differences between the groups (Mann-Whitney U test; z = −1.342, p = .180, two-sided). For more information, see Fig. B.1.
Erectile functioning and condom useFig. C.1 shows the independence between self-reported erectile functioning (IIFE-5) and the assessed erection variables (average percentage of circumference increase, maximum percentage of circumference increase, latency, and duration of erection). The prediction was not significant for either the experimental or the control groups.
DiscussionMany studies have reported that condoms affect their erectile response (Farrington et al., 2016; González-Hernández et al., 2020; Mustanski et al., 2021), highlighting the need to increase the intensity of intercourse or drug use to obtain more stimulation in response to erection loss while wearing a condom (CAEP-Intercourse; Exline et al., 2019; Hill et al., 2015; Suppiah et al., 2016; Reed et al., 2021). This implies a greater tendency to acquire STIs and/or unintended pregnancies in individuals with stable or casual sexual partners (Pöyhönen et al., 2020). This study examines the sexual arousal response of heterosexual men when using an external condom made of synthetic resin type AT-10. It was generally observed that pre-erection condom use did not interfere with male arousal response (subjective or erection). The use of pre-erection condoms also did not appear to be associated with self-reported erectile function (IIEF-5).
To the best of our knowledge, this study is the first to investigate the arousal response of heterosexual men when using a condom made of AT-10 type synthetic resin by phallometry. This study has proven the feasibility of assessing erection while using the external condom and allows for the objective evaluation of CAEP-I from the first state or penile flaccidity. Thus, this study showed that condom use—at least the Smart Pre-erection Condom use—does not seem to affect erection, although CAEP is highly prevalent (from 9 % to 47 %; Adam et al., 2005; Crosby & Sanders, 2017; Graham et al. 2006; Hill et al., 2015; Janssen et al., 2014; Li et al., 2020b; Sanders et al., 2012, 2014, 2015). These values could be due to the psychological attribution of condom use rather than the barriers to condom use. This is expected, as CAEP expectations are reported even among young people who have never used condoms (Morales et al., 2019; Vallejo-Medina et al., 2020), and have decreased after implementing health promotion programs (Anstee et al., 2019). Indeed, CAEP could be related to a negative attitude toward condom use with respect to pleasure (Plaza-Vidal et al., 2020).
Subjective sexual arousal is another relevant element when assessing sexual arousal activity (Chievers et al., 2010) as it seems to influence the systems of sexual regulation and activation (Laan & Janssen, 2007). Thus, male sexual experience is shaped by this and peripheral feedback from genital arousal (stimulus explicitness; Laan & Janssen, 2007). This suggests that the mismatch between subjective and physiological sexual arousal may be an important factor in determining sexual problems in men (Chievers et al., 2010). Although the external condom may contribute to such a mismatch, the results of this study showed no significant statistical differences between the groups in terms of subjective arousal. This indicated that the presence of CAEP (specifically CAEP-I) may be due to two possible reasons. First, other psycho-environmental variables need to be studied in detail (e.g., over-demanding male performance, condom manipulation effectiveness) to determine their relationship with CAEP. Second, the material of the common condom (i.e., latex) may be a moderating variable in the presence of CAEP.
ConclusionThere was independence between self-reported erectile functioning (IIFE-5) and the four erection variables assessed in both groups. This suggests that, based on our data, psychological factors related to self-reported erectile functioning do not appear to significantly influence the measured aspects of erection. This contradicts the traditional hypothesis that predicts that erectile functioning has an inversely proportional relationship with CAEP (Janssen et al., 2014).
Limitations and future directionsThis study is a pioneer in investigating the possible interference of an external condom made of a material other than latex on erectile functioning. The impact of its results on public health issues, such as prevention and/or intervention of sexual risk behaviors to mitigate unintended pregnancy and STI and sexual dysfunctions (e.g., erectile dysfunction; clinical practice), is inherent (Gómez-Lugo et al., 2022). However, factors such as the sexual orientation of the sample (i.e., exclusively or mainly heterosexual), the absence of groups with Condom-associated erectile problems (CAEP), the sample size, or the use of a non-traditional condom may affect the results, and these factors should be considered with caution. To pursue this line of research and achieve extrapolation of results, the following are recommended: compare materials (i.e., latex versus synthetic resin type AT-10, or others), including men who have sex with men and groups with types of CAEP (CAEP-A and/or CAEP-I), or monitor the influence or direction of penile sensitivity (e.g., with vibrotactile stimulation; Hill et al., 2014) with respect to the other measurements taken in this investigation. It is important to recognize that the decision to potentially use latex condoms should be approached with caution, considering various contextual, demographic, ethical and laboratory factors.
Sample Sociodemographic Data.
Note: M, Mean; SD, Standard deviation; n, number of cases; IIFE-5, International Index of Erectile Function; CAEP-A, Condom-Associated Erectile Problems Application; CAEP-I, Condom-Associated Erectile Problems Intercourse.
Participants’ Conditions 24 H before the Experimental Session.
Note: n, number of cases.