Disgust, in addition to fear, is a prominent emotional state associated with avoidance of distressing stimuli. While most of the research in disgust has been conducted in relation to Obsessive-Compulsive Disorder (OCD), recent data has also implicated disgust in the etiology of anxiety disorders in general. Studies have shown that decreases in disgust are key to symptom reduction in individuals with OCD. However, there has been little empirical work exploring whether these interventions are efficacious for childhood anxiety disorders that present with prominent disgust components. This study examined how disgust propensity in children with anxiety disorders responds to cognitive-behavioral therapy (CBT) with an emphasis on exposure. Forty-one children, ages 7 to 17, with anxiety disorders were evaluated for disgust propensity and were treated with intensive, weekly, CBT. It was found that disgust levels decreased following treatment across all anxiety disorder diagnoses, where children with primary OCD exhibited significantly greater reductions. Clinical implications and suggestions for further research of the treatment of disgust in relation to childhood anxiety disorders are discussed.
La asco, además del miedo, es un estado emocional prominente asociado con la evitación de estímulos perturbadores. Aunque la mayoría de la investigación se ha llevado a cabo en relación con el trastorno obsesivo-compulsivo (TOC), datos recientes han implicado la asco en la etiología de trastornos de ansiedad en general. Se ha demostrado que la disminución de la asco es clave para la reducción de los síntomas en personas con TOC. Sin embargo, son escasos los trabajos que exploren si estas intervenciones son eficaces en trastornos de ansiedad en la infancia con componentes prominentes de asco. Este estudio examinó cómo la propensión a la asco en niños con trastornos de ansiedad responde a la terapia cognitivo-conductual (TCC) con énfasis en la exposición. Cuarenta y un niños de 7 a 17 años, con trastornos de ansiedad, fueron evaluados en la propensión a la asco y tratados semanalmente con TCC intensiva. Se encontró que los niveles de asco disminuyeron tras el tratamiento en todos los diagnósticos de trastorno de ansiedad, siendo los niños con TOC primario los que mostraron reducciones significativamente mayores. Se discuten las implicaciones clínicas y sugerencias para futuras investigaciones sobre el tratamiento de la asco en relación con los trastornos de ansiedad infantil.
Anxiety disorders are marked by excessive fears, nervous affect, and avoidance of a wide range of specific objects and situations. Mechanisms considered critical in the development and maintenance of anxiety disorders are fear arousal that becomes associated with the presence of the particular stimuli, and corresponding relief of anxiety when these situations are avoided (Taylor, Cox, & Asmundson, 2009). Theoretical and empirical evidence supporting the role of fear associations in anxiety disorders has informed the development of exposure therapy, one of the most widely utilized empirically-supported treatments for anxiety disorders (Abramowitz, Deacon, & Whiteside, 2011). Exposure reduces anxiety by creating novel learning experiences with previously feared stimuli in which anticipated negative consequences do not occur. This treatment has been shown to reduce symptoms of anxiety disorders with large effect sizes across numerous diagnoses (Olatunji, Cisler, & Deacon, 2010).
While fear is a potent motivator for avoidance in anxiety disorders, it is not the only emotion that prompts this behavioral pattern. Disgust is another prominent emotional state associated with avoidance of distressing stimuli. Disgust is an emotion that evolved to protect humans from ingesting potentially harmful substances (Miller, 1997). In recent years, disgust has been increasingly recognized as a complex emotion that consists of several higher-order components, including reactions specific to violations of the body envelope that remind humans of their mortality or animalistic nature (animal-reminder disgust), moral transgressions (moral disgust), and contamination disgust–the propensity of one disgusting object to transmit disgusting properties to another object (Kelly, 2011; McKay & Tsao, 2005). Contamination disgust may encompass a range of situations that may or may not involve actual physical contact with a disgusting object, such as: objects that are neutral but come into incidental contact with a disgusting object (“law of contagion”), objects that are neutral but otherwise resemble a disgusting object (“law of similarity”), and objects that are removed from a disgusting object by several points of contact (“sympathetic magic”; Rozin & Fallon, 1987).
Research has shown that disgust plays an important role in the etiology of anxious psychopathology (Olatunji & McKay, 2007, 2009). First, at an observational level, the disgust-based concern related to contracting illness and experiencing overt physical harm is reflected in the symptoms of various phobias (Davey, Bickerstaffe, & MacDonald, 2006). The behavioral avoidance characteristic of many anxiety disorders also may be related to disgust, as data shows that many individuals exhibiting anxious avoidance are highly responsive to disgust-based information in the general environment (e.g., Woody & Tolin, 2002). Other evidence has even speculated that the experience of disgust predisposes individuals to negative interpretation bias, therefore contributing to the emergence of anxiety disorders on a general level (Matchett & Davey, 1991).
Data has also implicated disgust in specific anxiety disorders, with the bulk of this work conducted in relation to obsessive-compulsive disorder (OCD; e.g., Olatunji, Tart, Ciesielski, McGrath, & Smiths, 2011). Within the OCD literature, research has suggested that disgust is particularly salient for individuals who experience contamination-related obsessions and compulsions. For example, one study showed that individuals with elevated contamination fears tended to avoid behavioral tasks associated with stimuli that were perceived as disgusting but not actually physically harmful (e.g., drinking from a cup of fresh water with a label affixed reading “saliva sample”), as well as animals that may transmit germs or disease (e.g., holding a live earthworm). Other research has shown that the “sympathetic magic” aspect of contamination disgust is present in individuals with contamination-based OCD symptoms. Compared with non-anxious control subjects, these individuals were more fearful and avoidant of a potentially contaminated object even when it was many steps removed from the contamination source in behavioral avoidance tests using a pencil that touches a contaminant, which in turn touches another pencil, then touches a different pencil, and so on (Tolin, Worhunsky, & Maltby, 2004). Similar evidence was also found in an undergraduate sample, in which students with elevated contamination fears exhibited more avoidance of behavioral tasks involving “sympathetic magic” than individuals with elevated trait anxiety (Tsao & McKay, 2004).
Further tests of the specificity of disgust in contamination-based OCD symptoms have shown this direct link to exist independent from the effects of anxiety (Moretz & McKay, 2008). Other studies have replicated this unique and significant relation between disgust and contamination fear after controlling for negative affect (Olatunji, Moretz et al., 2010). Finally, higher levels of disgust sensitivity have been associated with more stable and persistent contamination fears in growth curve analyses (Olatunji, Moretz et al., 2010).
Although a majority of the literature examining disgust in OCD has focused on the connection between disgust and contamination-based OCD, disgust seems to be involved in other symptom presentations of OCD as well. Elevated disgust sensitivity has been associated with the frequency and severity of general obsessionality (Thorpe, Patel, & Simonds, 2003), findings which have been replicated several times (David et al., 2009; Olatunji, Unoka, Beren, David, & Amstrong, 2009). Other work has also extended the findings of relations between disgust and general obsessionality checking (David et al., 2009) and harm avoidant (Olatunji et al., 2009) OCD symptom presentations more specifically.
In addition to the evidence supporting the importance of disgust in the etiology and maintenance of OCD and other anxious psychopathology in adults, a small, yet, burgeoning body of research has associated disgust specifically with childhood anxiety disorders. It has been suggested that, as has been shown in adults, disgust plays a role in the pathogenesis of childhood anxiety (Muris, Merckelbach, de Jong, & Ollendick, 2002; Muris, Merckelbach, Schmidt, & Tierney, 1999). Experimental data has demonstrated that disgust mediates fear-related beliefs, leading to avoidant behavior (Muris et al., 2009) and anxious interpretation bias towards novel stimuli (Muris, Huijding, Mayer, & de Vries, 2012) in children. Other evidence even suggests that disgust propensity may be transmitted inter-generationally beginning as early as infancy with a mother's verbal and nonverbal displays of disgust in the presence of her child (Muris, Mayer, Borth, & Vos, 2013). However, it is worth noting that in another study, disgust failed to show an independent association to anxiety disorders when evaluated along with trait anxiety (Muris, van der Heiden, & Rassin, 2008), suggesting that disgust mechanisms alone may not be sufficient to explain the emergence of pediatric anxiety disorders.
Research shows that in the treatment of adults with anxiety disorders, disgust reactions are either resistant to treatment or slower to respond to in vivo exposure (Mason & Richardson, 2012; McKay, 2006) in comparison to fear responses. Recent quasi-experimental research has corroborated that disgust does indeed respond to exposure at a slower rate than fear, albeit only when study participants endorsed high contamination aversion (Adams, Willems, & Bridges, 2011), indicating a probable mediation role of contamination aversion in predicting treatment outcome for disgust-related anxiety. Yet despite the evidence that disgust does not respond as well to exposure therapy as does fear, studies have shown that decreases in disgust are key to symptom reduction in individuals with OCD (Olatunji et al., 2011). Taken together, these findings call for continued research on the treatment of disgust in order to improve anxiety treatment outcomes. Further, while there is much data demonstrating empirical support for childhood anxiety treatments (e.g., exposure therapy), there has been little work exploring whether these interventions are efficacious for childhood anxiety disorders that present with prominent disgust components. Specifically, clinical evaluations of the reduction of disgust in children at treatment completion have yet to be conducted.
This study aims to expand disgust-related research and its associations to anxiety disorders to children samples. The purpose of this study is twofold: (1) to evaluate level of disgust propensity in children with OCD compared to children with other anxiety disorders at baseline, and (2) to compare the role of reductions in disgust propensity following treatment in children with OCD versus other anxiety disorders. We hypothesized that cognitive-behavioral therapy with an emphasis on exposure therapy would reduce disgust propensity across anxiety disorders, but particularly for OCD.
MethodParticipantsForty-one children, ages 7 to 17, received intensive, weekly cognitive-behavioral therapy (CBT) at a private psychological practice specializing in anxiety disorders in Westchester, NY. Participants were 11.78 years old on average (SD=2.9), and predominately male (61.0%) and Caucasian (87.8%). Twenty children were diagnosed with primary OCD, and 21 children had another primary anxiety disorder diagnosis, including: separation anxiety disorder (n=6), generalized anxiety disorder (n=5), panic disorder (n=3), social anxiety disorder (n=3), posttraumatic stress disorder (n=2), selective mutism (n=1), and specific phobia (n=1). All participants were self-referred to treatment.
MeasuresAnxiety Disorders Interview Schedule for DSM-IV: Parent and Child Versions (ADIS-IV-C/P). The ADIS-IV-C/P (Silverman & Albano, 1996) is a clinician-administered, structured interview that was developed from DSM-IV diagnostic criteria for anxiety disorders. The participant first rates symptom-related situations for distress, indicating on a nine-point thermometer scale how they would feel in the situation (0=I feel fine, 8=I feel extremely distressed). The participant also rates same situations for the level of avoidance that they induce, or if avoidance is not possible, how much they would like to avoid the situation if they could (0=I never try to avoid this situation, 8=I always try to avoid this situation). Clinician-rated severity (CRS) is calculated as an overall score for each diagnosis. The ADIS-IV-C/P has demonstrated strong psychometric properties, including strong inter-rater reliability (parent-interview κ=.98, child-interview κ=.93; good test-retest reliability (parent-interview r=.76; and strong concurrent validity. The ADIS-IV-C/P has also been shown to be sensitive to changes related to treatment.
Children's Yale-Brown Obsessive-Compulsive Scale (CY-BOCS). The CY-BOCS (Scahill et al., 1997) is a ten-item semi-structured measure of childhood OCD symptom severity. The CY–BOCS consists of two subscales, Obsessions Severity (five items) and Compulsions Severity (five items), which are combined to create a total score. Items are rated on a five-point Likert scale assessing the severity of symptoms (i.e., distress, frequency, interference, and resistance) and the child's perceived control over his or her symptoms. The CY-BOCS shows high internal consistency (Cronbach's α=.87) as well as good to excellent test-retest reliability (ICCs ranging from .66 to .91). The CY-BOCS total scores show strongest correlations with the Leyton Obsessional Inventory score (r=.62) compared with r=.34 and r=.37 for the Children's Depression Inventory and Revised Children's Manifest Anxiety Scale total score, respectively, indicating strong concurrent and divergent validity (Scahill et al., 1997).
Disgust Emotion Scale for Children (DES-C). The DES-C (Muris, Huijding, Mayer, Langkamp, et al., 2012) is a 30-item scale assessing individual differences in disgust propensity across five domains: animals (e.g., “The sight of a large slug”), injection and blood (e.g., “A small vial of your blood”), mutilation and death (e.g., “Photos of wounded soldiers”), rotting foods (e.g., “A piece of rotting steak”), and odors (e.g., “The smell of human feces”). Each domain is covered by six items for which children rate the degree of disgust that they would experience if they were to be exposed to that item, using a 5-point Likert scale ranging from 0 (no disgust at all) to 4 (extreme disgust). The DES-C has shown excellent internal validity (Cronbach's α=.93) for the total scale, and ranging from α=.77 (animals) to α=.91 (rotting foods) for the subscales. The DES-C demonstrates good predictive validity, showing total scores strongly related to animal phobia and blood-injury phobia (r=.66 and .68, respectively) than to other phobias less salient to disgust, and moderate behavioral correlations with avoidance and feelings of disgust (Muris, Huijding, Mayer, Langkamp, et al., 2012).
Childhood Anxiety Sensitivity Index (CASI). The CASI (Silverman, Fleisig, Rabian, & Peterson, 1991) is a self-report questionnaire designed to assess fear and distress evoked by anxiety symptoms in youth. Items in the CASI include, “It scares me when my heart beats fast” and “When I am afraid, I worry that I might be crazy.” Respondents are asked to rate agreement with each of 18 items on a three-point Likert scale ranging from 1 (none) to 3 (a lot). Total scores can range from 18 to 54, with higher scores indicating greater anxiety sensitivity. The CASI has good internal consistency (Cronbach's α=.87; Weems, Hammond-Laurence, Silverman, & Ginsburg, 1998) and acceptable test-retest reliability at two weeks (r=.76 and r=.79 for the nonclinical and clinical samples, respectively; Silverman et al., 1991).
ProcedureTreatmentChildren received CBT specifically tailored to their presenting primary symptoms, which was delivered by a psychologist specializing in anxiety disorders. All children received exposure therapy (or exposure with response prevention for children diagnosed with OCD) as the main focus of treatment. Adjunctively, children ages 7 to 13 were administered a modified version of the Coping Cat cognitive therapy protocol (Kendall & Hedtke, 2006) and children ages 14 to 17 were administered the C.A.T. Project protocol (Kendall, Choudhury, Hudson, & Webb, 2002). Because the modifications to these protocols were primarily to emphasize the cognitive intervention components, the psychoeducational components were omitted. Instead, psychoeducation was delivered during the session immediately following the child's initial diagnostic evaluation (administration of the ADIS-IV-C/P). Weekly sessions were 45-50minutes long, and treatment lasted for 16 to 17 weeks. Parents were asked to participate in sessions every three to four weeks. These sessions focused on ensuring the child's participation in behavioral and cognitive exercises between sessions, as well as identifying potential impediments to maintaining consistency with these between-session exercises.
AssessmentThe ADIS-IV-C/P (Silverman & Albano, 1996) was used to diagnose participants with primary anxiety disorders prior to the start of treatment. This assessment was conducted by the treating clinician. All children completed the DES-C, and CASI approximately one week pre- and post-treatment. Children diagnosed with OCD also completed the CY-BOCS both before and after receiving exposure therapy.
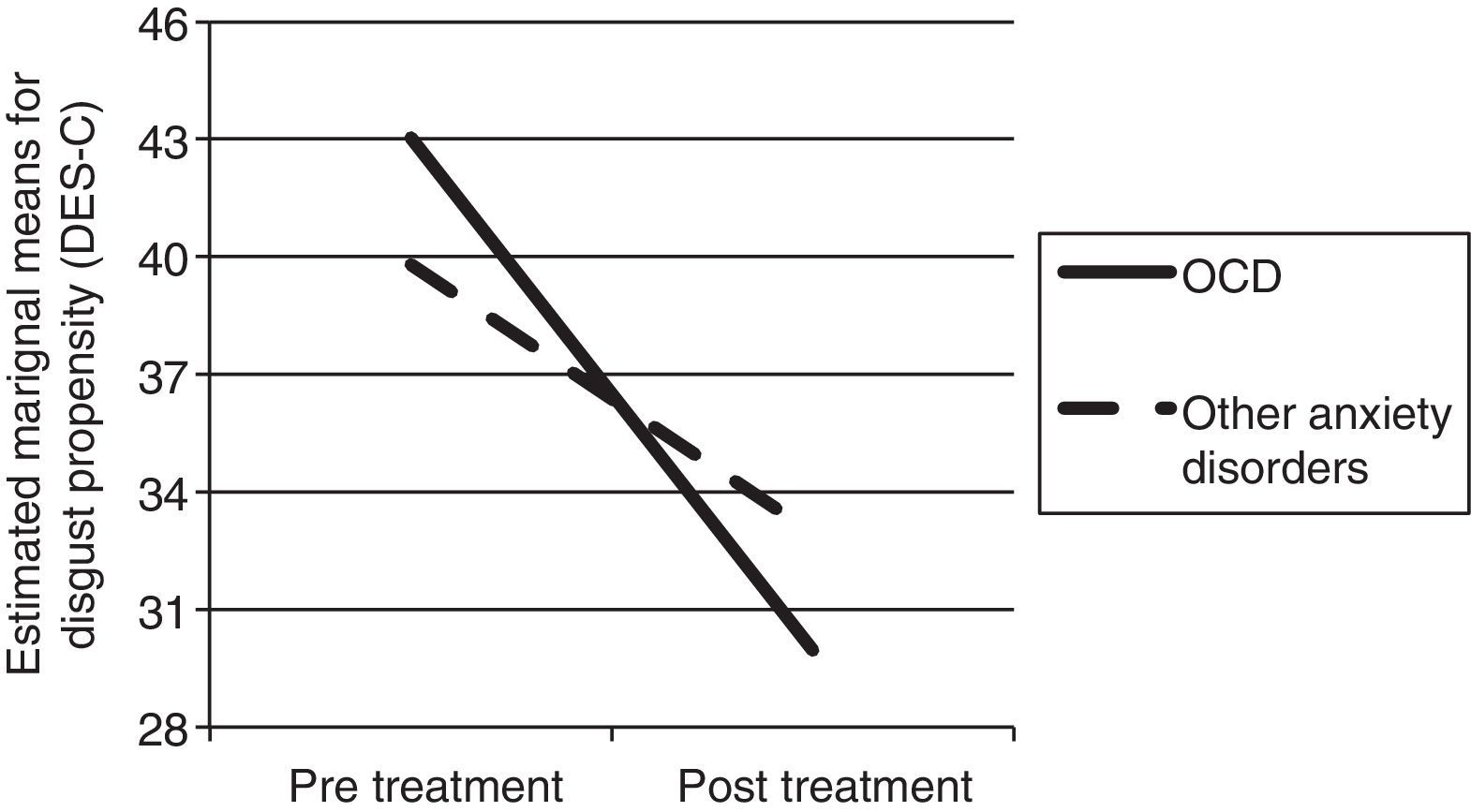
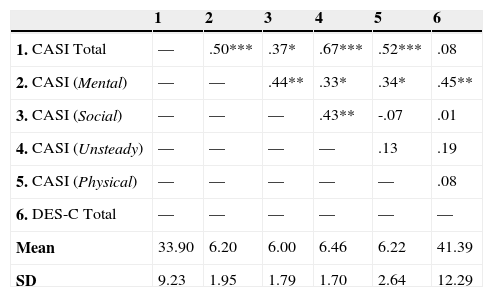
ResultsZero-order correlations of child self-report measures at baseline are reported in Table 1. Analysis with t-test revealed no significant differences in baseline levels of disgust (as measured by DES-C) between children with primary OCD (n=20) versus other anxiety disorder diagnoses (n=21). Repeated measures analysis of variance (ANOVA) analyzed differences in disgust levels from pre- to post-treatment. It was found that, in general, disgust levels, as measured by the DES-C, decreased following treatment across all anxiety disorder diagnoses (F(1,39)=46.77, p<.001; partial η2=.55). The average reliable change index (RCI; Jacobson & Truax, 1991) for reductions in disgust symptoms was 2.15 (SD=2.12), exceeding the threshold of 1.96 that indicates clinically significant symptom reduction (Jacobson & Truax, 1991). However, children with primary OCD exhibited significantly greater reductions in disgust following treatment than children with other primary anxiety disorder diagnoses (F(1,39)=4.58, p=.04; partial η2=.11; see Figure 1).
Zero-order correlations among baseline self-report measures.
| 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|
| 1. CASI Total | — | .50*** | .37* | .67*** | .52*** | .08 |
| 2. CASI (Mental) | — | — | .44** | .33* | .34* | .45** |
| 3. CASI (Social) | — | — | — | .43** | -.07 | .01 |
| 4. CASI (Unsteady) | — | — | — | — | .13 | .19 |
| 5. CASI (Physical) | — | — | — | — | — | .08 |
| 6. DES-C Total | — | — | — | — | — | — |
| Mean | 33.90 | 6.20 | 6.00 | 6.46 | 6.22 | 41.39 |
| SD | 9.23 | 1.95 | 1.79 | 1.70 | 2.64 | 12.29 |
Note: *=p<.05; **=p<.01; ***=p<.001. CASI=Childhood Anxiety Sensitivity Index; DES-C=Disgust Emotion Scale for Children
SD=standard deviation.
The RCI was calculated for changes in disgust following treatment, as measured by the DES-C. As there is no test-retest reliability available as of this writing for this measure, we relied on the established Cronbach's alpha (Truax & Thomas, 2008). Amongst children with a primary diagnosis of OCD, RCIs for disgust propensity were highly correlated with baseline CY-BOCS total scores (r(20)=.62, p=.004), and especially with the obsessions subscale (r(20)=.77, p<.001). RCIs for disgust propensity were not correlated with other symptom measures at baseline, either for the sample as a whole or when children with primary diagnoses of OCD versus other anxiety disorders were analyzed separately.
DiscussionThis study examined the effect of CBT on disgust reactions in a group of children with OCD and other anxiety disorders. In general, it was found that, regardless of anxiety disorder diagnosis, treatment with CBT was associated with a reduction in disgust reactivity. Additionally, no significant differences were found in disgust propensity between children with OCD versus other anxiety disorders prior to treatment. These data support previous research suggesting that disgust and related avoidance behavior is a higher-order feature of anxiety disorders.
Further, it was observed that children with OCD showed significantly greater reductions in disgust reactivity following treatment. Reductions in obsessionality appear to be most strongly associated with reliable change for disgust propensity, based on correlations between the RCI for the DES-C and the baseline CY-BOCS. Thus, these findings suggest that although the relevance of disgust to anxious psychopathology is not specific to OCD, the reduction of disgust propensity may be key in the treatment of this particular disorder.
Taken together, these results support previous research suggesting that disgust is related to the etiology, and therefore treatment, of anxiety disorders in general, and OCD in particular (Olatunji et al., 2011). The current findings also provide preliminary support for extending this theory to children. This is the first investigation that has evaluated the effect of CBT, indirectly, on disgust in a treatment-seeking sample of children with OCD and other anxiety disorders. Prior research has suggested that explicitly targeting disgust using exposure methods is associated with slower response, compared to fear, in individuals with OCD (McKay, 2006). The findings of the current study suggest that, in lieu of directly targeting disgust, symptom reduction may be achieved by alternatively targeting anxiety or other manifest symptoms. While the specific mechanism of exposure therapy is currently under contention (Craske et al., 2008; Kircanski et al., 2012), a reduction of disgust propensity could potentially signify habituation to disgust sensitivity (i.e., how distressing one finds the emotion of disgust; van Overveld, de Jong, Peters, Cavanagh, & Davey, 2006), or inhibitory learning of disgust reactions by reinforcing differential behavior associated with the previously disgusting stimuli.
While disgust propensity can be considered a higher-order factor for all anxiety disorders, it may be a more salient and critical treatment target when symptoms intersect with the core (e.g., blood-injection-injury phobias), animal-reminder (e.g., OCD with symptoms related to sex or bodily waste), and contamination (e.g., OCD with contamination symptoms, phobias of insects) domains (Olatunji, Ebesutani, Haidt, & Sawchuk, 2014; Olatunji et al., 2007). Though the results of this study showed global reductions in disgust propensity, the relatively small sample size did not allow for more nuanced examination of specific disgust domains or the influence of disgust sensitivity on anxiety symptoms. This study also did not assess associated behavioral avoidance due to disgust versus fear. Although previous studies have failed to show disgust to be specific to particular diagnoses and symptom domains (e.g., Berle et al., 2012; Muris et al., 1999; Woody & Tolin, 2002), Olatunji and colleagues (2014) assert that such a refutation cannot be made without sufficient assessment of potential domains of disgust expression, as was the case in this study.
Additionally, it is important to note that specific differences in the nature of disgust reactions between children and adults with anxiety disorders, and how they uniquely contribute to fear avoidance and disgust avoidance in each age group, are not yet well understood. Among adults, experimentally induced disgust leads to anxiety, regardless of whether stimuli are related to disgust or fear (Davey, MacDonald, & Brierley, 2008). This generalization of disgust across anxiety symptoms is mediated by negative interpretation biases (Davey et al., 2006), suggesting that disgust is implicated in the learning of avoidant behavior among adults. It is possible that children are prone to learning avoidant behavior in a similar fashion, wherein disgust leads to negative biases that maintain anxious avoidance of specific stimuli (Klein et al., 2014).
There are some important limitations to highlight in the present investigation. First, our conclusions regarding disgust reactions are based entirely on self-report assessment. While the instrument chosen, the DES-C, is the only available disgust assessment measure available for children, it remains unclear whether disgust reactions were alleviated in other response domains that may be more salient in the experience of the emotional state. For example, under conditions of exposure to previously feared situations, physiological arousal associated with disgust would be more relevant to potential avoidance reactions (Vrana, 2009). Physiological assessment under conditions of behavioral avoidance was not evaluated in this study, and would be warranted in future evaluations. In addition to this limitation, the sample of children with OCD was heterogeneous, with a range of primary symptoms of the condition. Future research should examine differential disgust reactions based on primary presenting symptom of OCD, given the range of disgust reactions associated with OCD (i.e., contamination fear; Olatunji, Moretz et al., 2010). Finally, it is unclear whether additional interventions that directly target disgust may augment CBT to provide further benefit for primary anxiety symptoms. While exposure appears to result in improvement, albeit slower than for other emotional states, recent analyses suggest other behavioral interventions may alleviate disgust responses (Mason & Richardson, 2012). Thus, future research should expand upon the results of this study by specifying particular disgust domains and behavioral avoidance responses associated with reductions in disgust reactivity following treatment both between OCD and other anxiety disorders, and also within the OCD diagnosis.
Available online 12 August 2014