Research has identified a wide range of psychosocial factors associated to choosing to engage in ongoing cancer screenings. Nevertheless, a systematic review of the theoretical frameworks and constructs underpinning studies on breast, cervical, and colorectal cancer screening participation has yet to be conducted. As part of the action-research project “Miriade,” the present study aims to identifying the main theoretical frameworks and constructs adopted in the literature over the past five years to explain cancer screening participation. According to the PRISMA guidelines, a search of the MEDLINE/PubMed and PsycINFO databases was made. Empirical studies conducted from 2017 to 2021 were included. The following keywords were used: breast OR cervical OR colorectal screening AND adhesion OR participation OR engagement AND theoretical framework OR conceptual framework OR theory. Overall, 24 articles met the inclusion criteria. Each theoretical framework highlighted clinical and psychosocial constructs of cancer screening participation, focusing on the individuals (psycho-emotional functioning and skills plan) and/or the health services perspectives. Findings from the present study acknowledge the plurality of the theoretical frameworks and constructs adopted to predict or promote breast, cervical, and colorectal cancer screening adhesion and the need for new research efforts to improve the effectiveness of cancer screening promotion interventions.
Cancer is one of the leading causes of morbidity and mortality worldwide (WHO, 2020). However, a substantial proportion of cancer diagnoses could be avoided and survival rates could be improved through the implementation of prevention strategies, such as cancer screenings. Cancer screenings entail detecting cancer at an asymptomatic stage of development (Ogden et al., 2012; Rex et al., 2000), identifing among apparently healthy people those who are at high risk, as well as to intervene early and more effectively.
Therefore, the healthcare systems worldwide are making efforts to ensure equity in access to timely, specialized, and free cancer screening programs. This is done by inviting the target populations to participate in tailored screenings programs that, according to the indications of the Ministry of Health, are for the prevention of breast, cervical and colorectal cancers. For the risk of breast cancer, women aged 50 to 69 are invited every two years for a bilateral mammogram; for the risk of cervical cancer, women aged between 25 and 64 are invited every three years to carry out Pap test or human papillomavirus [HPV] testing; for the risk of colorectal cancer, people from 50 to 74 years of age are invited every two years, without distinction of sex, to high-sensitivity fecal occult blood tests [FOBTs] or colonoscopy (WHO, 2020).
Although screening tests are undoubtedly advantageous for early cancer detection and treatment success, many people in the recommended age groups still do not (Gracie et al., 2016; Hart et al., 1997; Rex et al., 2000; USPSTF, 2021; Vernon et al., 1990). Therefore, research has increasingly explored factors influencing participation rates in screening programs (Authors, 2022), underlining a variety of barriers (Lim & Ojo, 2017; Klabunde et al., 2005) such as individuals’ lack of knowledge and awareness (Azubuike & Okwuokei, 2013; Elobaid et al., 2014; Mahalakshmi & Suresh, 2020), lack of physician recommendations (O'Malley et al., 2001) or lack of heterogeneous staff for gender and ethnicity (Alshahrani et al. 2019); health insurance status (Rodríguez et al., 2005), socioeconomic inequalities (Maheswaran et al., 2006), and difficult accessibility to locations (Chen et al., 2018). Furthermore, several studies have underlined the role of psycho-affective factors (Driedger et al. 2017; Harcourt et al., 2014) and meaning-making processes (Lemmo et al., 2020) in influencing cancer screening decisions, such as the emotional costs associated with specific tests, namely disgust (Kotzur et al. 2019), shame, embarrassment, discomfort, and fear (Blomberg et al., 2008; Ehrlich-Jones et al., 2021; Zorogastua et al. 2017). Fear is an emotion that crosses different levels: fear of screening in itself, previous negative experiences and fear for the results because many people consider cancer as a deadly diagnosis (Al-Azri et al., 2020; Bourdeanu et al. 2020). Nonetheless, although these studies have investigated cancer screening participation, they often lack a clear definition of the theoretical frameworks and psychological constructs driving the research, highlighting a more recent literature on the subject which is fragmented in the study of single determined factors or mediators (Authors, 2022). Historically the main theoretical models that study health behaviors are part of social cognition approach (Conner & Norman, 2015), applying the key cognitions and their inter-relationships in the understanding of health behaviors, as medical service usage for cancer screening. Changing attitudes toward cancer screening exams can increase the likelihood of obtaining a preventive test (Taylor, 2018). For example, according to the theory of planned behavior, women who have positive attitudes regarding mammography and who perceive social norms as favoring their obtaining a mammogram are more likely to participate in a mammography program (Montano & Taplin, 1991; Messina et al., 2004). Women who have positive attitudes, subjective norms (direct & indirect), and perceived behavior control were significantly associated with intention to cervical screen (Olgilvie et al., 2016). Furthermore, as is true of many health behaviors, beliefs predict the intention to participate in colorectal screening, whereas low SES or poor health status interfere with cancer screening access (Power et al., 2008). These historical theoretical models have encountered different evolutions and applications but to date there is no review work that collects the theoretical frameworks that guide the most recent studies on adhesion to cancer screening.
As it is known, the possibility to acknowledge and identify the theoretical frameworks and relevant constructs adopted to predict and improve cancer screening engagement would help to develop and adopt more effective theory-based intervention programs (Miche & Prestwich, 2010; Kelly et al., 1993). According to a large body of research, theory-based interventions can foster health-related choices and incentive in the promotion of screening coverage effectively (Kalke et al., 2020; Kreuter & Wray, 2003; Myers et al., 2007; Noar et al., 2007; Walsh et al., 2010; Savicka & Circene, 2020).
This study is part of a larger action-research project named MIRIADE - An Innovative Model of Research-Intervention for the identification of adherence profiles to cancer screening - founded by the Regional Prevention Plan (PRP Campania 2020-2025 Ministry of Health, Italy) with evidence-based healthcare action goals of improving cancer screening participation with theory-based intervention.
In this preliminary study, the following research questions have been proposed:
- (1)
What are the theoretical frameworks and their main theoretical constructs that have been used in the literature over the last five years for the study of cancer screening participation? (RQ1). What specific models are used for each type of screening: breast, cervical, and colorectal cancer screening? (RQ1.1).
- (2)
Regarding the theoretical constructs, which ones are useful for the study of participation in screening regardless of the type of tumor and which ones are useful for each type of screening? (RQ2).
By identifying a comprehensive set of theoretical frameworks and psychological constructs beyond single predisposing or hindering factors in the most recent studies on cancer screening engagement and addressing if they are specific for the type of screening (breast, cervical, colorectal cancer screening), this review could inform future research direction on what are the theoretical constructs to be integrated at the base of an intervention that aims to promote cancer screening engagement so as to develop theory-based screening program interventions.
MethodsThis systematic review was conducted following the procedure for the search and selection of studies set in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Page et al., 2021).
Search strategy and data collectionArticles were identified through a search of MEDLINE/PubMed and PsycINFO bibliographic databases using “breast OR cervical OR colon cancer screening” AND “adhesion OR participation OR engagement” AND “theoretical framework OR conceptual framework OR theory” as keywords. Articles were included if they met the following inclusion criteria: (1) they were empirical studies; (2) had a clear theoretical statement; (3) at least one of three cancer screening types was the subject of study; (3) were written in Italian or English; and (4) published between January 2017 and October 2021.
Regarding the fourth inclusion criteria, we justify the time frame (5 years) of our search. This review is preliminary study of MIRIADE project which is inscribed in the five-year period 2020–2025 because it is part of the Regional Prevention Plan 2020–2025, or the local response to the National Prevention Plan established by the Ministry of Health which sets different objectives for the relevant areas of Public Health, including implementation of cancer screening. With this systematic review we want to explore the state of the art of literature from the 5 years prior to the start of their project.
The exclusion criteria were as follows: (1) absence of full text; (2) systematic reviews/study protocols/dissertations; (3) articles about medical issues; (4) articles with other types of cancer (e.g., skin or lung); (5) articles developing intervention programs without a clear theoretical framework; and (6) articles with clear theories and theoretical frameworks but out of the topic “cancer screening behaviors.”
Firstly, individual titles were initially screened for relevance by two researchers and duplicate references were removed. Therefore, titles and abstracts were independently reviewed by two researchers. Afterward, a selected pool of articles was chosen for full-text reading and the final set of articles was established for inclusion in the systematic review. Before the final removal, any discrepancy or disagreement was solved by a discussion involving all the authors.
To identify the strengths and limitations of the selected primary studies, a quality assessment was made following the Mixed Methods Appraisal Tool version 2018 (Hong et al., 2018). Two authors (D.L., F.V.) reviewed all the articles and performed independent assessments of quality and eligibility with a result of 96% inter-rater agreement.
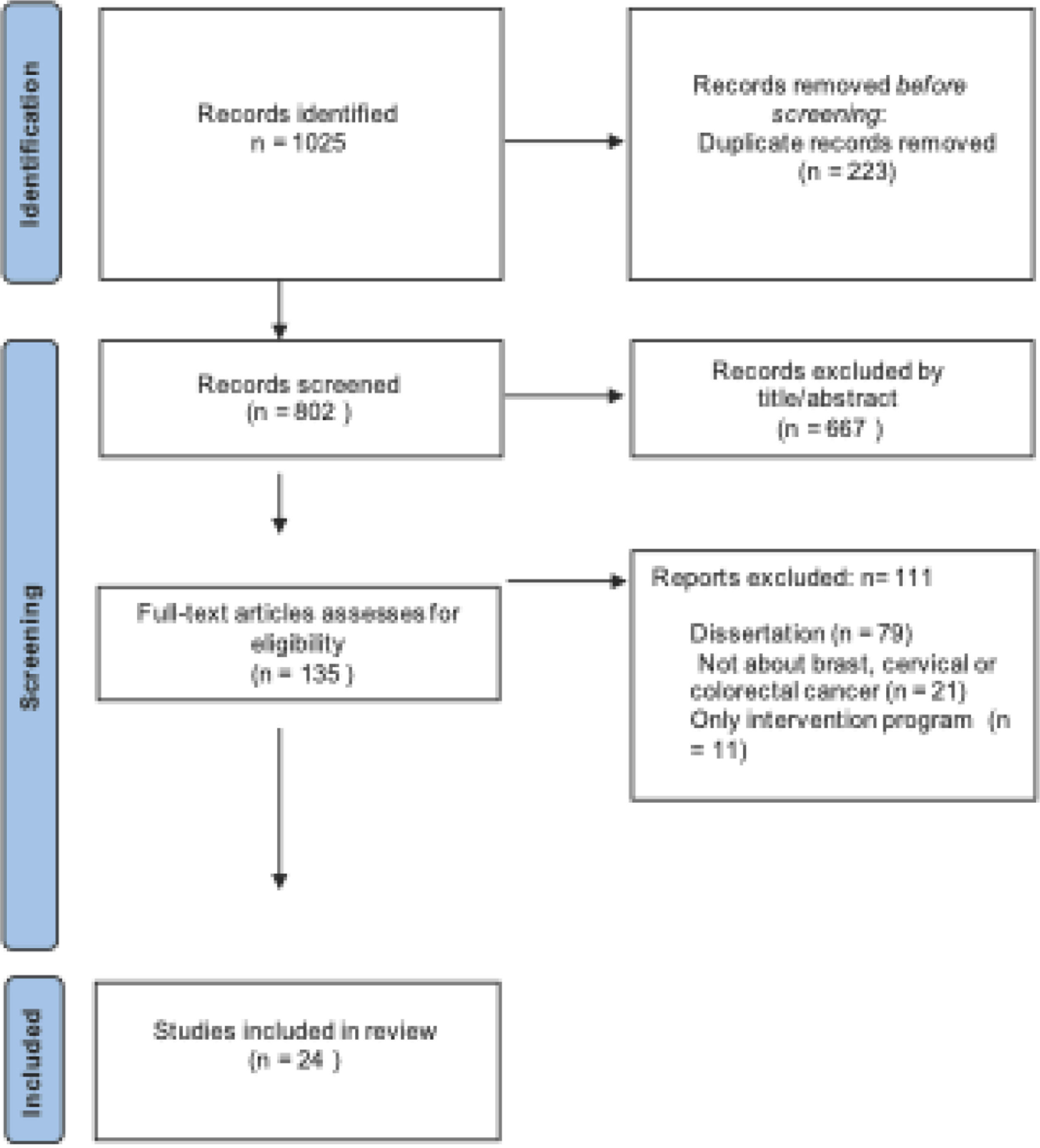
ResultsStudy selectionAltogether, 1025 records were identified, 223 of which were removed because they were duplicates. After assessing title/abstracts of individual citations, 667 of 802 records were removed as they were considered fully out of topic. Therefore, 135 articles were retrieved for further evaluation, 111 of which were excluded because they did not meet the inclusion criteria (e.g., dissertations; other types of cancer; intervention programs without theory). A total of 24 studies were included in the final analysis. Full details of the selection process are reported in Fig. 1 through a PRISMA flow diagram.
Results about research questions oneResponding to the first research question explanatory theoretical frameworks and their main theoretical constructs (RQ1) used in the literature over the last five years for the study of cancer screening participation were identified. 5 studies focused on the theoretical framework used to investigate participation in breast cancer screening, 12 focused on that used to investigate participation in cervical cancer screening, and 7 focused on the theoretical framework used to investigate participation in colorectal cancer screening.
In brief (see Table 1), all 24 studies specified at least one theoretical framework. Health Belief Model was the most frequently used (8 studies) both in the case of basic research and as theory-based interventions (Noman et al., 2020; Freund, Cohen, & Azaiza, 2017; Soonhee et al., 2018; Aldohaian et al., 2019; Ampofo et al., 2020; Akhagba, 2017; Fleming et al., 2018; Williams et al., 2018). It's followed by the Theoretical Domains Framework & COM-B Model (3 studies), model used for basic research (Oketch et al., 2019; O'Donovan et al., 2021; Dharni et al., 2017). One study (Lubi et al., 2021) reported using the Social practice theory and another (Aleshire et al., 2021) reported using the Penchansky and Thomas’ conceptualization of health care access. Protection Motivation Theory was used in two studies (Li et al., 2020; Malmir et al., 2018) and another two studies (Marlow et al., 2017; Ryan et al., 2019) used Precaution Adoption Process Model. One study (McQueen et al., 2019) based its intervention on Integrated conceptual model- impact of narratives in promoting cancer screening. 6 other studies (Brzoska et al., 2020; Qureshi et al., 2019; Attarabeen et al., 2018; Anurag et al., 2021; Le Bonniec et al., 2021; Woudstra et al., 2018) use each a theoretical model for basis researches: The Andersen Model of health service use; The ecological and Heron's six categories intervention framework; Self-regulation Model; Theory of Planned Behavior with cultural competency theory; Action control framework; Informed decision making and health literacy skills framework.
Theoretical frameworks and constructs for cancer screening participation in the studies analyzed (N = 24).
In the table for each model we report the main theoretical constructs that compose it.
Responding to the research question RQ1.1, only HBM is a transversal model for studying participation in all 3 types of screening. Theoretical Domains Framework & COM-B Model is the basis of studies for cervical and colorectal cancer. All the other models, as shown in the table, emerge as used in single types of screening.
Results about research question twoResponding to the second research question (RQ2), the constructs useful for studying participation in screening across the three types of screening and the useful constructs for each type of screening are identified.
In the three types of screening the transversal theoretical constructs used are: awareness, perceived barriers, and facilitators of cancer screening participation.
The construct of awareness in the preventive context is linked to that of cancer literacy (Soonhee et al., 2018) or knowledge and skills needed to find, understand, evaluate, and use the information and advices the health system has to offer regarding prevention, diagnosing, and treating cancer. This construct expresses the importance of knowledge, information about mammograms, and clinical breast exams, such as why they are important, what the process is, and current screening guidelines; that is, not so much to have information on cancer but information to address in community awareness programs. In fact, this represents an effective intervention key to educate women and specifically teachers who can in turn transmit knowledge (Noman et al., 2020).
However, it emerges that even if a woman is convinced of the benefits, this does not significantly predict participation in screening programs, just as motivation is not a significant determinant. On the other hand, the role that the perception of barriers plays in hindering participation in screening appears to be of importance.
The perceived barriers are also related to the cultural belonging of a woman such as to be configured as unique beliefs and individual perceptions. This construct is the basis of awareness-raising interventions aimed at improving knowledge and adherence to screening through a pre-packaged response script on perceived barriers of a religious and ethnic-cultural nature (Freund et al., 2017).
For migrant women, linguistic and sociocultural challenges, mainly cultural differences in the delivery of health services and in healthy recommendations (home versus host country), play a key role in influencing their acceptance and adoption of cervical cancer screening (Akhagba, 2017).
For women with obesity diagnosis, perceived barriers such as embarrassment with the gynecological examination or fear of patronizing behaviors from the general practitioner may hinder cervical cancer screening participation. Likewise, women with poor self-perceived health could perceive higher barriers to cancer screening uptake, as they may prioritize more urgent health issues over secondary prevention. In addition, a low education level and family history for cervical cancer were significantly associated with the belief of high susceptibility for developing cervical cancer (Aldohaian et al., 2019).
Overall, the use of promoters to deliver cervical cancer/HPV screening information and resources appears to be a favorable and realistic educational approach to improve and expand access and availability of culturally pertinent information and services to a particularly at-risk group (Fleming et al., 2018).
Considering the facilitators as a construct, research on colorectal screening behavior suggested that taking part in screening is a way of protecting own interests and of keeping healthy and screening participation represents a civic duty because not participating would be a waste of the NHS’ time and money (Dharni et al., 2017).
Regarding cervical cancer screening, research has underlined the following dimensions that significantly influence health outcomes and the desire to know one's HPV status: awareness and acceptability of HPV self-sampling; personal perception of cervical cancer risk; confidence in the ability to complete HPV self-sampling; peer and partner encouragement; privacy and comfort conducting the HPV self-sampling; and proximity to screening sites. Furthermore, the following specific barriers were identified: social stigma associated with cervical cancer; specific fears, including fear of pelvic exam and of disease and death (Oketch et al., 2019). Autonomous motivation was linked to positive screening behaviors. Deficits in physical and psychological abilities as inadequate coping skills were barriers to screening, while physical and social opportunity could facilitate participation. Older women raised age-related issues and had more negative attitudes to screening, while younger women identified practical barriers (O’ Donovan et al., 2021)
In breast cancer screening the main theoretical constructs are: habitual, emotional, and practical reasons and disparities of access . The final decision to participate in breast cancer screening is not only an individual behavioral act but also a health practice influenced by three major types of reasons, that is, habitual, emotional, and practical (Lubi et al., 2021).
The habitual patterns of communication with the medical system seem to significantly influence the way women perceive the activity related to the breast screening program. For example, in women's life, the easy health problems were not reasons to bother doctors, while screening actually means going to a doctor in the absence of symptoms. This aspect shows the importance of the cultural and societal aspect of the decision formation and expressed health practice, indicating that the acquirement of health practices starts with childhood and continues in an ongoing process during the lifespan.
The emotional aspects aggregate under this category different beliefs, fears, and cognitive reactions. The perception about one's health status, as “inner knowledge” or “gut feeling,” might play an important role in screening decision making. A special group of emotional reasons are related to different kinds of fears, especially with those related to the painful procedure of mammography. In addition to the fear against physical pain, it also may be that women are afraid to get emotionally hurt.
The practical aspects for deciding not to go undergo breast cancer screening are the fast rhythms of everyday life and obligations that make a screening activity low priority, just as the confusion on the booking procedures themselves or difficulties in the physical accessibility of the health service becomes significant.
Accessibility is a construct also used in the study of racial disparities in access to mammography screening for black women (Aleshire et al., 2021). Black women are more likely to distrust the health care system, and this distrust has been linked to decreased reporting of mammography barriers. Black women continue to lag behind in mammography screening. Multiple factors contribute to this disparity, and patient–provider communication and support as factors that could enhance the health care experience and result in a more trusting patient–provider relationship.
In cervical cancer screening the main theoretical constructs are: the threat and coping appraisal process, unawareness, diversity-sensitive services, and personal informed choice
To decide to carry out a pap smear, the threat assessment and personal coping process appears to be relevant constructs. It seems that women get more motivated to control the danger and accept the recommended responses when the perceived threat and efficacy are at a high level (Malmir et al., 2018). In other words, women are more probable to undergo screenings and to do pap tests if they logically address the benefits and understand the severity and harms of the disease as well as the associated consequences. In fact, perception, self-efficacy, and response efficacy of screening participations and the decrease in the perceived response cost (feeling embarrassed, anxiety, and impersonal about screening) are important for the evaluation of coping. The enhancement of women’ self-efficacy through the presentation of successful examples and the encouragement of those having regular screening participations were among the other aims of the current study, which led to the improvement (Li et al., 2020).
Still from a process point of view, specific attention was given to the study of women who do not participate in cervical screening and who can be differentiated into the following three types: unaware of screening, intending to have screening but were currently overdue, and who had decided not to attend. In these three cases, the majority of cervical cancer screening non-participants are not making an active decision not to attend but rather are either unaware or unable to act (Marlow et al., 2017). The lack of knowledge of the risk factors for cervical cancer—having many sexual partners, infection with HPV, or long-term use of the contraceptive pill—appears decisive in non-participation. Therefore, many women are not making an informed decision about non-participation and the screening information materials (Ryan et al., 2019).
Also, in the context of cervical cancer screening, the review shows a focus on specific populations, as migrant women. The implementation of diversity-sensitive services that aim at reducing disparities in access to cervical cancer prevention among migrant women (Brzoska et al., 2020) is fundamental. The lower utilization of healthcare services by migrant women—compared with non-migrant women—can be explained by the greater barriers migrants encounter in health care. Indeed, the health system is still not sufficiently sensitive to the needs and expectations of this population group. Implementing patient-oriented health care through diversity-sensitive health services is necessary to support informed decision making. This does not only include information taking into account the often times limited health literacy of this population group but also comprises information and services that consider their cultural needs and expectations.
For immigrant women in Norway, the construct of informed personal choice emerges, to be achieved with interventions aiming at promoting cancer screening adhesion, is that women could be interactive during the intervention (i.e., they can challenge the information being given to them). The intervention can be mainly seen as prescriptive and informative, as we tried to give the participants advice on the uptake of pap smear and objective information about the benefits of participating in the screening program and harms of non-participation and instructions on how to proceed. From the facilitative point of view, our intervention was mainly supportive and motivational, as we tried to answer questions and fears expressed by the women. As regards the cathartic and catalytic elements, we allowed the participants to express their experiences, anger, hesitations during the interactive meeting, and being judgmental in deciding whether to participate in the screening program or not. Through these elements we have tried in every possible way to encourage women to participate in the screening program without being authoritative or confronting, but helping them in making a personal informed choice for participation considering both the harms of not participating and benefits of participation (Qureshi et al., 2019).
In colorectal cancer screening the main theoretical constructs are: colon cancer worry, receptivity to fecal immunochemical test, individuals’ skills, and narrative influences
The colon cancer worry is not associated with screening participation, but it is associated with a generalized illness anxiety condition of the subject. However, this construct allows us to consider the emotional representation of colon cancer (Attarabeen et al., 2018). The participants reported they would experience depression and shock if diagnosed with cancer. In particular, colorectal cancer was associated with death, worries related to the necessity to wear a colostomy bag, and, social embarrassment. However, not only did colon cancer and its treatment produce negative associations but also the screening procedure entails several barriers; it was considered unpleasant, socially inconvenient, and embarrassing (e.g., pain; having areas of their body exposed).
Receptivity to the FIT (fecal immunochemical test) Kit screening was measured using a TPB framework that assessed attitudes, normative beliefs (norms), perceived behavioral control (PBC), and intention to be screened. This construct also appears associated with the perception of the healthcare provider cultural competency. Additionally, the intention to engage in FIT Kit screening has mediated a significant link between perceived cultural competence and acceptance of an offer to receive a free FIT Kit. Perceived cultural competence was most strongly connected to the intentions and screening behavior of the FIT kit through attitudes, although the links to normative beliefs were also significant. Curiously, although cultural competence was positively associated with PBC, we found no subsequent effect of PBC on FIT kit screening intentions or FIT kit request. In other words, racial minority patients who trust their health care providers to be more culturally competent may be more reassured to undertake thorough colorectal cancer screening options, and therefore, may have lower opinions on noninvasive screening options, including stool-based colorectal cancer screening (Dawadi et al., 2021). Intention-behavior profiles toward colorectal cancer screening in profiles could be differentiated on TPB (i.e., attitudes, subjective norms, PBC) and self-regulation variables (i.e., action planning, coping planning). Compared with nonintenders, successful and unsuccessful intenders reported a significantly higher level of subjective norms, PBC, and coping planning. Successful intenders also reported a significantly higher level of coping planning than unsuccessful intenders. However, successful and unsuccessful intenders could not be significantly differentiated on subjective norms and PBC (Le Bonniec et al., 2021).
From a health literacy skills perspective, so that the subject can make an informed decision linked to colorectal cancer screening, both operators and the target population undergo 8 decision-making stages and 10 key health literacy skills in colorectal cancer screening. The decision-making stages are as follows: (i) receiving invitation; (ii) recognizing decision; (iii) structuring decision options; (iv) delegating decision; (v) evaluating options based on facts and/or feelings; (vi) making a decision; (vii) participating or not; and (viii) interpreting result. The health literacy skills were as follows: skills in accessing, understanding, deriving meaning, appraising information, communicating, weighing up pros and cons, using information, following instructions, and translating decisions into actual participation.
Lastly, to increase colorectal cancer screening uptake, narrative intervention may have advantages over didactic information. In particular, survivors’ narratives (compared with those by the screeners) elicited greater emotional involvement, and increased negative affect and concern linked to screening. This resulted in a greater intention to participate in cancer screening; nevertheless, greater negative effect was also associated with less self-efficacy, the latter being a strong predictor of screening intention. It was the stories of the screeners that spurred more self-referential engagement, which reduced the counter-arguments that helped mitigate its negative influence on screen intentions (McQueen et al., 2019).
DiscussionThe review highlights that the literature in the last 5 years has used a considerable plurality of theoretical frameworks and constructs useful to explain cancer screening participation.
We can organize the theoretical models that emerged from the review into three main/core assumptions: behavioral models; functioning and process models; health cultural models.
In the first core assumption are considered social and cognitive mechanisms behind preventive choice and health service use, mainly used for the study of participation in cancer screening, regardless of specific cancer. In the second core assumption there are the models which highlights preventive engagement process in taking care of oneself, in the decision-making and in the relationship with health professionals. In the third core assumption the models look to the individual as an agent in a culturally defined world where preventive practices are intertwined with representations and cultural differences and participation in screening can represent a civic duty. The knowledge in the field of the theory can be useful to form the basis of future cancer screening interventions (Hagger & Weed, 2019).
Looking specifically at results for each single type of cancer screening, we can instead highlight two aspects.
As a first aspect, we highlight that 12 studies have emerged for cervical cancer screening as compared to the 7 for colon cancer screening and 5 for breast cancer screening. This is probably because cervical cancer has been ranked as the second most incident gynecological cancer and the leading cause of cancer-related death among women worldwide, where coverage of the target population ranges from about 25% to 80% (WHO, 2022). We also think of the breadth of the age group to which gynecological screening is aimed, embracing the entire span of a woman's life, all biological and psychosexual life stages. A smaller number of studies emerge for breast cancer screening as the literature has probably dealt with this type of screening in previous years or using studies that often arose in the context of the medical field or were carried out by multidisciplinary teams that aimed to purely investigate the role of psychological variables, without defining and adopting a conceptual model/framework to approach the topic from a psychological perspective.
We also think of the difference of organs and parts of the body to which these screenings refer: breast external and visible, cervix and colorectal, internal and invisible organs that perhaps require the development of greater criteria for understanding development of clearer theoretical perspectives (Lemmo et al., 2020).
With respect to the number of articles found, the possible limits of the search must also be considered: due to the several and heterogeneous words used in the cancer screening literature, it was difficult to define search terms to capture all relevant papers. Although searches were kept broad—with extensive hand searching of reference lists—to capture a wide range of articles, the search terms could have included terms such as “adherence” OR “intention” OR “motivation” AND “breast” OR “cervical” OR “colorectal cancer screening.” However, subsequent readings of these results did not seem to make a difference on the final set of papers chosen for inclusion. The review only included published papers, which did not capture potentially meaningful sources of information such as dissertations, conferences abstracts and official reports. The review only included studies published starting from 2017, and this may have been a source of bias.
As a second aspect, we highlight the multiplicity of theoretical models (6 different models for 7 studies in total) used to study colorectal cancer screening behavior. First of all, colorectal screening is of recent onset as a health practice compared to the other two types of screening. Therefore, we think that in the last 5 years the literature has had the need to apply different models in this field. In fact, the TPB, a framework particularly used in screening behaviors, emerges in this review only applied to the colorectal cancer screening.
In this context, a key role is given to understanding the relationship between intention and behavior, a privileged object of TPB studies. This axis of understanding can allow research to outline profiles of subjects who intend and do not intend to carry out screening actions.
Moreover, probably this type of prevention is more complex than the other two in examination procedures and in fear of colon cancer.
Looking at the specificity of the theoretical constructs used for each type of screening we highlight that as regards breast cancer screening, it is suggested to evaluate preventive actions as a social practice, rather than only a subjective choice. Indeed, preventive actions need to be conceptualized and implemented “at the meeting point” between the citizens’ demand and the supply of preventive health services.
As regards cervical cancer screening, the studies dedicated to understanding the phenomenon of participation have attached importance to the individual processes of assessing the threat and the possible coping response, adaptive or maladaptive. The procedural perspective has also allowed us to identify different cognitive and behavioral phases determined by facilitating or hindering factors.
In particular, in the context of gynecological screening, the lack of awareness, rather than being linked to the screening activity, is linked to risk factors such as sexual infections and therefore unprotected sexual relations. Furthermore, the informed choice is aimed at regulating the accessibility of health services, taking into account the needs of women. Indeed, cancer screening has been described as a “teachable moment” (Senore et al., 2012). This definition discloses the opportunity to foster a more effective delivery of cancer prevention advice and interventions.
As regards to colorectal cancer screening, understanding of participation through studies that focus on the interaction of the cognitive and emotional representation of the disease as well as the relationship between concern and risk as aspects of self-regulation. Furthermore, the need for individuals to possess health literacy skills to make informed decisions is highlighted.
ConclusionFrom the results, it appears clear that the implementation of an individualistic approach is not sufficient to bring along desired preventive choices. All groups of reasons, individual, relational and social context are involved in the decision-making process. To develop successful interventions to improve participation in the context of cancer screening, the need to use theory in the design of the intervention that aims at cognitive and behavioral constructs, aims at social influences, the emotional aspects of the subject and accessibility and acceptance of the context is evident.
We think it is useful to consider the development of an interpretative reading that considers them as psychological functioning axes to be considered in an integrated manner in understanding the phenomenon of participation in cancer screening.
The cognitive and emotional representation of the disease and of the investigation tests allows us to focus on aspects of self-regulation in the individual process of making preventive choice which also implies the assessment of the sense of threat and of one's own adaptive or maladaptive responses. These aspects, combined with the perception of one's own motivations, the barriers of the context, the criteria for accessibility to health services, the quality of the health relationship in the decision-making process lead to the possibility of working on preventive processes. Also, we highlight the necessity to take into account the emotional aspects entailed within healthy choices.
In summary, the findings from the present review have suggested the necessity to address regulatory cognitive and emotional processes, and that simultaneously considers individuals and relationships within the healthcare services usage.
From this point of view, although people are pushed to become owners and managers of their own well-being and self-care, health services are still necessary to effectively support people in health-related decisions. Therefore, public health campaigns and education should carefully consider not only the individualistic and tailored approach to health care, but also the “institutional” role of health services in influencing healthful choices.
Empower individuals and empower healthcare contexts, personalizing promotion and access on the basis of psychosocial profiling of the target subjects to whom the programs are aimed, is an important research efforts to improve the effectiveness of cancer screening promotion interventions.