Background/Objective: Alzheimer-type dementia is one of the most frequent causes of dependence in an aging population, which combines with a considerable demand for care. Furthermore, when the caregiver is a family member or person without specialized training, such care impacts on that person's health. The Inventory of Overburden in Alzheimer's Patient Family Caregivers with no Specialized Training (IPSO-CA24) was designed to find out the needs of these caregivers and evaluate the caregiver's burden or distress. Method: The psychometric properties of the questionnaire were analyzed (in a reliability analysis, exploratory factor analysis and confirmatory analysis) based on the responses of 255 caregivers. Results: The factor analyses showed a six-factor structure (Reaction to diagnosis, Physical health, Psychological symptomatology (caretaker), Behavioral symptomatology (patient), Knowledge of the illness, and Level of dependence) explaining 66.52% of the total variance with a reliability of .75 to .93. Support was also found for its convergent validity. Conclusions: The IPSO-CA24 responds to the need for an instrument enabling multidimensional evaluation of the burden on the family caregiver without specialized training.
Antecedentes/Objetivo: La demencia tipo Alzheimer es una de las causas más frecuentes de dependencia en población mayor, a lo que se une, la considerable demanda de cuidados. Además, cuando el cuidador es un familiar o una persona sin formación especializada, el cuidado tiene un impacto sobre su salud. Para conocer las necesidades de estos cuidadores y evaluar el nivel de sobrecarga o malestar del cuidador, se realiza la propuesta del Inventario de Sobrecarga en Cuidadores Familiares sin Formación Especializada de Enfermos de Alzheimer (IPSO-CA24). Método: En base a las respuestas de 255 cuidadores, se analizaron las propiedades psicométricas del cuestionario, mediante análisis de fiabilidad, análisis factoriales exploratorios y confirmatorios. Resultados: Los análisis factoriales informan de una estructura de seis factores relacionados (Reacción ante el diagnóstico, Salud física, Sintomatología psicológica (cuidador), Sintomatología conductual (enfermo), Conocimientos de la enfermedad y Nivel de dependencia), con una fiabilidad entre 0,75 y 0,93, que explican el 66,52% de la varianza total. También se obtiene apoyo para su validez convergente. Conclusiones: El IPSO-CA24 viene a dar respuesta a la necesidad de un instrumento que permita una valoración multidimensional de la sobrecarga del cuidador familiar sin formación especializada.
At the present time, Alzheimer-type dementia continues to be one of the most frequent causes of dependence of the older population, posing a challenge for public health (World Health Organization & Alzheimer's Disease International, 2012), and therefore, requiring coordinated worldwide action by responsible agencies (Prince et al., 2015) (World Health Organization, 2015). According to recent reports (Alzheimer's Association, 2016), caregivers of Alzheimer's Disease and other dementia patients provide continued attention during a longer period than caregivers of persons who are dependent for other causes. The considerable demand on caregivers of a dependent relative, for example, on the activities of daily life (Gázquez, Pérez-Fuentes, Mercader, & Molero, 2011) have negative consequences to the health of the caregiver (Berglund, Lytsy, & Westerling, 2015) and their quality of life (Díaz-Prieto & García-Sánchez, 2015; Flores, Jenaro, Moro, & Tomşa, 2014). The volume of research work analyzing the profile of the family caregiver has multiplied in recent years (Brown & Brown, 2014) mediated by the boost in quality of publications in social sciences (García-Pereira & Quevedo-Blasco, 2015). In this field, the concept of caregiver burden is of special interest and requires conceptual and dimensional consensus. However, Martín-Carrasco, Domínguez-Panchón, Muñoz-Hermoso, González-Fraile, and Ballesteros-Rodríguez (2013) warned that the burden on the family caregiver is being evaluated from different approaches, impeding comparison of the results of research.
Since the first definition of caregiver burden (Grad & Sainsbury, 1963), many attempts have been made at delimiting the concept using different models to include its possible dimensions. Poulshock and Deimling (1984) proposed a multidimensional approach to this burden, where different dimensions were interrelated (patient problems, burden and its impact on the caregiver). Montgomery, Stull & Borgatta (1985) differentiated between the “objective burden” or facets related to caregiving, and “subjective burden” or the caregiver's perception of the impact the objective burden has on their physical, psychological and social condition.
Caregiver stress is often considered a powerful predictive factor of burden. The Transactional Model of Stress and Coping by Lazarus and Folkman (1984) established a relationship between the caregiver's evaluation of the situation (demand) and their ability to cope with it. In other cases, the caregiving burden is related to the patient's problems and deterioration. Pearlin, Mullan, Semple, and Skaff (1990) defined burden as the caregiver's subjective evaluation of the objective demands made by the patient (patient's physical and cognitive deterioration, functional disability and behavioral problems). Later, Sandín (1999), in his stress process model, included variables that maintain a modulating function of the response to stress, among them, psychosocial demands and state of health. In other dependent populations, daily stress is referred to as a risk to mental health (Schönfeld, Brailovskaia, Bieda, Zhang, & Margraf, 2016). Several personal resources having a protective effect against the negative influence of stress on family caregivers have been identified (Gázquez, Pérez-Fuentes, Molero, & Mercader, 2015; Lanzón & Díaz, 2015; Otero-López, Villardefrancos, Castro, & Santiago, 2014).
The goal, as stated by Zarit, Femia, Kim and Whitlatch (2010), should therefore be to design evaluation instruments which fit to the caregiver's reality and enable intervention to be directed at specific targets, and not a generic problem, which is only theoretically common to all caregivers. Thus, the heterogeneity of the caregivers’ profiles and their needs (Rosa et al., 2010) requires studies testing intervention effectiveness (Chacón, Sanduvete, Portell, & Anguera, 2013) and the inclusion of new therapeutic variables (Bornas, Noguera, Pincus, & Buela-Casal, 2014; Vives, Orte, & Sánchez, 2016). Along this line, a model is proposed that sustains the development of an evaluation instrument for the specific needs of the Alzheimer patient family caregiver (Pérez-Fuentes et al., 2014). A series of factors has to be taken into account for the early detection of stress or burden in this specific caregiver profile. On one hand, caregiver-related factors, such as reaction to the diagnosis (feelings), physical health and knowledge of the disease, and on the other, patient-related factors, such as level of dependence, and, finally, emphasize special attention to the symptomatology, which in this case, is a two-dimensional factor, caregiver psychological symptomatology and patient behavioral symptomatology.
In absence of patient treatment, one of the concerns which caregivers often refer to is the difficulty in diagnosing dementia early. This could have a significant impact on the emotional response of caregivers, and therefore, on caregiving quality (Caron & Caron, 2011). De Vugt and Verhey (2013) believe that early diagnosis offers the opportunity of advancing in the process of adapting to the role of caregiver. Thus caregivers most able to adapt to the changes typical of dementia feel more competent to care for them and experience fewer health problems. According to Boots, Wolfs, Verhey, Kempen, and de Vugt (2015), early intervention helps caregivers to identify their needs and increase their knowledge of the changing roles in the relationship, preventing overburdening. The use of certain coping strategies by patients and their relatives facilitates decision-making after diagnosis which will affect later adjustment of caregiving (Bronner, Perneczky, McCabe, Kurz, & Hamann, 2016).
After the critical moment of the diagnosis, the caregiver often experiences feelings of doubt and unease, especially due to ignorance of the illness and caregiving required (Rosa et al., 2010). In this situation, the caregiver's previous beliefs and expectations may influence the feeling of burden positively or negatively. Feldberg et al. (2011) suggested that the more negative the caregiver's beliefs are, the higher the probability of their experiencing overburdening and therefore, becoming more vulnerable to stress and anxiety. Training caretakers in symptomatology and the evolution of the disease, or in handling daily situations, could reduce overburden and even avoid its appearance (Lima-Rodríguez, Lima-Serrano, & Domínguez-Sánchez, 2015; Saavedra, Bascón, Arias, García, & Mora, 2013). Molinuevo and Hernández (2011) thought evolution of the patient's behavioral symptomatology is another of the factors determining how the caregiver copes with caregiving and the burden generated by it. Corazza et al. (2014) found a positive correlation between the caregiver's feeling of burnout and neuropsychiatric distress of the Alzheimer's patient. There has been a trend in recent years to analyze the relationship between patient characteristics and caregiver burden (Lou et al., 2015). Along this line, Peña-Longobardo and Oliva-Moreno (2015) found that the probability of the family caregiver having problems (health, professional and leisure) is associated positively with the degree of patient dependence. Rogero-García and Ahmed-Mohamed (2014) thought perception of uncovered needs is related to the characteristics of the dependent person, the caregiver and the caregiving context. Thus such aspects as the impact caregiving has on the health of the caregiver (Fernández de Larrinoa et al., 2011) are being evaluated. Delgado et al. (2014) found a worse state of health, heavier demand on healthcare services and use of medication by family caregivers. Recently, higher mortality rates have been shown in family caregivers, although with a slight decrease in recent years (Roth, Fredman, & Haley, 2015). Precisely because of the caretaker's fatigue, the concept of caregiver burnout is being reexamined, which in spite of being a term used in the scope of healthcare to refer to professional stress in their daily work, in the case of family caregivers, it could be performing the same function (Da Silva, Braga, & Da Silva, 2009). The study by De Valle-Alonso, Hernández-López, Zúñiga-Vargas, and Martínez-Aguilera (2015) found that overburden was a predictor of burnout in family caregivers of elderly patients, although neither the personal characteristics nor conditions of caregiving were directly related to level of burden.
In parallel to the concept of evolution, several instruments have also been designed to assess caregiver burden in the area of evaluation (Crespo & Rivas, 2015). Sometimes, classification of these tests depends on what they are measuring: a) one-dimensional, such as the Burden Interview (Zarit, Reever & Bach-Peterson, 1980), the Caregiver Strain Index (Robinson, 1983) or the Caregiver Perceived Burden (Strawbrigde & Wallhagen, 1991); two-dimensional, such as Montgomery's Burden Scale (Montgomery, Goneya, & Hooyman, 1985); and multidimensional, such as the Caregiver Appraisal Scale (Lawton, Kleban, Moss, Rovine, & Glicksman, 1989), the Caregiver Burden Inventory (Novak & Guest, 1989) or the Questionnaire on Resources and Stress (Holroyd, 1987). Although a diversity of instruments are used to determine the level of caregiver burden, preference for the use of the one by Zarit et al. (1980) has been continuous since the nineties (Martos et al., 2015). Another instrument which should be pointed out is the Caregiver Burden Inventory (Novak & Guest, 1989), which although it has no Spanish adaptation, is one of the most commonly used.
On top of the few tests developed or adapted for the Spanish population, authors such as Garand et al. (2013) say that interventions carried out are directed basically at caregivers who already have heavy burdens, but that intervention for so-called “new caregivers” is also necessary, that is, preventive intervention for caregivers of recently diagnosed patients. Thus the purpose of this study, from this perspective, was to validate an instrument for early detection of the needs of Alzheimer's patient family caregivers without specialized training, which would evaluate the needs for intervention in the family caregiver without specialized training and enable design of early intervention to avoid overburden of the caregiver.
MethodParticipantsThe sample was selected from the medical histories in the database of the Andalusian Healthcare Service Family Caregiver Attention Plan, 843 of whom were Alzheimer's patients. Of these, those who were not part of the target population, for example, who were in an advanced stage of the disease, were eliminated, and patients who had ortho-prosthetic devices at home were also discarded. The final population consisted of 507 family caregivers of patients with Alzheimer's in its early or moderate stages. Of these, participants were chosen at random from the various Basic Healthcare Districts in Almeria, leaving a study sample of 255 caregivers (95% confidence level and confidence interval of 4.33%), all of whom were family caregivers of patients diagnosed with Alzheimer's Disease. Of this sample 85.7% were women and 14.3% were men, with a mean age of 55.39 years (SD=12.41). Of the persons cared for, 57.6% were in a moderate stage of the disease (Stage II), while 42.4% were in an early stage (Stage I). With regard to the first variable, 63.9% of the caregivers were sons/daughters, 26.7% were spouses, 2.7% were sons/daughters-in-law, 1.2% were siblings and 15.5% were other relatives.
Instruments- -
Ad hoc questionnaire on sociodemographic data such as age, sex, stage of disease (Early or Moderate), relationship (son/daughter, spouse, son/daughter-in-law, sibling, other relative).
- -
General Health Questionnaire by Goldberg (GHQ-28) (Lobo, Pérez-Echeverría, & Artal, 1986). The GHQ-28, in addition to measuring perceived health and emotional wellbeing, detects both recent and chronic health problems. It consists of a total of 28 items distributed in four components (depression, anxiety, physical social dysfunction symptoms) with seven items each and with a Cronbach's alpha of .86, .89, .70 and .87, respectively.
- -
Índice de Esfuerzo del Cuidador [Caregiver's Effort Index] (López & Moral, 2005). This assesses the burden and effort of caregiving based on 13 items. Validation of the instrument for the Spanish population found a Cronbach's alpha of .80, and in this study it was .75.
- -
Barthel Scale (Baztán et al., 1993; Mahoney & Barthel, 1965). This questionnaire has 10 items designed to assess the functional independence/dependency in performing basic daily activities. A low score indicates a high level of dependency. Internal consistency showed a Cronbach's alpha of .86-.92 in the original version and .93 in this sample.
- -
Inventario de Sobrecarga en Cuidadores Familiares de Enfermos de Alzheimer [Inventory of Overburden in Alzheimer's Patient Family Caregivers with no Specialized Training] (IPSO-CA38). Its construction followed the model proposed by Pérez-Fuentes et al. (2014) with 38 items on aspects to be found included in six factors: Reaction to diagnosis (Feelings), Physical health, Psychological Symptomatology (Caregiver), Behavioral Symptomatology (Patient), Knowledge of the disease and level of dependence. The response choices are on a four-point Likert-type scale from 1=Not at all to 4=A lot.
When permission had been requested from the Almeria Healthcare District Research Committee and the corresponding Research Ethics Committee, the staff in charge of implementing the questionnaires met and was informed of how to proceed with each subject. Thus each of the caregivers was informed about the purpose of the study, the confidentiality of the data and filled in the required informed participation consent form. First the target group for instrument design was formed, and all the points indicated by the caregivers were included in a pilot version, and that first 38-item version of the IPSO was given to 20 caregivers to evaluate their understanding of the items. Interrater validation was also carried out (by four specialists) to analyze the theoretical-logical domain. When the modifications had been made as suggested by both groups, the final version of the IPSO was drafted. It was then given individually in a structured interview lasting from about ten to fifteen minutes.
Data analysisThis is a descriptive cross-study in which the descriptive data and reliability were calculated using SPSS.22 (2013) and confirmatory factor analysis was done with AMOS.22 (2013). The analysis was done in three steps. First reliability and validity of the original 38-item IPSO-CA38 model were analyzed. Then, because reliability and goodness of fit were unacceptable, errors causing the lack of fit were analyzed by reliability analysis of each item, measurement error, estimation error and correlated measurement errors. Based on the analysis of these indicators, the number of items in the inventory was reduced to 24, for which descriptive and reliability analyses were done before confirmatory factor analysis. In a third step, fit of this reduced 24-item version of the inventory (IPSO-CA24) with six factors (maintaining the model proposed by Pérez-Fuentes et al. (2014) in two ways, with and without a general overburden index. To determine the degree of fit of the models, the statistics and indices most commonly used for this were calculated: χ2, χ2/df (degrees of freedom), Adjusted Goodness-of-Fit Index (AGFI), Comparative Fit Index (CFI), and Root Mean Square Error of Approximation (RMSEA).
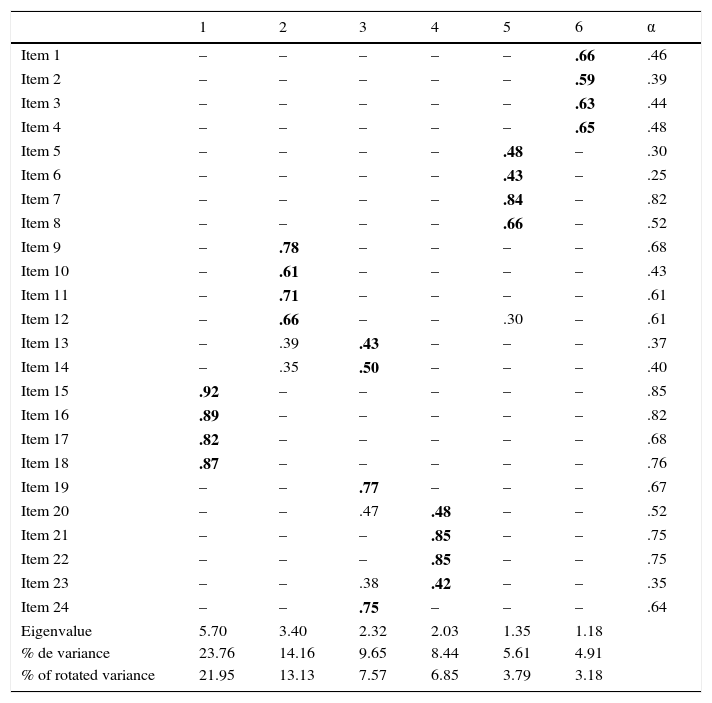
ResultsDescriptive statisticsThe correlations of the 24 items in the reduced version of the Inventory of Overburden in Alzheimer's Patient Family Caregivers with no Specialized Training (IPSO-CA24), and the means, standard deviations, asymmetry and kurtosis are shown in Table 1. It may be observed that most of the correlations are statistically significant and kurtosis and asymmetry of each variable are acceptable, so the use of the method of maximum similarity seems justified for estimating the model's goodness of fit. Furthermore, exploratory factor analysis was performed using maximum likelihood with oblique rotation, for which the KMO coefficient was .82 and Bartlett's sphericity test found χ2=2916.33, which is significant with 276 degrees of freedom (p<.001). As shown in Table 1, six factors explained 66.52% of the variance, where Factor 1 had the most weight, although the rest of the factors had saturations over .40. In addition, the percentage of variance explained by Factor 1 Knowledge of the disease, which is comprised of four items, is slightly higher than the rest (23.76%).
Matrix of rotated components (IPSO-CA24).
| 1 | 2 | 3 | 4 | 5 | 6 | α | |
|---|---|---|---|---|---|---|---|
| Item 1 | – | – | – | – | – | .66 | .46 |
| Item 2 | – | – | – | – | – | .59 | .39 |
| Item 3 | – | – | – | – | – | .63 | .44 |
| Item 4 | – | – | – | – | – | .65 | .48 |
| Item 5 | – | – | – | – | .48 | – | .30 |
| Item 6 | – | – | – | – | .43 | – | .25 |
| Item 7 | – | – | – | – | .84 | – | .82 |
| Item 8 | – | – | – | – | .66 | – | .52 |
| Item 9 | – | .78 | – | – | – | – | .68 |
| Item 10 | – | .61 | – | – | – | – | .43 |
| Item 11 | – | .71 | – | – | – | – | .61 |
| Item 12 | – | .66 | – | – | .30 | – | .61 |
| Item 13 | – | .39 | .43 | – | – | – | .37 |
| Item 14 | – | .35 | .50 | – | – | – | .40 |
| Item 15 | .92 | – | – | – | – | – | .85 |
| Item 16 | .89 | – | – | – | – | – | .82 |
| Item 17 | .82 | – | – | – | – | – | .68 |
| Item 18 | .87 | – | – | – | – | – | .76 |
| Item 19 | – | – | .77 | – | – | – | .67 |
| Item 20 | – | – | .47 | .48 | – | – | .52 |
| Item 21 | – | – | – | .85 | – | – | .75 |
| Item 22 | – | – | – | .85 | – | – | .75 |
| Item 23 | – | – | .38 | .42 | – | – | .35 |
| Item 24 | – | – | .75 | – | – | – | .64 |
| Eigenvalue | 5.70 | 3.40 | 2.32 | 2.03 | 1.35 | 1.18 | |
| % de variance | 23.76 | 14.16 | 9.65 | 8.44 | 5.61 | 4.91 | |
| % of rotated variance | 21.95 | 13.13 | 7.57 | 6.85 | 3.79 | 3.18 |
Note. Extraction method: Principal axis factoring. Rotation method: Equamax. Rotation converged in seven iterations.
Internal consistency of the inventory is good (α=.85), and also of each of the scales: Reaction to diagnosis (Feelings) α=.75; Physical health α=.75; Psychological symptomatology (Caregiver) α=.84; Behavioral symptomatology (Patient) α=.77; Knowledge of the disease α=.93; and Level of dependence α=.79.
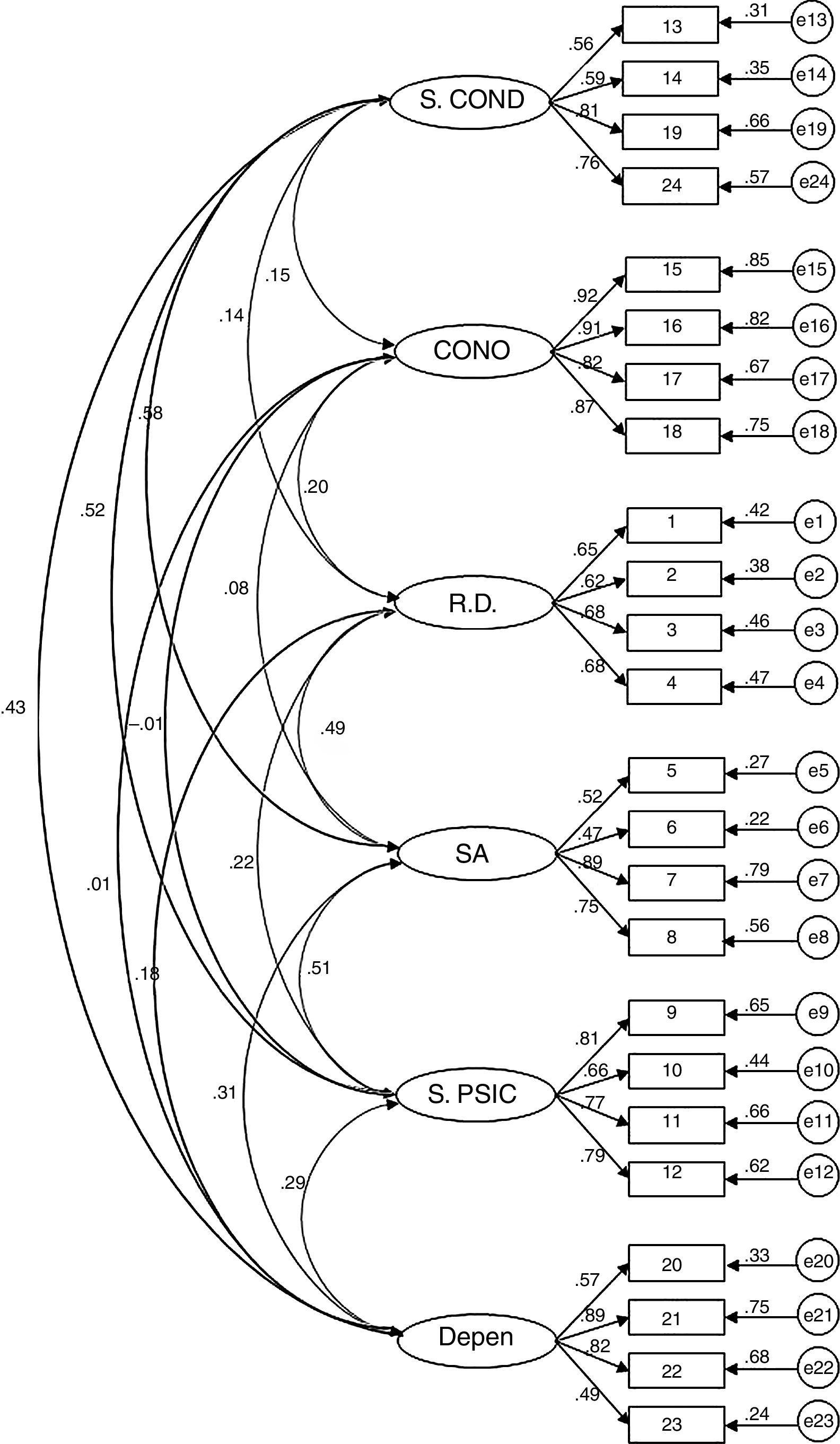
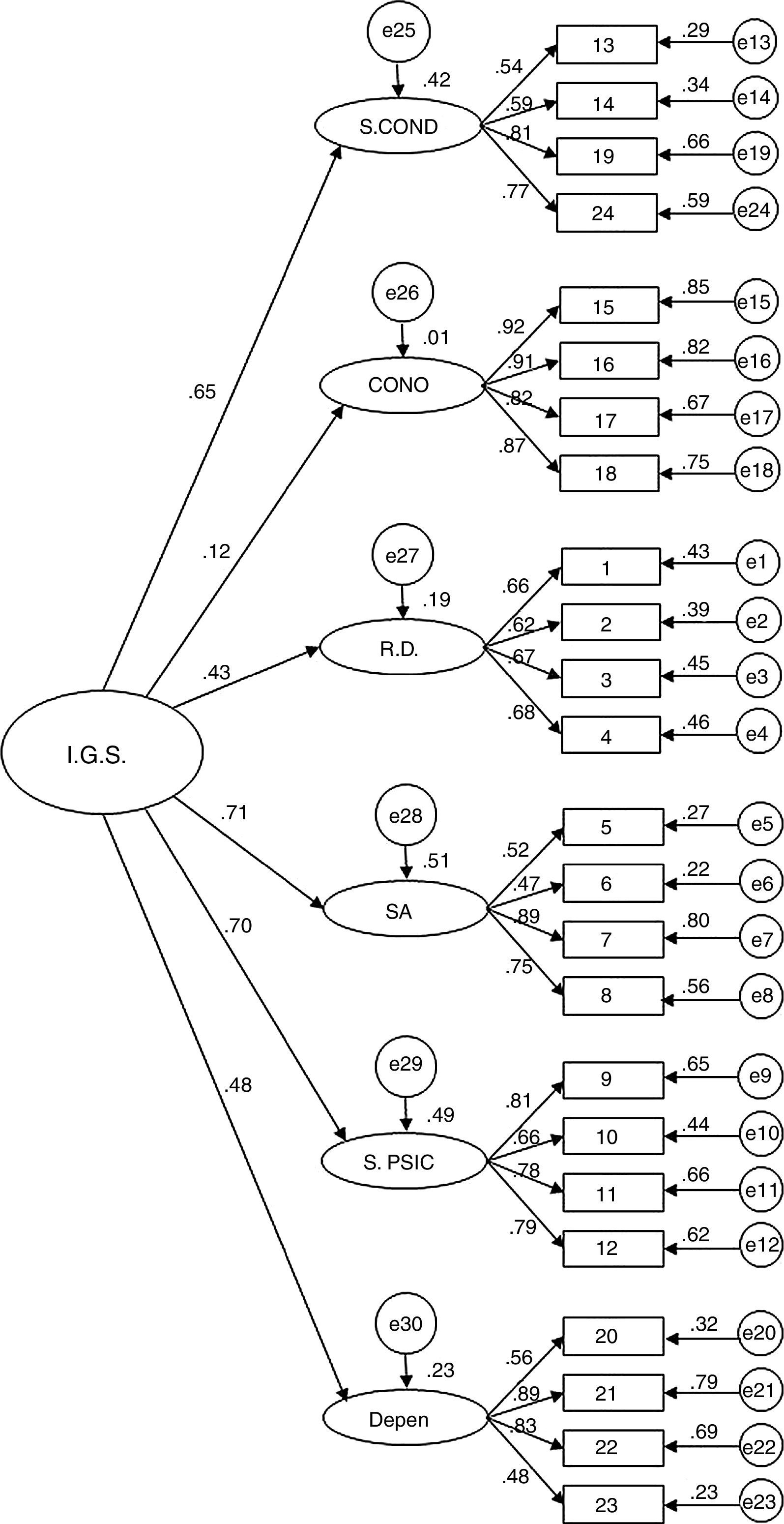
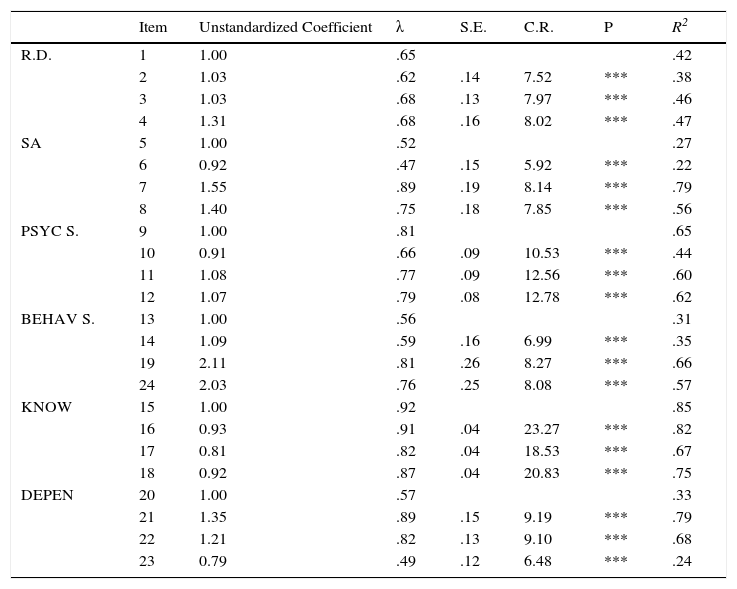
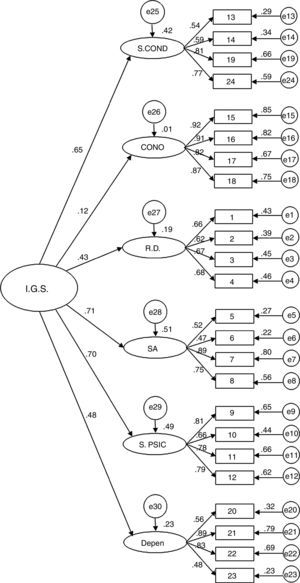
Confirmatory Factor AnalysisAfter checking that asymmetry (-1.4–1.2) and kurtosis (-1.3–.1) were adequate, the structure of the questionnaire was evaluated by comparing goodness of fit of the two alternative models, one model with six first-order factors (Model 1) and a model with a hierarchical structure (six first-order factors and a general second-order factor) (Model 2). The results show that both models have similar fit (Model 1: χ2=458.56; df=237; p < .001; χ2/df=1.94; GFI=.87; AGFI=.83; CFI=.92; RMSEA=.06 (.05-.06; p < .05); Model 2: χ2=498.52; df=246; p<.001; χ2/df=2.02; GFI=.86; AGFI=.83; CFI=.91; RMSEA=.06 (.05-.07; p<.01)). Although at first Model 1 seemed to show better fit, the models are nested and their fit can be compared statistically. The result of this test shows the existence of significant statistical differences in the fit of the two models (Δχ2=4.44; p<.001). Therefore, based on this statistical criterion and parsimony, Model 1 was selected as the best for representing the structure of the IPSO-CA24. Specific fit of Model 1 is modest or acceptable, depending on the criterion used (acceptable if going by χ2/df, CFI or RMSEA; modest if using GFI or AGFI). In any case, it should be considered that the fit of this type of instruments (self-report) is difficult to optimize without estimating the correlations of the measurement errors (which are common, both from the effect of the method of accessing information in itself and how some of the items are written). Therefore, and keeping in mind that in estimating the model's goodness of fit these covariates were not included, it is possible to assume that goodness of fit of Model 1 is acceptable (Figures 1 and 2, Table 2).
Goodness of fit of the IPSO-CA24 model.
| Item | Unstandardized Coefficient | λ | S.E. | C.R. | P | R2 | |
|---|---|---|---|---|---|---|---|
| R.D. | 1 | 1.00 | .65 | .42 | |||
| 2 | 1.03 | .62 | .14 | 7.52 | *** | .38 | |
| 3 | 1.03 | .68 | .13 | 7.97 | *** | .46 | |
| 4 | 1.31 | .68 | .16 | 8.02 | *** | .47 | |
| SA | 5 | 1.00 | .52 | .27 | |||
| 6 | 0.92 | .47 | .15 | 5.92 | *** | .22 | |
| 7 | 1.55 | .89 | .19 | 8.14 | *** | .79 | |
| 8 | 1.40 | .75 | .18 | 7.85 | *** | .56 | |
| PSYC S. | 9 | 1.00 | .81 | .65 | |||
| 10 | 0.91 | .66 | .09 | 10.53 | *** | .44 | |
| 11 | 1.08 | .77 | .09 | 12.56 | *** | .60 | |
| 12 | 1.07 | .79 | .08 | 12.78 | *** | .62 | |
| BEHAV S. | 13 | 1.00 | .56 | .31 | |||
| 14 | 1.09 | .59 | .16 | 6.99 | *** | .35 | |
| 19 | 2.11 | .81 | .26 | 8.27 | *** | .66 | |
| 24 | 2.03 | .76 | .25 | 8.08 | *** | .57 | |
| KNOW | 15 | 1.00 | .92 | .85 | |||
| 16 | 0.93 | .91 | .04 | 23.27 | *** | .82 | |
| 17 | 0.81 | .82 | .04 | 18.53 | *** | .67 | |
| 18 | 0.92 | .87 | .04 | 20.83 | *** | .75 | |
| DEPEN | 20 | 1.00 | .57 | .33 | |||
| 21 | 1.35 | .89 | .15 | 9.19 | *** | .79 | |
| 22 | 1.21 | .82 | .13 | 9.10 | *** | .68 | |
| 23 | 0.79 | .49 | .12 | 6.48 | *** | .24 |
Note. R.D.=Reaction to diagnosis (Feeling); SA=Physical health; PSYC S.=Psychological symptomatology (Caregiver); BEHAV S.=Behavioral symptomatology (Patient); KNOW=Knowledge of disease; DEPEN=Level of dependence; λ=Standardized regression coefficient; EE=Standardized Errors; C.R.=Critical ratio; P=Probability; R2=Squared Multiple Correlation of each item; ***=p< .001.
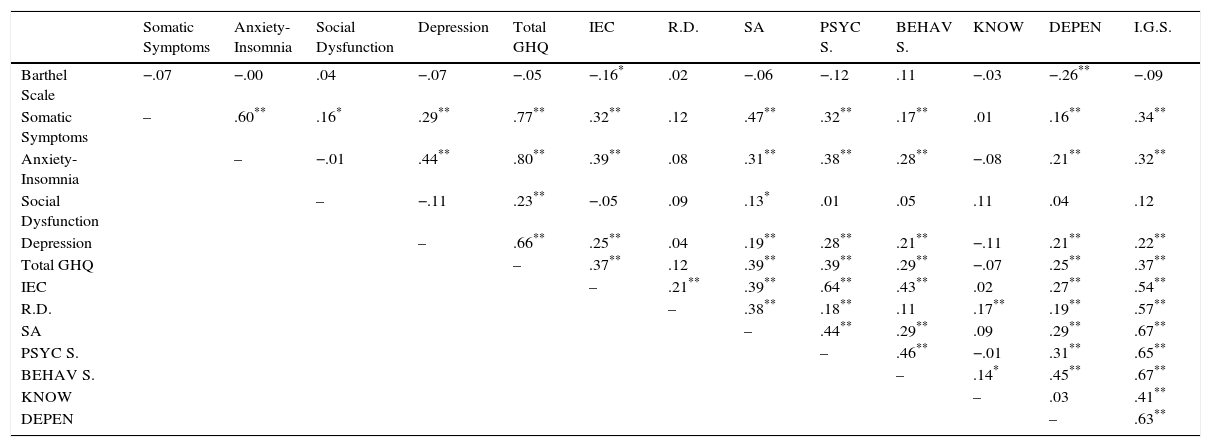
Convergent validity testing of the questionnaire with the Barthel Scale shows that only the IPSO-CA24 dependence factor shows any correlation, and that is negative, that is, as independence of the person cared for diminishes importance of the level of dependence factor increases for the caregiver. It should also be emphasized that practically all the health factors (GHQ-28) are correlated with the General Overburden Index as well as with several factors of the IPSO-CA24, showing how social dysfunction is only related positively to physical health of the caregiver. Finally, both total score or General Overburden Index and factors comprising the IPSO-CA24 show positive correlation with the General Caregiver's Effort Index, except Knowledge of the disease, that is, the greater the effort made by the caregiver, the more importance given to different facets of caregiving (Table 3).
Correlations. Convergent validity analysis of IPSO-CA24.
| Somatic Symptoms | Anxiety-Insomnia | Social Dysfunction | Depression | Total GHQ | IEC | R.D. | SA | PSYC S. | BEHAV S. | KNOW | DEPEN | I.G.S. | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Barthel Scale | −.07 | −.00 | .04 | −.07 | −.05 | −.16* | .02 | −.06 | −.12 | .11 | −.03 | −.26** | −.09 |
| Somatic Symptoms | – | .60** | .16* | .29** | .77** | .32** | .12 | .47** | .32** | .17** | .01 | .16** | .34** |
| Anxiety-Insomnia | – | −.01 | .44** | .80** | .39** | .08 | .31** | .38** | .28** | −.08 | .21** | .32** | |
| Social Dysfunction | – | −.11 | .23** | −.05 | .09 | .13* | .01 | .05 | .11 | .04 | .12 | ||
| Depression | – | .66** | .25** | .04 | .19** | .28** | .21** | −.11 | .21** | .22** | |||
| Total GHQ | – | .37** | .12 | .39** | .39** | .29** | −.07 | .25** | .37** | ||||
| IEC | – | .21** | .39** | .64** | .43** | .02 | .27** | .54** | |||||
| R.D. | – | .38** | .18** | .11 | .17** | .19** | .57** | ||||||
| SA | – | .44** | .29** | .09 | .29** | .67** | |||||||
| PSYC S. | – | .46** | −.01 | .31** | .65** | ||||||||
| BEHAV S. | – | .14* | .45** | .67** | |||||||||
| KNOW | – | .03 | .41** | ||||||||||
| DEPEN | – | .63** |
Note.
Factor analysis of the IPSO-CA24 identified six robust dimensions of overburden in Alzheimer's patient family caregivers with no specialized training: Reaction to diagnosis, Physical health, Psychological symptomatology (caregiver), Behavioral symptomatology (patient), Knowledge of the disease and Level of dependence. Although, adjusting the Model 1, six-factor model without the general overburden index, is acceptable, we analyzed the properties of both, leaving the selection of one of them for future studies. The questionnaire, the scales, etc., may be found at the link: www.grupocuidadores.com/ipso.
The consequences to physical health derived from caring for a family member make this dimension highly of overburden (Berglund et al., 2015; Delgado et al., 2014; Roth et al., 2015), and is more likely as the degree of patient dependence increases (Peña-Longobardo & Oliva-Moreno, 2015). Furthermore, with the inclusion of two symptomatology factors (psychological in the caregiver and behavioral in the patient), the IPSO-CA24 can subjectively evaluate the caregiver in other more objective facets of burden (Pearlin et al., 1990). Apart from this, the knowledge caregivers have about the disease is related to their expectations (Feldberg et al., 2011), the attitude with which they cope with situations derived from caregiving (Saavedra et al., 2013), and therefore, how they manage the disease (Lima-Rodríguez et al., 2015). Another of the components that directly influences the quality of caregiving is their reaction to the diagnosis (Caron & Caron, 2011). Specifically, the protective effect which having an early diagnosis might have in the long term becomes more obvious in family caregivers (Vugt & Verhey, 2013) both in decision-making and in adapting to the caregiver roll (Boots et al., 2015; Bronner et al., 2016).
Some of these dimensions, although already found in other measures of caregiver burden (Crespo & Rivas, 2015; Martos et al., 2015), have not been included in methodological proposals where they combine in an evaluation instrument such as this one. Furthermore, the diversity of approaches that evaluate the burden (Martín-Carrasco et al., 2013) must be added to the difficulty entailed in the heterogeneity of the caregiver profile itself (Rosa et al., 2010). All of this makes comparison of measurement instruments in this field (Brown & Brown, 2014) a difficult task.
To conclude, IPSO-CA24 component interactions with other measures show adequate levels of construct validity and the need to continue working in the line of the model proposed by Pérez-Fuentes et al. (2014), thereby insisting on a multidimensional approach to burden (Poulshock & Deimling, 1984; Rogero-García & Ahmed-Mohamed, 2014), and the current trend to consider patient and caregiver characteristics together (Lou et al., 2015). This instrument therefore responds to the need for multidimensional evaluation of the burden of family caregivers without specialized training.