Background/Objective: Depression and suicide ideation regularly occur together. Yet, little is known about factors that buffer individuals against the development of suicide ideation. The present study investigated, whether positive mental health buffers the association between depression and suicide ideation in a longitudinal study design. Methods: A total of 207 German students (70.3% female; age: M=26.04, SD=5.33) were assessed at a baseline evaluation and again twelve months later. Data were collected using self-report questionnaires. Linear hierarchical regression analysis was used to analyze the data. Positive mental health was considered to moderate the impact of depression on suicide ideation – controlling for age and gender. Results: Positive mental health was shown to moderate the impact of depression on suicide ideation: in those students who reported higher levels of positive mental health, depression severity showed no association with suicide ideation over time. Conclusion: Positive mental health seems to confer resilience and should be taken into account, when assessing individuals for suicide risk.
Antecedentes/Objetivo: La depresión y la ideación suicida ocurren regularmente juntos. Sin embargo, poco se sabe sobre los factores que protegen a las personas contra el desarrollo de la ideación suicida. El presente estudio investigó si la salud mental positiva amortigua la asociación entre la depresión y la ideación suicida en un diseño de estudio longitudinal. Método: Un total de 207 estudiantes alemanes (70,3% mujeres; edad: M=26.04, SD=5.33) fueron evaluados en una evaluación de línea base y nuevamente doce meses después. Los datos fueron recolectados usando cuestionarios de autoinforme. Se utilizó un análisis de regresión jerárquica lineal para analizar los datos. Se consideró que la salud mental positiva moderaría el impacto de la depresión en la ideación suicida, controlando la edad y el sexo. Resultados: Se demostró que la salud mental positiva modera el impacto de la depresión en la ideación suicida: en aquellos estudiantes que reportaron niveles más altos de salud mental positiva, la severidad de la depresión no mostró asociación con la ideación suicida con el paso del tiempo. Conclusión: La salud mental positiva parece conferir resistencia y debe tenerse en cuenta al evaluar a los individuos por riesgo de suicidio.
Suicide is the second leading worldwide cause of death for individuals aged 15 to 29 years (World Health Organization, WHO, 2014). Furthermore, suicide ideation and suicidal behaviors are especially common in young adults (Nock, Borges, & Ono, 2014). Among various risk factors, suicide ideation is seen as one of the strongest predictors of subsequent suicidal behavior (Franklin et al., 2017): Severe or pervasive ideation has been shown to predict death by suicide (Brown, Beck, Steer, & Grisham, 2000) and even passive ideation, such as a wish to die, has been identified as a risk factor for death by suicide (Brown, Steer, Henriques, & Beck, 2005). Since there is a rapid transition from suicide ideation to plans and attempts, Borges et al. (2014) claim that intervention efforts need “to focus on prevention of ideation rather than prevention of the transition from ideation to more serious outcomes” (p. 73). Yet, little is known about factors that buffer individuals against the development of suicide ideation.
In their work on the buffering hypothesis, Johnson, Wood, Gooding, Taylor and Tarrier (2011) suggest that to be viewed as conferring resilience, a psychological construct needs to demonstrate the following characteristics: (1) It needs to comprise a separate dimension to risk and moderate the association between risk and outcome. Therefore, to ascertain resilience an assessment of both, risk and suicide ideation or suicidal behavior is necessary; (2) It needs to be viewed as existing on a bipolar continuum, with its inverse amplifying the association between risk and outcome; (3) It needs to be a psychological construct, such as a set of positive beliefs. In the context of a comprehensive literature review, Johnson et al. (2011) identified various abilities and beliefs with buffering qualities concerning suicide ideation, such as positivity of attributional style, social support and self-agency.
In a recent test of the buffering hypothesis, Siegmann et al. (2017) examined the degree to which different resilience factors – namely positive mental health, self-efficacy, satisfaction with life, social support and psychosocial stress resistance – buffer the effects of depression on suicide ideation. Only positive mental health was shown to moderate the association between depression and suicide ideation both in a sample of German (N=601) and Chinese (N=2867) students: For those individuals who reported high levels of positive mental health, their levels of suicide ideation did not increase significantly even when they experienced a heightened level of depressive symptoms. Positive mental health may therefore be considered as conferring resilience in the sense of Johnson et al. (2011). Yet, due to the cross-sectional nature of the study, conclusions on causality cannot be drawn. Nonetheless, this finding complements a previous study, in which positive mental health was shown to predict the remission of suicide ideation in a large sample of young women (N=1.396), whereas severity of psychopathology, life satisfaction and self-efficacy did not predict the course of suicide ideation (Teismann, Forkmann, Glaesmer, Egeri, & Margraf, 2016). In both studies, positive mental health was assessed with the Positive-Mental Health Scale (Lukat, Margraf, Lutz, van der Veld, & Becker, 2016), an instrument developed to measure emotional, psychological and social aspects of well-being.
Regarding positive mental health, it is important to acknowledge that mental health and mental illness are not opposite ends of a single continuum, rather they constitute distinct but correlated axes (e.g., Keyes, 2005; Westerhoff & Keyes, 2010). Thus, the absence of psychopathology does not equal the presence of mental health and the presence of psychopathology does not equal the absence of mental health. As such, it has regularly been found that about ten percent of a given sample suffer from high levels of psychopathology and still report high levels of subjective well-being (e.g., Lyons, Huebener, Hills, & Shinkareva, 2012; Suldo & Shaffer, 2008). Even, suicide ideation and positive mental health regularly co-occur in clinical samples (Teismann et al., 2017).
On this background, the aim of the current study was to investigate, whether positive mental health does not only buffer the impact of depression on suicide ideation in a cross-sectional study design (cf. Siegmann et al., 2017), but also in a longitudinal study design. As depressive symptoms are one of the main risk factors for suicide ideation (Franklin et al., 2017), it is of special relevance to focus on factors that have the potential to mitigate the influence of this special risk factor on the development of suicide ideation. As such, it was hypothesized, that positive mental health would buffer the impact of depression on suicide ideation over a 12-month period.
MethodProcedureData for the present study was drawn from the ongoing BOOM (Bochum Optimism and Mental Health) project, a large-scale, cross-cultural, longitudinal investigation of risk and protective factors in mental health (Maercker et al., 2015; Schönfeld, Brailovskaia, Bieda, Zhang, & Margraf, 2016; Schönfeld, Brailovskaia, & Margraf, 2017). The Ethics Committee of the Faculty of Psychology of the Ruhr-Universität Bochum approved the study. All national regulations and laws regarding research on human subjects were followed, and required permission was obtained. Participants were provided information about the purpose of the study and an assurance of their anonymity in participation, and gave written informed consent in order to participate. Furthermore, all participants were provided with information where to receive help in case of psychological distress.
In Germany, each year (since 2011) an invitation e-mail including a link to the BOOM-baseline survey is sent to all students enrolled at the Ruhr-Universität Bochum, a large state university. After completing the baseline survey including questionnaires on different aspects of positive mental health (e.g., life satisfaction, self-efficacy, social support) as well as mental health problems (e.g., depression, anxiety, and stress), participants are asked whether they allow the BOOM-research-team to contact them for further assessment waves.
Data for the present study was collected between October/December 2015 (T1) and again between October/December 2016 (T2). A collective invitation e-mail including a link to an anonymous online survey using the Unipark-server (www.unipark.de) was sent to a randomly selected sample of 300 students of the Ruhr-Universität Bochum who had already taken part in an earlier recruitment wave within the BOOM-Project. In October/December 2016, a further collective invitation e-mail including a link to the second online self-report survey was sent to those students who had participated in the survey in 2015. Both surveys included the same questionnaires.
ParticipantsIn total 207 German students (n=147, 70.3% female; age: M=26.04, SD=5.33) at the Ruhr-Universität Bochum took part at the first measurement time point (T1) in 2015 and at the follow-up assessment (T2) in 2016. At T1, most students were either in their third (18.8%) or eleventh (15.9%) semester (range: 1-16 semesters). Students were registered in 18 different faculties. Most German students either lived together with a partner (n=124, 61.4%) or were singles (n=80, 38.6%).
MeasuresSuicidal Ideation and Behavior. Twelve-month suicide ideation (“How often have you thought about killing yourself in the past year?”) was assessed using the respective item of the Suicidal Behaviors Questionnaire – Revised (SBQ-R; Osman et al., 2001). The suicide ideation item is presented with a 5-point [1=never; 5=very often (5 or more times)] Likert scale. Lifetime suicide attempts were assessed using the respective item-response from the SBQ-R: “Have you ever attempted suicide, and really hoped to die?” If participants affirmed this question, they were also asked how often they attempted suicide in their lifetime. Though the original SBQ-R consists of four items, only the aforementioned items were used in the current study due to space constraints. The SBQ-R has been recommended for screening purposes (Batterham et al., 2015) and has repeatedly been used in clinical and non-clinical samples (Osman et al., 2001).
Depression. Depression was measured by a subscale of the Depression-Anxiety-Stress Scales 21 (DASS-21; Henry & Crawford, 2005). The seven depression items are presented with a 4-point (0=did not apply to me at all; 3=applied to me very much or most of the time) Likert scale. Psychometric properties of the DASS are well established in both clinical and non-clinical studies (Henry & Crawford, 2005). A score ≥ 10 points to a mild depressive symptomatology (Lovibond & Lovibond, 1995). Internal consistency in the current sample was α=.89.
Positive mental health. The nine-item Positive Mental Health Scale (PMH-scale; Lukat et al., 2016) assesses mainly emotional aspects of well-being. It was developed to assess a single holistic concept of positive emotionality related to positive mental health. The PMH-scale's items derived from the Trierer Personality Inventory (Becker, 1989), the Freiburg Personality Inventory (Fahrenberg, Selg, & Hampel, 1989), the Mental Health Scale (Tönnies, Plöhn, & Krippendorf, 1996), the Berner Well-Being Inventory (Grob et al., 1991), and one item formulated by Lukat et al. (2016). Participants respond to statements such as “In general, I am confident”, “All in all, I am satisfied with my life”, “I feel that I am actually well equipped to deal with life and its difficulties” on a scale ranging from 0 (I disagree) to 3 (I agree). Unidimensional structure and good convergent and discriminant validity are demonstrated in samples comprised of students, patients and the general population (Lukat et al., 2016). Cronbach's alpha was α=.92 in the current study.
Data AnalysesAll statistical analyses were conducted using the statistical analysis program R 3.3.2. Initially correlation analyses were carried out to explore associations between key variables. Changes in study variables from baseline (T1) to follow-up (T2) were analyzed using t-tests for dependent samples. To evaluate the relationship between depression, positive mental health and suicide ideation, a 4-step hierarchical linear regression analysis was conducted with T2 suicide ideation (SBQ-R) as dependent variable. Age and gender – both factors being differently associated with suicide ideation (Nock et al., 2014) – were entered as control variables in Step 1; depression severity (DASS) at T1 was entered in Step 2; positive mental health (PMH) at T1 was entered in Step 3, and the interaction of T1 depression severity and positive mental health was entered in Step 4. All metric predictors were z-standardized before entering into the regression analyses. If the interaction term adds significant predictive variance to the regression model, it indicates a moderating effect of positive mental health on the association between depression and suicide ideation (Hayes, 2013).
ResultsDescriptive statistics and correlationsDescriptive statistics for each measure are presented in Table 1. At baseline, 43 participants (21.5%) indicated some degree of suicidal ideation (i.e. SBQ-R Suicide Ideation Item > 0) within the past 12 months. Lifetime suicide attempts were reported by seven participants (3.4%). At the follow-up assessment 12 month later, 49 participants (23.6%) indicated some degree of suicidal ideation within the past 12 months. No participant attempted suicide between the two assessments. T-tests for dependent samples revealed that suicide ideation declined from the baseline to the follow-up assessment, t(206)=5.47, p=.000, whereas depression increased, t(206)=−3.38, p=.001, and positive mental health did not change, t(206)=0.64, p=.522.
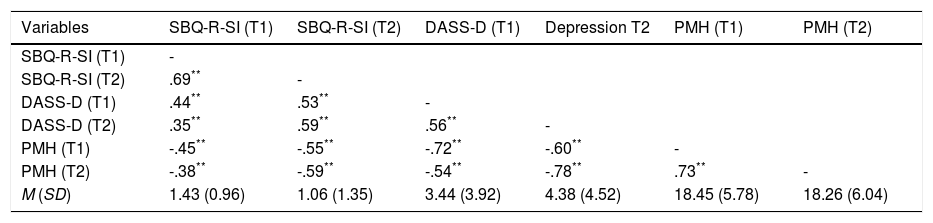
Means, standard deviations and correlations of study variables.
| Variables | SBQ-R-SI (T1) | SBQ-R-SI (T2) | DASS-D (T1) | Depression T2 | PMH (T1) | PMH (T2) |
|---|---|---|---|---|---|---|
| SBQ-R-SI (T1) | - | |||||
| SBQ-R-SI (T2) | .69** | - | ||||
| DASS-D (T1) | .44** | .53** | - | |||
| DASS-D (T2) | .35** | .59** | .56** | - | ||
| PMH (T1) | -.45** | -.55** | -.72** | -.60** | - | |
| PMH (T2) | -.38** | -.59** | -.54** | -.78** | .73** | - |
| M (SD) | 1.43 (0.96) | 1.06 (1.35) | 3.44 (3.92) | 4.38 (4.52) | 18.45 (5.78) | 18.26 (6.04) |
Note: DASS-D=Depression Anxiety Stress Scales – Depression Subscale; PMH=Positive Mental Health; SBQ-SI=Suicide Behaviors Questionnaire-Revised – Suicide Ideation.
Correlations indicated that depressive symptoms correlate positively with suicide ideation, and both depressive symptoms as well as suicide ideation correlate negatively with positive mental health at both assessments (see Table 1).
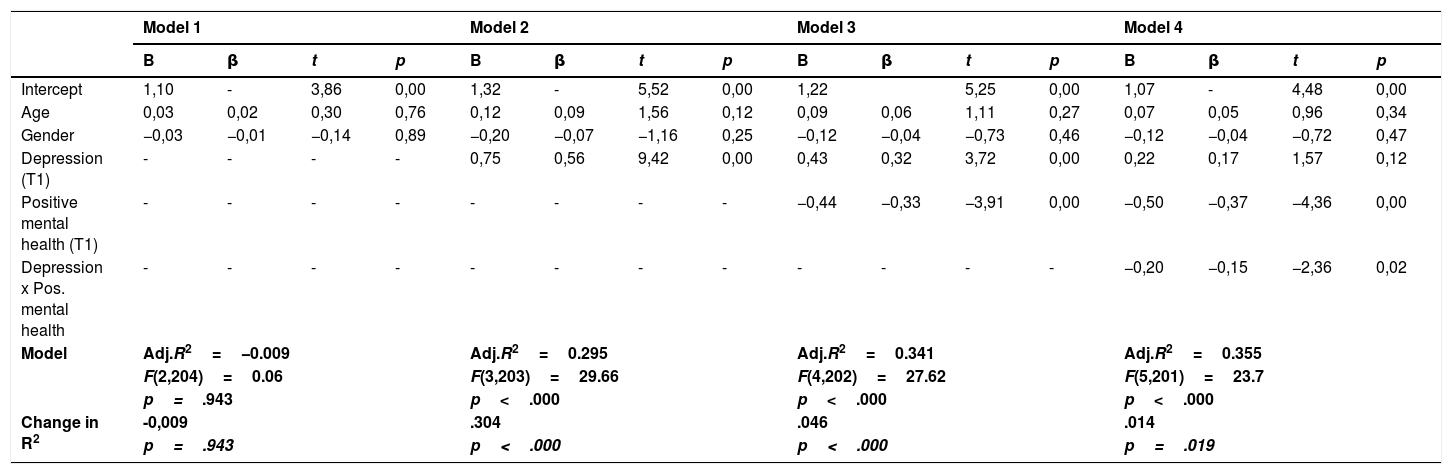
Moderation analysisTable 2 shows the results of the hierarchical linear regression analysis with suicide ideation at T2 as criterion variable.
Results of the hierarchical linear regression analysis predicting suicidal ideation (T2).
| Model 1 | Model 2 | Model 3 | Model 4 | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | β | t | p | B | β | t | p | B | β | t | p | B | β | t | p | |
| Intercept | 1,10 | - | 3,86 | 0,00 | 1,32 | - | 5,52 | 0,00 | 1,22 | 5,25 | 0,00 | 1,07 | - | 4,48 | 0,00 | |
| Age | 0,03 | 0,02 | 0,30 | 0,76 | 0,12 | 0,09 | 1,56 | 0,12 | 0,09 | 0,06 | 1,11 | 0,27 | 0,07 | 0,05 | 0,96 | 0,34 |
| Gender | −0,03 | −0,01 | −0,14 | 0,89 | −0,20 | −0,07 | −1,16 | 0,25 | −0,12 | −0,04 | −0,73 | 0,46 | −0,12 | −0,04 | −0,72 | 0,47 |
| Depression (T1) | - | - | - | - | 0,75 | 0,56 | 9,42 | 0,00 | 0,43 | 0,32 | 3,72 | 0,00 | 0,22 | 0,17 | 1,57 | 0,12 |
| Positive mental health (T1) | - | - | - | - | - | - | - | - | −0,44 | −0,33 | −3,91 | 0,00 | −0,50 | −0,37 | −4,36 | 0,00 |
| Depression x Pos. mental health | - | - | - | - | - | - | - | - | - | - | - | - | −0,20 | −0,15 | −2,36 | 0,02 |
| Model | Adj.R2=−0.009 | Adj.R2=0.295 | Adj.R2=0.341 | Adj.R2=0.355 | ||||||||||||
| F(2,204)=0.06 | F(3,203)=29.66 | F(4,202)=27.62 | F(5,201)=23.7 | |||||||||||||
| p=.943 | p<.000 | p<.000 | p<.000 | |||||||||||||
| Change in R2 | -0,009 | .304 | .046 | .014 | ||||||||||||
| p=.943 | p<.000 | p<.000 | p=.019 | |||||||||||||
In Model 1, neither age nor gender was associated with suicide ideation. In Model 2, depression emerged as a significant predictor of suicide ideation and in Model 3 positive mental health was a significant predictor of suicide ideation. In Model 4, the two-way-interaction of depression and positive mental health was a significant predictor. Although significant, the additional variance explained in Model 4 was rather low.
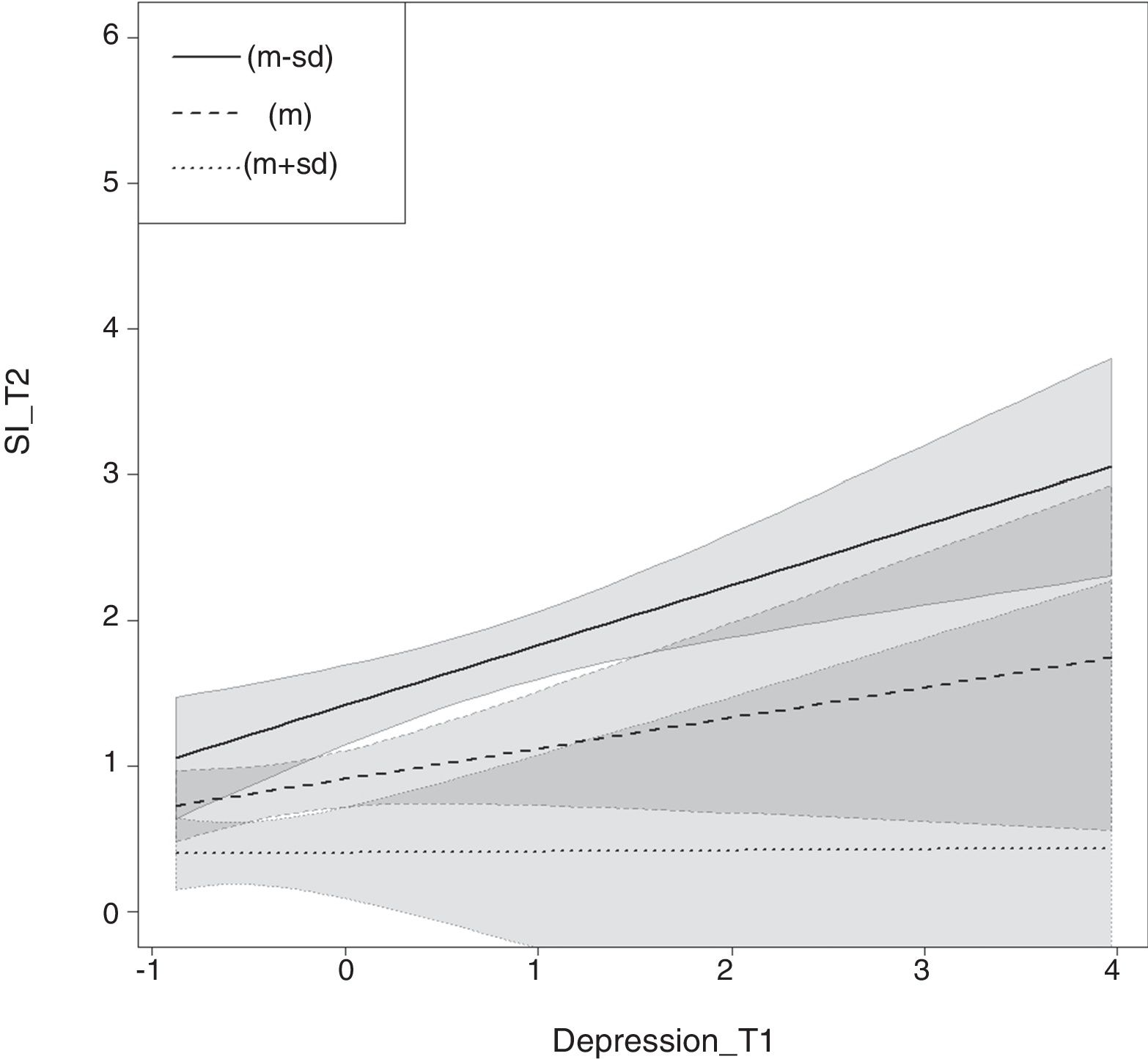
Nonetheless, positive mental health was found to moderate the effect of depression severity on suicide ideation. As can be seen in Figure 1, for those who reported higher levels of positive mental health (M+1SD), depression severity showed no association with suicide ideation over time.
Results of linear regression analysis with depression at T1 (depression_T1) predicting suicide ideation at T2 (SI_T2) for mean values (M) values M+1SD and M-1SD of the moderator PMH at T1. Light lines represent 95% confidence intervals of each regression line and shaded areas the range between regression line and corresponding 95% confidence interval.
In this longitudinal study, positive mental health was shown to buffer the impact of depression on suicide ideation in German students: For those individuals who reported high levels of positive mental health, their levels of suicide ideation did not increase significantly even when they experienced a heightened level of depressive symptoms. A general style of positive emotionality might therefore act as a resilience factor in the sense of Johnson et al. (2011). The current finding complement previous studies showing that well-being, as assessed with the PMH-scale, seems to be of special relevance to positive psychological functioning. As such previous studies found positive mental health to moderate the association between depression and suicide ideation in a cross-sectional analysis of German and Chinese students (Siegmann et al., 2017). Furthermore, the PMH-scale was among the most important predictors of remission from suicide ideation (Teismann et al., 2016) as well as from specific and social phobia (Trumpf, Becker, Vriends, Meyer, & Margraf, 2009; Vriends et al., 2007).
In terms of clinical implications, the results of the current study suggest that it may be important to account for the presence of facets of positive mental health in addition to risk factors, when assessing individuals for suicide risk. Though it seems obvious to do so, we doubt that this is regularly being done in clinical practice – especially since questions regarding a general sense of well-being are seldom incorporated in risk assessment tools. Furthermore, since positive mental health can significantly alter the impact of depression, it may be beneficial to think of fostering well-being in clinical interventions for depression and suicide prevention (c.f., Fava, 2016). On a theoretical level, the current results underscore the necessity that theoretical models of suicide ideation/behavior should strive to integrate both pathogenetic and protective factors (c.f., Cheavens, Cukrowicz, Hansen, & Mitchell, 2016).
There are several limitations to the present study. First, suicide ideation was only assessed with the respective item of the SBQ-R instead of a more comprehensive method to assess suicide ideation. Yet, it is rather common to assess suicide ideation with limited items in epidemiological studies (c.f., Borges, Angst, Nock, Ruscio, & Kessler, 2008; Gunnell, Harbord, Singleton, Jenkins, & Lewis, 2004) and there is strong evidence for the predictive ability and relevance of single items assessing suicide ideation (Green et al., 2015; Simon et al., 2013). Second, generalization of the results towards other age or societal groups than university students is not possible, since the study focused only on this highly educated population. Third, as a non-clinical sample was studied, levels of depression were rather low. As such, it is unclear to what extent the results would generalize to clinical samples. This latter aspect is true for most of the aforementioned studies on positive mental health. Therefore, studying the buffering qualities of positive mental health in clinical samples is highly warranted.
In reference to student samples, the current study underscores the importance of positive mental health as a buffer against suicide ideation in the face of depression.
FundingData collection and data analysis was supported by the Alexander von Humboldt-Professorship of Jürgen Margraf. The funding source was not involved in the interpretation of the data, in the writing of the report and in the decision to submit the article for publication.