Background/Objective: Sleep insufficiency, which affects more than 45% of the world's population, has a great importance when considering older adults. Thus, this research tested a mediation hypothesis, through a path analysis, which explains how depression relates to the quality of life considering the effects of sleep quality in older adults. Method: A sample of 187 community-dwelling Portuguese older adults answered questionnaires about sociodemographic status (age, gender, highest level of education completed, family status, sports activities, health, and retirement status), quality of life, sleep quality, and depression. Descriptive and path analysis statistics were performed considering the results of the normality test. Results: The sample has health characteristics and presents adequate sleep duration. Sleep quality acted as a mediator between depression and the quality of life in older adults, considering the variation of gender and health. This suggests that it is important to establish self-care practices, namely sleep quality, to intervene in the ageing process. Conclusions: It is important to consider sleep quality associated with depression for older adults and to test interventions to minimize health impacts. Also, more researches are needed about the primary prevention in sleep quality relating to depression.
Antecedentes/Objetivo: La insuficiencia del sueño, que afecta a más del 45% de la población mundial, tiene una gran importancia al considerar los adultos mayores. Por lo tanto, esta investigación probó una hipótesis de mediación, que explica cómo la depresión se relaciona con la calidad de vida, considerando los efectos de la calidad del sueño en adultos mayores. Método: Una muestra de 187 ancianos portugueses residentes en la comunidad respondió a cuestionarios sobre el estado sociodemográfico (edad, sexo, nivel educativo más alto, estado familiar, actividades deportivas, estado de salud y jubilación), calidad de vida, calidad del sueño y depresión. Se realizaron estadísticas descriptivos y de análisis de trayectoria, considerando los resultados de la prueba de normalidad. Resultados: La muestra presenta características de salud y una duración adecuada del sueño. La calidad del sueño actuó como mediador entre la depresión y la calidad de vida en adultos mayores, considerando la variación de género y salud. Conclusiones: Es importante considerar la calidad del sueño asociada con la depresión para adultos mayores y realizar intervenciones para minimizar los impactos en la salud. Además, se necesitan más investigaciones sobre la prevención primaria de la calidad del sueño relacionada con la depresión.
Good sleep quality is effective in preventing premature ageing, as demonstrated in a pioneering study that found that sleep deprivation had a detrimental effect on metabolism, endocrine function (Spiegel, Leproult, & Van Cauter, 1999), cognitive functions (Ballesio & Lombardo, 2016), health status (Rayward, Duncan, Brown, Plotnikoff, & Burton, 2017), life satisfaction (Zhi et al., 2016), and others. This means that sleep insufficiency can worsen chronic health problems related to age (Quevedo-Blasco, Zych, & Buela-Casal, 2014; Spiegel et al., 1999). That is, sleep strongly influences many aspects of health (physical, cognitive, and emotion health) and its restriction may predispose a person to adverse health conditions (Hirshkowitz et al., 2015). Thus, sleep insufficiency is a variable of great importance when considering older adults, because it may impact several domains, such as attention impairments, slowed response time, memory and concentration impairments, decreased ability to accomplish daily tasks, and increased risk of falling (Abraham, Pu, Schleiden, & Albert, 2017).
Having in account that the World Health Organization, WHO (2015) expects an increase from the current 841 million to 2 billion of the world's population to be over 60 years old by 2050, elderly well-being is a challenge to global public health. Unfortunately, the fact that elderly individuals live longer is not necessarily related to their quality of life; many these individuals depend on medication and medical and welfare care (WHO, 2015). This shows the importance of increasing research efforts to explore how the health of older adults is affected by issues such as the sleep quality. Therefore, there must be a better understanding of the multitude of factors impacting sleep satisfaction to improve sleep quality in older adults (Abraham et al., 2017) and promote health and quality of life.
The negative impact of sleep insufficiency and poor sleep quality has been observed and demonstrated in the physical, emotional, mental, and social domains of life, both on a short- and long-term basis (Gottlieb et al., 2005; Quevedo-Blasco et al., 2014; World Association of Sleep Medicine, 2016). There is also empirical evidence that shows a negative impact of the above-mentioned aspects on psychological disorders, such as depression, anxiety, and psychosis (Ballesio & Lombardo, 2016; Quevedo-Blasco et al., 2014). Therefore, emotion and sleep have been shown to be closely related, this issue is increasingly recognized as an important area of research (World Association of Sleep Medicine, 2016).
In addition, the relationship between sleep and emotions has been demonstrated as bi-directional and is reported by Kahn, Sheppes, and Sadeh (2013, p. 225) as a “vicious cycle”. Sleep tends to compromise emotional regulation, which in many cases leads to an increase in negative emotions and interrupts sleep, leading to new deficiencies in emotional well-being and life satisfaction (Kahn et al., 2013; Rayward et al., 2017). For this reason, further research is needed to understand the relationship between sleep and emotions, and the impact that this relationship may have on the quality of life. As such, this study tested a mediation hypothesis, through a path analysis, which could explain how depression relates to the quality of life considering the effects of sleep quality in older adults. This work aims to contribute to the knowledge about the relationship between sleep quality and depression, in order to assist in the development of interventions for the prevention of depression for older adults.
MethodParticipantsThis study used a cross-sectional descriptive design and intended to assess a non-clinical sample to meet with the WHO guidelines in the report entitled: World report on ageing and health (WHO, 2015, p. 18) that underlines the need for a development of new systems for health care and long-term care that are more in tune with the needs of older people. Above all, it will need to transcend outdated ways of thinking about ageing, foster a major shift in how we understand ageing and health, and inspire the development of transformative approaches.
Then, the inclusion criteria for the participants were: (a) older than 60 years, age prior to retirement and which provides scope for understanding the early stage of aging with “healthier” and more active individuals; (b) ability to understand, read, and write in Portuguese; (c) not living in a nursing home; and (d) not requiring permanent medical care in a specific location.
A convenience sample of 204 community-dwelling Portuguese older adults was collected. Subsequently, 12 individuals were excluded because they answered “no” to the question: “Do you consider yourself a healthy person?”. When considering that this research used self-report questionnaires the individual perception about health is relevant to obtain the desired sample (i. e., non-clinical sample with healthier characteristics as possible). Finally, five individuals were also removed from the sample to ensure univariate and multivariate normality.
A total of 187 questionnaires were used in the statistical analysis. For each individual data regarding age (M=69.43; SD=7.11), gender (73.3% were females), literacy (55.4% had basic scholarship), household (67.4% cohabitate), sports activities (70.7% practice sports), and retirement (87.6% were retired) were recorded. The application process occurred in Senior Universities from Portugal, where the participants were informed about the research objectives. All the participants in this study freely consented to answer the questionnaire. Anonymity and confidentiality standards were assured for all participants.
InstrumentsSociodemographic variables included age (in years), gender (male/female), highest level of education completed (primary or secondary education, graduate, postgraduate, master's, or PhD), household (live alone or in cohabitation), sports activities (play or not play sports), health (consider themselves as healthy), and retirement status.
Sleep quality was evaluated by the Portuguese version of the Pittsburgh Sleep Quality Index (PSQI-PT; João, Becker, Jesus, & Martins, 2017). This index is comprised by 19 items grouped into seven dimensions graded from 0 (No difficulty) to 3 (Difficulties). The PSQI dimensions include: (a) subjective sleep quality; (b) sleep latency; (c) sleep duration; (d) habitual sleep efficiency; (e) sleep disturbances; (f) use of sleeping medication; and (g) daytime dysfunction. The sum of these dimensions yields one global score, which ranges from 0 (no difficulty) to 21 (severe difficulties), highest scores indicate a worse sleep quality. A global PSQI score greater than 5 indicates major difficulties in at least two dimensions or moderate difficulties in more than three components. The internal consistency of the present study, estimated by Cronbach's alpha, was .69. Similar to values were found in other studies with non-clinical samples (Becker & Jesus, 2017; Spira et al., 2012).
Depression was assessed by the Portuguese version of the Depression Anxiety Stress Scale (DASS-21). This scale is comprised by 21 items, divided into three scales (depression, anxiety, and stress) with seven items each, and graded from 0 (It did not apply anything to me) to 3 (Applied to me most of the time). Participants evaluate the degree to which they experienced each symptom during the previous week. The results of the depression scale are determined by the sum of results of the seven items, where the minimum is 0 and the maximum 21. The highest scores on the depression scale correspond to negative emotional states (Pais-Ribeiro, Honrado, & Leal, 2004). The internal consistency for the present study, estimated by Cronbach's alpha, was .89.
Quality of life was evaluated by two scales. The first, WHOQOL-Bref (abbreviated version of the WHOQOL-100), was created by the World Health Organisation Quality of Life (Vaz Serra et al., 2006) and is a questionnaire comprised by 26 items grouped into four domains: (a) physical health (pain and discomfort, energy and fatigue, sleep and rest, mobility, daily living activities, dependence on medication and treatment, and work capacity); (b) psychological (positive feelings, thinking about learning, memory, concentration, self-esteem, body image and appearance, negative feelings, spirituality, religion, and personal beliefs); (c) social relationships (personal relationships, social support, and sexual activity); and (d) environment (physical security and protection, home environment, financial resources, health and social care (availability and quality), opportunities to acquire new information and skills, participation in and recreation/leisure opportunities, physical environment (pollution, noise, climate, transit), and transportation). The second, WHOQOL-Old, was also developed by the World Health Organization Quality of Life (Vilar et al., 2014) and must be applied together with the WHOQOL-Bref. This questionnaire is comprised by 24 items grouped into six domains: (a) Sensory abilities; (b) Autonomy; (c) Past activities, present, and future; (d) Social participation; (e) Death and dying; and (f) Intimacy. The scores from these six domains - or the values of the 24 items from the WHOQOL-Old - are combined to produce a general overall quality-of-life score for older adults, denoted here as the ageing domain. Therefore, the quality of life measure was evaluated for five domains (i.e., four domains related to WHOQOL-Bref and one domain related to WHOQOL-Old) that ranged from 0 to 100. The internal consistency of the present study, estimated by Cronbach's alpha, was .88 (WHOQOL-Bref) and .84 (WHOQOL-Old).
This research was performed in accordance with the European research guidelines and received approval from the Consulting Board of the Research Centre for Spatial and Organizational Dynamics (CIEO - Universidade de Algarve, Portugal). All the participants freely consented to answer the questionnaires and signed an informed consent statement before their inclusion in the study. Anonymity and confidentiality were assured for the participants.
Statistical analysisData entry errors or missing data were not observed; thus it was possible to consider all the questionnaires applied. Data analyses were performed with SPSS software version 21 and AMOS version 20. DASS-21, WHOQOL-Bref, WHOQOL-Old, and PSQI were computed. Descriptive statistics were computed for each sociodemographic, depression (Depression scale - DASS-21), quality of life (physical health, psychological, social relationships, social relationships, environment, and aging domains - WHOQOL-Bref and WHOQOL-Old), and sleep quality (PSQI-PT) variables, and their reliability was examined with the Cronbach's alpha coefficient (α). Descriptive statistics were calculated as frequencies for categorical variables, whereas means and standard deviations were computed for continuous variables.
The existence of outliers was evaluated by the square distance of Malahanobis (D2) and normality was assessed by the uni- and multivariate coefficients of skewness (sk) and kurtosis (ku). Five observations showed D2 values that would suggest their removal; therefore, the analysis was performed without these observations (N=187). Then, all the variables showed adequate normality as reported by Marôco (2014) for the maximum likelihood estimation (MLE) method, i.e., skewness >2-3 and kurtosis>7-10. To test the mediation hypothesis a path analysis technique was performed. The significance of the regression coefficients was evaluated after the estimation of the parameters by the maximum likelihood estimation method using AMOS 20.
The significance of direct, indirect, and total effects was assessed with bootstrap resampling as described by Marôco (2014). The effects with p ≤ .05 were considered significant. The adjustment of the model was evaluated using several statistical indexes including the chi-squared goodness-of-fit test (non-significant values indicate a good model fit), the root mean square error of approximation (RMSEA; values ≤ .05 indicate a very good fit), and the comparative fit (CFI), goodness of fit (GFI), and Tucker-Lewis (TLI) indexes (values ≥ .95 indicate a very good fit) (Marôco, 2014).
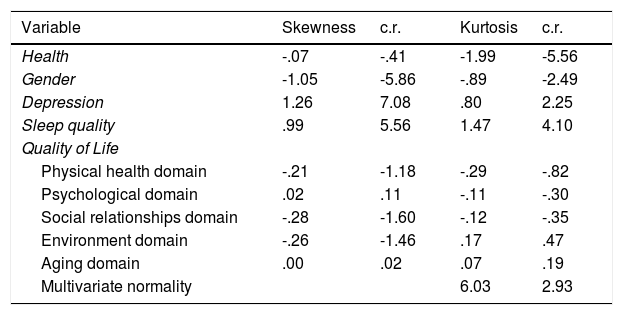
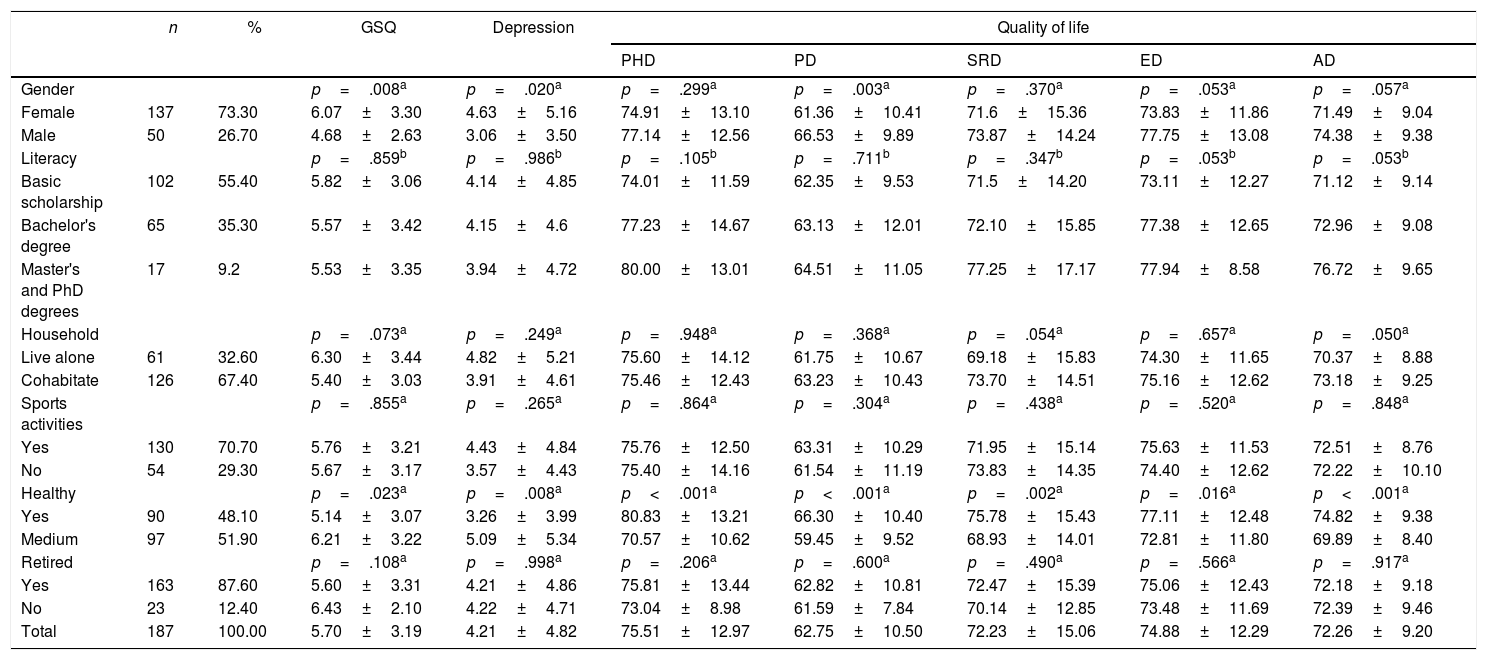
ResultsThe results of the normality assessment demonstrated that the variables used did not violate the assumptions of multivariate normality (Table 1). Baseline characteristics of the participants stratified by mean and standard deviation of each measure are presented in Table 2. There are significant differences between genders for the variables sleep quality, depression, and psychological domains (quality of life). There is a difference between individuals who consider themselves as healthy and those who consider themselves to be moderately healthy for all the considered variables (sleep quality, depression, and all domains of life quality).
Statistics for assessing the normality of the observed variables in the model.
| Variable | Skewness | c.r. | Kurtosis | c.r. |
|---|---|---|---|---|
| Health | -.07 | -.41 | -1.99 | -5.56 |
| Gender | -1.05 | -5.86 | -.89 | -2.49 |
| Depression | 1.26 | 7.08 | .80 | 2.25 |
| Sleep quality | .99 | 5.56 | 1.47 | 4.10 |
| Quality of Life | ||||
| Physical health domain | -.21 | -1.18 | -.29 | -.82 |
| Psychological domain | .02 | .11 | -.11 | -.30 |
| Social relationships domain | -.28 | -1.60 | -.12 | -.35 |
| Environment domain | -.26 | -1.46 | .17 | .47 |
| Aging domain | .00 | .02 | .07 | .19 |
| Multivariate normality | 6.03 | 2.93 | ||
Note. c.r.=critical ratio.
Sample characteristics and mean distribution (M±SD) to global sleep quality (GSQ), depression and quality of life domains.
| n | % | GSQ | Depression | Quality of life | |||||
|---|---|---|---|---|---|---|---|---|---|
| PHD | PD | SRD | ED | AD | |||||
| Gender | p=.008a | p=.020a | p=.299a | p=.003a | p=.370a | p=.053a | p=.057a | ||
| Female | 137 | 73.30 | 6.07±3.30 | 4.63±5.16 | 74.91±13.10 | 61.36±10.41 | 71.6±15.36 | 73.83±11.86 | 71.49±9.04 |
| Male | 50 | 26.70 | 4.68±2.63 | 3.06±3.50 | 77.14±12.56 | 66.53±9.89 | 73.87±14.24 | 77.75±13.08 | 74.38±9.38 |
| Literacy | p=.859b | p=.986b | p=.105b | p=.711b | p=.347b | p=.053b | p=.053b | ||
| Basic scholarship | 102 | 55.40 | 5.82±3.06 | 4.14±4.85 | 74.01±11.59 | 62.35±9.53 | 71.5±14.20 | 73.11±12.27 | 71.12±9.14 |
| Bachelor's degree | 65 | 35.30 | 5.57±3.42 | 4.15±4.6 | 77.23±14.67 | 63.13±12.01 | 72.10±15.85 | 77.38±12.65 | 72.96±9.08 |
| Master's and PhD degrees | 17 | 9.2 | 5.53±3.35 | 3.94±4.72 | 80.00±13.01 | 64.51±11.05 | 77.25±17.17 | 77.94±8.58 | 76.72±9.65 |
| Household | p=.073a | p=.249a | p=.948a | p=.368a | p=.054a | p=.657a | p=.050a | ||
| Live alone | 61 | 32.60 | 6.30±3.44 | 4.82±5.21 | 75.60±14.12 | 61.75±10.67 | 69.18±15.83 | 74.30±11.65 | 70.37±8.88 |
| Cohabitate | 126 | 67.40 | 5.40±3.03 | 3.91±4.61 | 75.46±12.43 | 63.23±10.43 | 73.70±14.51 | 75.16±12.62 | 73.18±9.25 |
| Sports activities | p=.855a | p=.265a | p=.864a | p=.304a | p=.438a | p=.520a | p=.848a | ||
| Yes | 130 | 70.70 | 5.76±3.21 | 4.43±4.84 | 75.76±12.50 | 63.31±10.29 | 71.95±15.14 | 75.63±11.53 | 72.51±8.76 |
| No | 54 | 29.30 | 5.67±3.17 | 3.57±4.43 | 75.40±14.16 | 61.54±11.19 | 73.83±14.35 | 74.40±12.62 | 72.22±10.10 |
| Healthy | p=.023a | p=.008a | p<.001a | p<.001a | p=.002a | p=.016a | p<.001a | ||
| Yes | 90 | 48.10 | 5.14±3.07 | 3.26±3.99 | 80.83±13.21 | 66.30±10.40 | 75.78±15.43 | 77.11±12.48 | 74.82±9.38 |
| Medium | 97 | 51.90 | 6.21±3.22 | 5.09±5.34 | 70.57±10.62 | 59.45±9.52 | 68.93±14.01 | 72.81±11.80 | 69.89±8.40 |
| Retired | p=.108a | p=.998a | p=.206a | p=.600a | p=.490a | p=.566a | p=.917a | ||
| Yes | 163 | 87.60 | 5.60±3.31 | 4.21±4.86 | 75.81±13.44 | 62.82±10.81 | 72.47±15.39 | 75.06±12.43 | 72.18±9.18 |
| No | 23 | 12.40 | 6.43±2.10 | 4.22±4.71 | 73.04±8.98 | 61.59±7.84 | 70.14±12.85 | 73.48±11.69 | 72.39±9.46 |
| Total | 187 | 100.00 | 5.70±3.19 | 4.21±4.82 | 75.51±12.97 | 62.75±10.50 | 72.23±15.06 | 74.88±12.29 | 72.26±9.20 |
Note. n=sample size; M=mean; SD=standard-deviation; PHD=Physical health domain; PD=Psychological domain; SRD=Social relationships domain; ED=Environment domain; a=p-value for independent samples t-test; b=p-value for ANOVA.
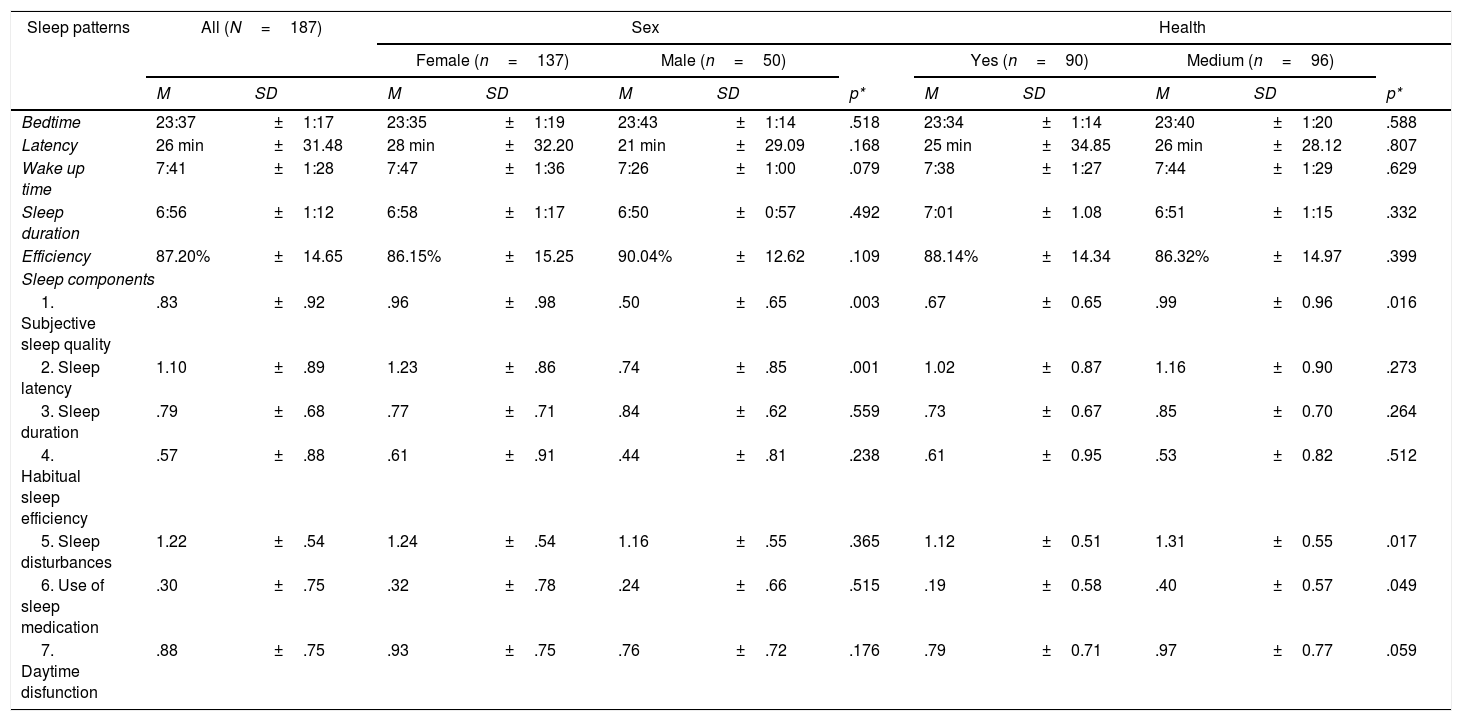
The mean distribution relative to the baseline characteristics of the participants demonstrated that gender and health are variables that must be considered, because they produce significant differences between groups. Table 3 contains the mean data of sleep patterns and sleep components of the whole sample and of the sample divided by gender and health. However, there were no significant differences in sleep patterns between groups. Regarding sleep components, there was a significant difference between subjective sleep quality for both characteristics (gender and health), sleep latency for gender, sleep disturbance for health, and use of sleep medication for health.
Sleep patterns and Sleep components according to PSQI responses.
| Sleep patterns | All (N=187) | Sex | Health | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Female (n=137) | Male (n=50) | Yes (n=90) | Medium (n=96) | |||||||||
| M | SD | M | SD | M | SD | p* | M | SD | M | SD | p* | |
| Bedtime | 23:37 | ±1:17 | 23:35 | ±1:19 | 23:43 | ±1:14 | .518 | 23:34 | ±1:14 | 23:40 | ±1:20 | .588 |
| Latency | 26 min | ±31.48 | 28 min | ±32.20 | 21 min | ±29.09 | .168 | 25 min | ±34.85 | 26 min | ±28.12 | .807 |
| Wake up time | 7:41 | ±1:28 | 7:47 | ±1:36 | 7:26 | ±1:00 | .079 | 7:38 | ±1:27 | 7:44 | ±1:29 | .629 |
| Sleep duration | 6:56 | ±1:12 | 6:58 | ±1:17 | 6:50 | ±0:57 | .492 | 7:01 | ±1.08 | 6:51 | ±1:15 | .332 |
| Efficiency | 87.20% | ±14.65 | 86.15% | ±15.25 | 90.04% | ±12.62 | .109 | 88.14% | ±14.34 | 86.32% | ±14.97 | .399 |
| Sleep components | ||||||||||||
| 1. Subjective sleep quality | .83 | ±.92 | .96 | ±.98 | .50 | ±.65 | .003 | .67 | ±0.65 | .99 | ±0.96 | .016 |
| 2. Sleep latency | 1.10 | ±.89 | 1.23 | ±.86 | .74 | ±.85 | .001 | 1.02 | ±0.87 | 1.16 | ±0.90 | .273 |
| 3. Sleep duration | .79 | ±.68 | .77 | ±.71 | .84 | ±.62 | .559 | .73 | ±0.67 | .85 | ±0.70 | .264 |
| 4. Habitual sleep efficiency | .57 | ±.88 | .61 | ±.91 | .44 | ±.81 | .238 | .61 | ±0.95 | .53 | ±0.82 | .512 |
| 5. Sleep disturbances | 1.22 | ±.54 | 1.24 | ±.54 | 1.16 | ±.55 | .365 | 1.12 | ±0.51 | 1.31 | ±0.55 | .017 |
| 6. Use of sleep medication | .30 | ±.75 | .32 | ±.78 | .24 | ±.66 | .515 | .19 | ±0.58 | .40 | ±0.57 | .049 |
| 7. Daytime disfunction | .88 | ±.75 | .93 | ±.75 | .76 | ±.72 | .176 | .79 | ±0.71 | .97 | ±0.77 | .059 |
Note. * t-test for independent samples.
The sample showed, for the majority of the participants (63.7%, n=119), the existence of an adequate sleep duration (seven to eight hours per day), according to the recommendations for this age group (Hirshkowitz et al., 2015). Other considerations included findings that older adults sleeping six to nine hours have better cognitive functioning, lower rates of mental and physical illnesses, and enhance quality of life compared with shorter or longer sleep durations (Hirshkowitz et al., 2015). So, those who sleep between six to nine hours of sleep are 89.9% (n=168) of the sample.
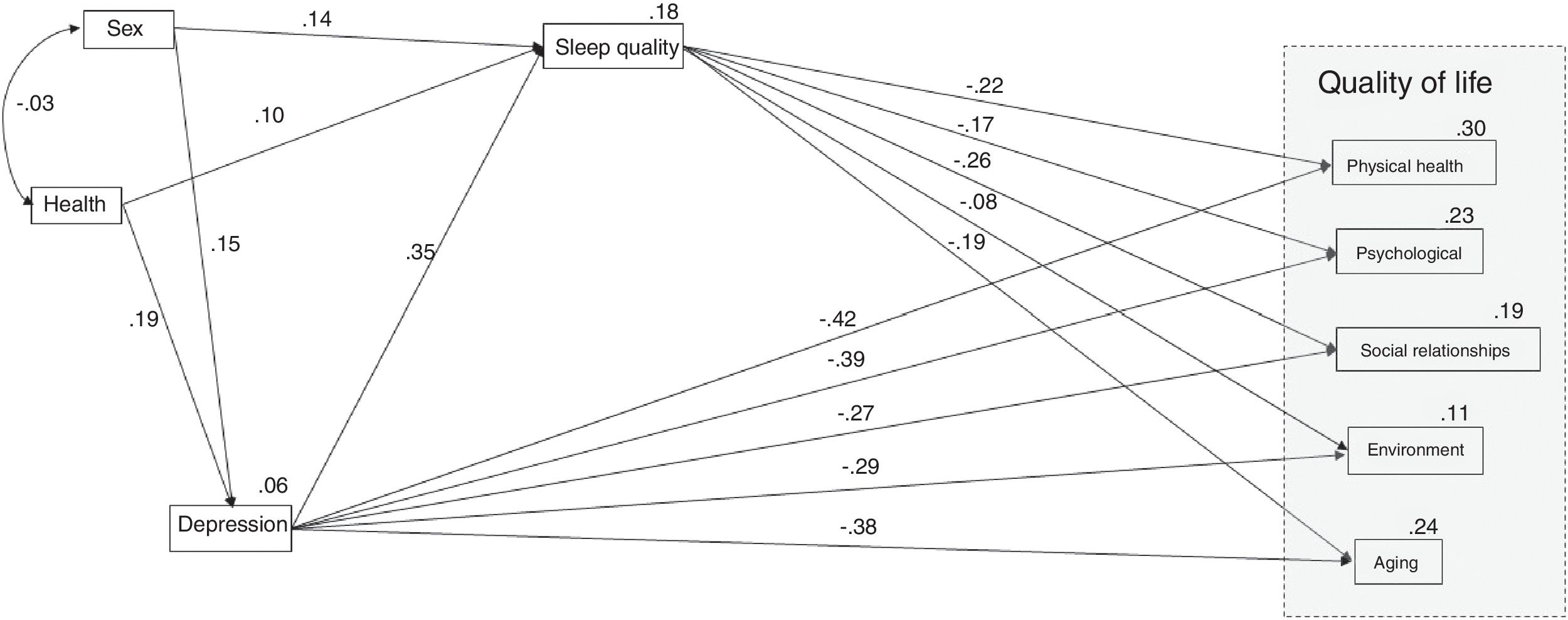
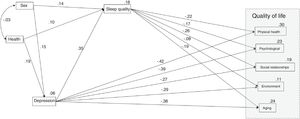
The proposed model (Figure 1) attempted to test the hypothesis that sleep quality mediates the relationship between depression and the quality of life of Portuguese older adults. Previous analyzes have demonstrated the importance of considering health and gender as exogenous variables. Figure 1 shows the model with the standardized regression coefficients and R2 values of the quality of life domains.
The model fit showed a moderate adjusted model (χ2(df)=41.55(10), p<.001; RMSEA=.10; CFI=.95; GFI=.96; TLI=.82). The adjusted model accounts for 30% of the physical health domain, 23% of the psychological domain, 19% of the social relationships domain, 11% of the environment domain, and 24% of the ageing domain of quality of life. All the trajectories were statistically significant (p<.05), with exception of the effect of sleep quality on the environmental domain (p=.261); i.e., the indirect effect of depression on the environmental domain was not statistically significant, as well as the effect of health on sleep quality (p=.126).
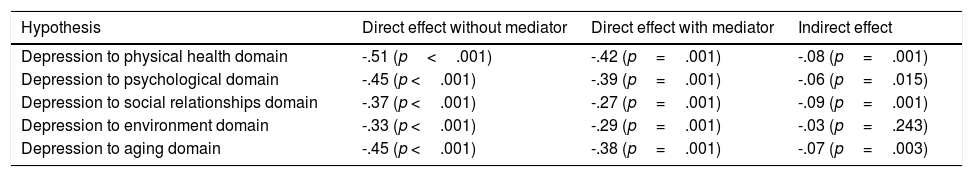
Regarding mediation assumptions (Marôco, 2014), their effects and respective significance were calculated for each tested mediation hypothesis (Table 4). It was observed that the sleep quality mediated the effect of depression with all domains of life quality, except for the environment domain.
Standardised effects* of mediation of sleep quality to quality of life.
| Hypothesis | Direct effect without mediator | Direct effect with mediator | Indirect effect |
|---|---|---|---|
| Depression to physical health domain | -.51 (p<.001) | -.42 (p=.001) | -.08 (p=.001) |
| Depression to psychological domain | -.45 (p <.001) | -.39 (p=.001) | -.06 (p=.015) |
| Depression to social relationships domain | -.37 (p <.001) | -.27 (p=.001) | -.09 (p=.001) |
| Depression to environment domain | -.33 (p <.001) | -.29 (p=.001) | -.03 (p=.243) |
| Depression to aging domain | -.45 (p <.001) | -.38 (p=.001) | -.07 (p=.003) |
Note. *Standardized effects=β.
The present study aimed to confirm whether sleep quality mediated the relationship between depression and the quality of life of Portuguese older adults. The age range of the sample used in the present study introduces some important criteria due to the fact that the participants had autonomy to perform their daily activities. This criterion differs from other studies where the lack of autonomy was considered (Moryś, Pąchalska, Bellwon, & Gruchała, 2016). This study intended to evaluate a non-clinical sample and the strategy followed was to collect the sample within senior universities. The goal was to have participants who had a more active life and were in better health. A clinical sample or institutionalized individuals would have many more variables that would influence the results. Therefore, the use of a non-clinical sample allowed us to develop a different look for the proposed goal of this study. The guidelines followed are based on proposal of the WHO (2015), meaning that it is necessary to transcend the outdated ways of thinking about ageing. Thus, this study attempted to address “health” - not just “diseases” - to develop fundamental health research on ageing. As such, these results follow the effort to understand the functioning of older adults within a health perspective.
Researches focusing on healthy elderly adults have found that the studies that used objective sleep measures (e.g., polysomnography) showed a poorer sleep quality than results from subjective measures (Maglione et al., 2012). However, this difference also occurred when sleep was associated with depressive symptoms (Maglione et al., 2012). This divergence using objective versus subjective measures can be explained by the multifactorial structure of the sleep dysfunction construct, which causes confusion in diagnosis with respect to determining which individuals need a deeper investigation of the etiology of their complaints (Mollayeva et al., 2016). This characterizes a challenge in primary and specialized medical care.
In this research depression was characterized as loss of self-esteem and motivation, and was associated with the perception of low probability of achieving life goals that are meaningful to an individual (Lovibond & Lovibond, 1995). Therefore, the depression subscale of DASS-21 measured the core symptoms of depression, i.e., cognitive symptoms. In older adults the physical symptoms and consequent reactive emotion to physical disease often mimic vegetative and affective symptoms of depressive disorders. Thus, cognitive symptoms of depression are highly valid and specifically useful for differentiating older individual's pathological depression (Moryś et al., 2016).
The number of recommended sleeping hours for older adults is six to eight hours per day, it does not differ much from adults (seven to nine hours) (Hirshkowitz et al., 2015). At this time of life the majority of older adults has no obligations related to employment, as such sleep requirements are lower. In addition, older adults tend to have more opportunities to sleep compared to younger ones. Increased age-associated morbidity influences sleep in this age group (Hirshkowitz et al., 2015).
Despite the changes in sleep structure, most of the older adults in this sample (89.9%) sleep between six to nine hours, findings show that older adults who sleep this number of hours have better cognitive functioning, lower rates of physical and mental illness, and better quality of life compared to shorter or longer sleep durations (Hirshkowitz et al., 2015). This proves that the results presented are able to reflect as closely as possible the health of this age group. Nevertheless, 4.8% of the sample has excessive sleep time (≥ nine or ten hours), which is strongly related to morbidity and mortality, signaling the need for medical, neurological, or psychiatric evaluation (Hirshkowitz et al., 2015).
Accumulated evidence suggests the close link between impaired sleep and aging-related cognitive decline (Hita-Yañez, Atienza, & Cantero, 2013), supporting the role of sleep loss in the pathogenesis of Alzheimer's disease (Kang et al., 2009; Roh et al., 2012). In the present study participants most likely ranged from normal cognition to mild cognitive impairment (not dementia) given the lack of neurological/neuropsychological examinations. If this is the case, those with poorer cognitive function may show impaired sleep, which in turn may be related to decreased life quality and increased risk of depression.
A previous meta-analysis verified that depression was associated with subjective sleep disturbances (r0=.42, p <.001; Becker, Jesus, João, Viseu, & Martins, 2016), as well as other works (Dzierzewski et al., 2015; Maglione et al., 2012; Potvin, Lorrain, Belleville, Grenier, & Préville, 2014; Rashid & Tahir, 2015). Thus, sleep quality was considered an important variable influencing depression and other variables, such as life quality.
The adjusted model used in this study demonstrated that poor sleep quality is capable of mediating the relationship between depression and life quality domains, except on the environmental domain. In consonance, other works showed that poor sleep quality has been observed as having a long- and short-term negative impact on physical, emotional, mental, and social life domains (Gottlieb et al., 2005; World Association of Sleep Medicine, 2016). Therefore, aspects of the environment domain were not previously addressed as a factor associated with sleep quality. However, in the proposed model there was no significant effect.
This research adds the role of sleep quality as an intervening variable between depression and quality of life. Therefore, health care should pay more attention to the sleep quality of older adults and provide educational programs for the management of sleeping difficulties (Park, Yoo, & Bae, 2013). Thus, it may enable the maintenance of a good sleep quality as a way to promote health and prevent possible diseases (Kaufmann, Susukida, & Depp, 2017; Knutson et al., 2017).
Several studies relate the impact of sleep quality on depression but it is necessary to develop a preventive approach, which will contribute to a better quality of life in older adults (Ohayon et al., 2017). Other researches have demonstrated the need to prevent depression in adults and this could be an important factor to improve the quality of life (Richards et al., 2016). Therefore, education and policy initiatives that promote appropriate sleep hygiene behaviors in older adults are necessary and it is very important to assess with more detail the efficiency of sleep quality interventions and the relationship between with depression outcomes.
This study presents a major limitation related to the sample size. The use of different analytical techniques to assess sleep quality is restricted. There are many aging-related conditions that indeed affect sleep and mood, for instance obesity/overweight, subclinical signs of sleep breathing/motor disorders, hypertension, diabetes, impaired cognition, preclinical Alzheimer's disease, and cerebral vascular damage. Therefore, it is necessary to obtain this information from the sample to understand how it is could influence the results obtained in the present study.
Thus, in future studies it is necessary to use a larger sample that includes moderation analyses using the sleep quality assessment model proposed by Becker and Jesus (2017). Also, the evaluation of sleepiness will be important to correlate with perceived sleep quality in obtaining more specific results, as well as other important characteristics of aging explained above.
It is important to establish self-care practices for people who are able to explore the way they are living during the ageing process and to assist in adapting to this transitional moment in life, by trying to minimize the impact of depression. At the same time, primary prevention in sleep quality should be developed and evaluated considering the possible prevalence of depression.
FundingThis study was supported by the Foundation for Science and Technology–Portugal (CIEO–Research Centre for Spatial and Organizational Dynamics, University of Algarve, Portugal). N. B. Becker received a doctoral fellowship from the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES). Process BEX 1990/15-2.