Background/Objective: Concomitant prescription of two or more psychiatric medications has become the rule and patients could adhere differently to their various drugs prescribed. Sidorkiewicz et al. published a questionnaire for assessing adherence to each specific drug. Method: This study explored the predictive validity of the Spanish version of the Sidorkiewicz questionnaire in a sample of 470 consecutive psychiatric outpatients using 897 psychiatric drugs. Results: The questionnaire showed adequate predictive validity in both univariate and multivariate analyses (logistic regression and CHAID segmentation) since they demonstrated a significant association with the 10-item Drug Attitude Inventory and with the Necessity and Concern Scales of the Beliefs about Medications Questionnaire. Some demographic and clinical variables were significant in the univariate analyses but lost significance in the multivariate analyses. Conclusions: The adherence of the psychiatric patient to his/her prescribed treatment may not be significantly influenced by socio-demographic or clinical characteristics, but rather by attitudes toward medication, perceptions of personal necessity for medication, and concerns about its potential adverse effects. This study's findings suggest that the Spanish version of the Sidorkiewicz questionnaire may be a useful and valid instrument for assessing adherence to each individual drug taken by psychiatric outpatients undergoing polypsychopharmacy.
Antecedentes/Objetivo: La prescripción concomitante más de un psicofármaco en un mismo paciente se ha convertido en la regla de la práctica clínica psiquiátrica actual, pudiendo adherirse los pacientes de manera diferente a sus diversos fármacos prescritos. Sidorkiewicz y colaboradores publicaron un cuestionario para evaluar la adherencia a cada fármaco tomado por el paciente. Método: Este estudio valora la validez predictiva de la versión española del cuestionario de Sidorkiewicz en una muestra de 470 pacientes ambulatorios psiquiátricos consecutivos que usaban 897 fármacos psiquiátricos. Resultados: El cuestionario mostró una adecuada validez predictiva, tanto en análisis univariados como multivariados (regresión logística y CHAID), registrándose asociaciones significativas con el DAI-10 y con las escalas de Necesidad y Preocupación del BMQ. Algunas variables sociodemográficas y clínicas fueron significativas en el análisis univariado perdiendo su significación en el multivariado. Conclusiones: La adherencia del paciente psiquiátrico al tratamiento no está condicionada por características sociodemográficas o clínicas, sino por actitudes hacia la medicación y por las percepciones de necesidad personal de la medicación y preocupaciones sobre sus posibles efectos adversos. La versión española del cuestionario de Sidorkiewicz es un instrumento válido para evaluar la adherencia a cada fármaco tomado por pacientes psiquiátricos ambulatorios polimedicados.
Polypharmacy, taking multiple drugs, is becoming common and almost the norm for most psychiatric patients (Ghaemi, 2002). The popularity of polypharmacy is somewhat surprising since it is based on experience rather than evidence (Stahl, 2002) and there is general agreement that polypharmacy can interfere with optimal medication adherence (Murray & Kroenke, 2001) which may lead to limited treatment effectiveness and result in higher rates of relapse, hospitalization, and disability (Sajatovic, Velligan, Weiden, Valenstein, & Ogedegbe, 2010). The prevalence of polypharmacy in psychiatry varies by country and even within different mental health resources in one country and can also be influenced by differing definitions. Having defined polypharmacy as the use of two or more psychoactive medications to treat the same psychiatric condition (Kingsbury, Yi, & Simpson, 2001), in our catchment area in the Canary Islands, Spain, we found a 42% prevalence in a large sample of>2,500 psychiatric outpatients representing the population of the Community Mental Health Centers (with a mean number of different psychotropic drugs=1.63±0.93, range 1–7) (De las Cuevas & Sanz, 2004). Strikingly, the prevalence increases to 93% in>1,300 patients discharged from psychiatric hospitals to the same Community Mental Health Centers (3.3±1.3, range, 1–9) (De las Cuevas & Sanz, 2005).
There is no established gold standard method for measuring medication adherence; each method has pros and cons (Garfield, Clifford, Eliasson, Barber, & Willson, 2011; Williams, Amico, Bova, & Womack, 2013). Although self-reports tend to overestimate adherence behavior (Osterberg & Blaschke, 2005), the use of validated self-report questionnaires is the simplest and least expensive method of measuring adherence (Garfield et al., 2011; National Collaborating Centre for Primary Care, NICE, 2009). Moreover, self-report questionnaires provide actionable information to medical providers about patient medication-taking behavior (Stirratt et al., 2015) in clinical psychiatric settings.
In situations of polypharmacy, available self-report questionnaires for assessing medication adherence are hampered because they provide a measure of global adherence in each patient, but do not provide information about each individual drug taken by each patient. In our experience, this is a major problem, because our psychiatric patients appear to adhere differently to the various psychiatric medications prescribed to them and exhibit diverse medication-taking behaviors for the various drugs. Our experience is supported by the limited available information on medication adherence studies in non-psychiatric patients (Osterberg, Urquhart, & Blaschke, 2010; Viana et al., 2014).
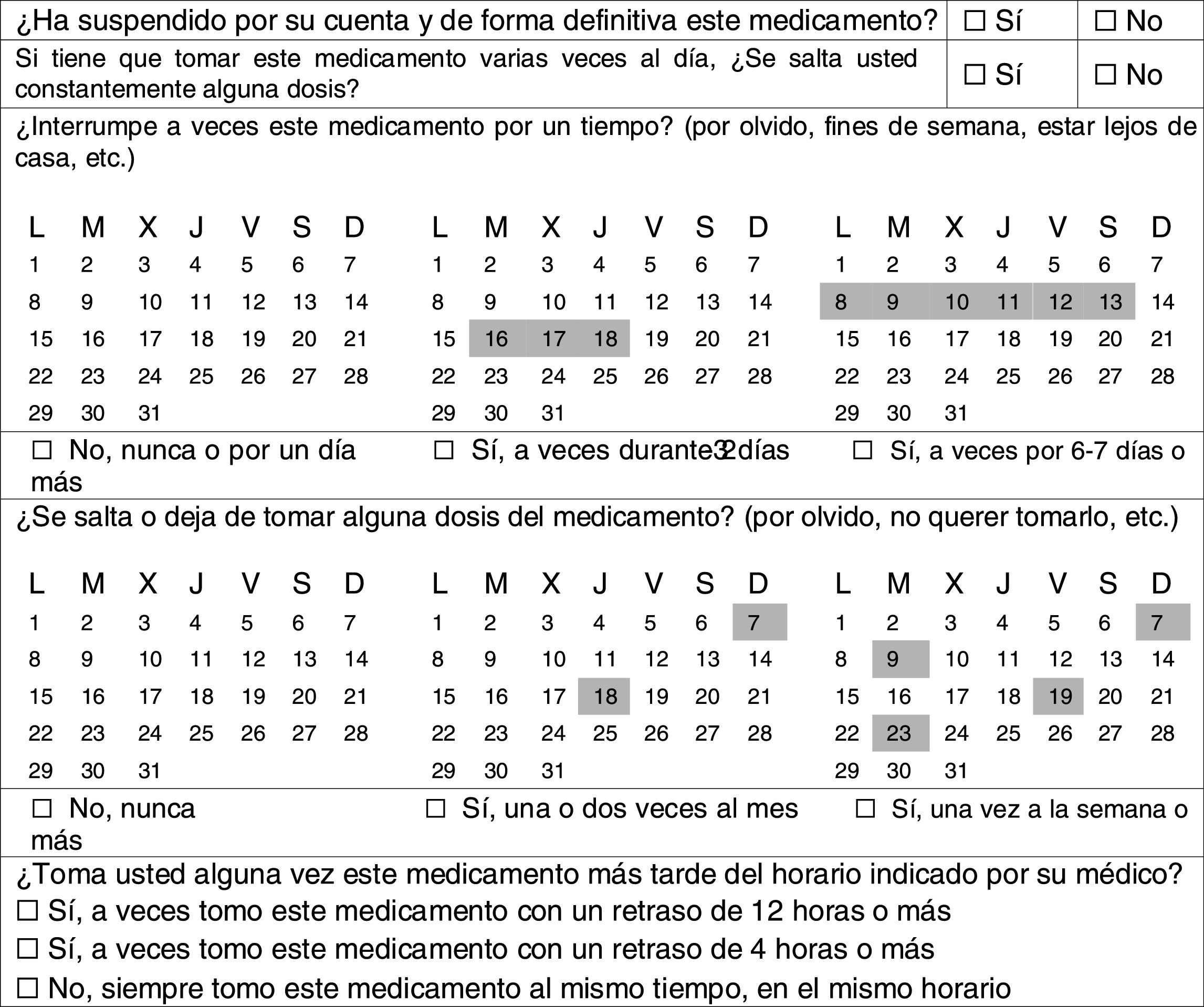
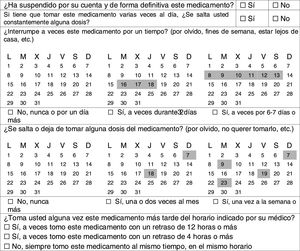
The idea of having a global measure of medication adherence for each patient basically implies that adherence is a characteristic of each patient influenced by the complexity of the prescription regimen, long-term medication use, and clinical conditions. On the other hand, Sidorkiewicz, Tran, Cousyn, Perrodeau and Ravaud (2016), proposed an original and new approach based on the idea that adherence also is a property of medicine classes. This self-reported adherence tool is an instrument for assessing adherence for each individual drug in patients with long-term therapies. The questionnaire contains five questions related to (1) early discontinuation of the drug, (2) systematic omission of a daily dose (e.g., at noon), (3) drug holidays, (4) skipping doses and (5) schedule errors. Each question has two or three possible answers, and the language uses non-threatening sentences to reduce social desirability bias, with practical examples and pictographs to help patients recognize their medicine-taking behaviors. The instrument defines six drug adherence levels for a given drug. Level 1 corresponds to high drug adherence (no drug holidays, no missing doses and no schedule errors); level 2 corresponds to good drug adherence (no drug holidays and no missing doses; schedule errors ≥4h); level 3 corresponds to moderate drug adherence (no drug holidays; missing doses once or twice a month and/or schedule errors ≥12h); level 4 corresponds to poor drug adherence (drug holidays for 2–3 days and/or missing doses ≥1/week); level 5 corresponds to very poor drug adherence (systematically skipping a daily dose and/or drug holidays ≥6 days); and level 6 corresponds to drug discontinuation. The authors (Sidorkiewicz et al., 2016) report adequate psychometric properties, including good convergent validity with the Morisky Medication Adherence Scale of 4 items (Morisky, Green, & Levine, 1986), with the Lu self-reported adherence instrument (Lu et al., 2008), and a significant agreement with the adherence evaluated by their physicians. It also showed good temporal stability (test-retest).
This new tool appears to us to be the most effective method for measuring treatment using self-reported adherence, which is our major priority for psychiatric clinical practice, and for advancing our research studies in medication adherence in psychiatry. This study aims to explore the predictive validity of the Spanish version of the recently published Sidorkiewicz adherence tool in a psychiatric outpatient setting. Thus, it is our first attempt to explore the different medication-taking behaviors for each drug taken by patients with polypharmacy in our outpatient catchment area.
MethodStudy design and participantsThis cross-sectional study was completed at the Community Mental Health Services of a university hospital in the Canary Islands, Spain. The inclusion criteria for the psychiatric outpatients were as follows: (1) 18 years or older, (2) able to read and understand Spanish, (3) diagnosed with a psychiatric disorder; (4) treated for at least 3 months with psychiatric drugs, and (5) participating voluntarily. Each participant received a full explanation of the study, after which, all participants signed an informed consent document. This study was approved by the Ethics Committee for Clinical Research of the University Hospital Nuestra Señora de la Candelaria, in the Canary Islands. Each participant then filled out a brief socio-demographic survey and the rest of the questionnaires. We offered no reward for participation.
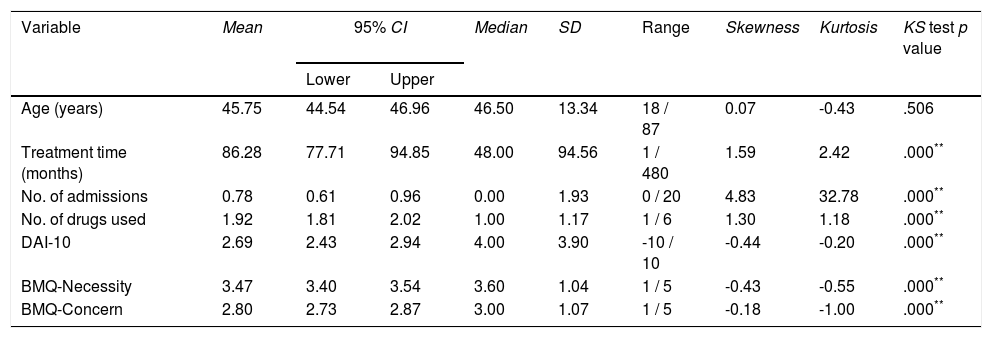
A final sample of 470 consecutive psychiatric outpatients was accepted for participation in this study (560 patients invited to participate, 84% response rate). Table 1 shows their socio-demographic and clinical variables.
Socio-demographic and clinical characteristics of psychiatric outpatients (n=470, using 897 psychoactive drugs).
| Variable | Mean | 95% CI | Median | SD | Range | Skewness | Kurtosis | KS test p value | |
|---|---|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||||
| Age (years) | 45.75 | 44.54 | 46.96 | 46.50 | 13.34 | 18 / 87 | 0.07 | -0.43 | .506 |
| Treatment time (months) | 86.28 | 77.71 | 94.85 | 48.00 | 94.56 | 1 / 480 | 1.59 | 2.42 | .000** |
| No. of admissions | 0.78 | 0.61 | 0.96 | 0.00 | 1.93 | 0 / 20 | 4.83 | 32.78 | .000** |
| No. of drugs used | 1.92 | 1.81 | 2.02 | 1.00 | 1.17 | 1 / 6 | 1.30 | 1.18 | .000** |
| DAI-10 | 2.69 | 2.43 | 2.94 | 4.00 | 3.90 | -10 / 10 | -0.44 | -0.20 | .000** |
| BMQ-Necessity | 3.47 | 3.40 | 3.54 | 3.60 | 1.04 | 1 / 5 | -0.43 | -0.55 | .000** |
| BMQ-Concern | 2.80 | 2.73 | 2.87 | 3.00 | 1.07 | 1 / 5 | -0.18 | -1.00 | .000** |
| Variable | Category | Frequency | Percent | 95% CI | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Sex | Male | 223 | 47.4% | 42.9% | 52.1% |
| Female | 247 | 52.6% | 47.9% | 57.1% | |
| Educational level | Can read and write | 12 | 2.6% | 1.3% | 4.4% |
| Primary school | 132 | 28.1% | 24.1% | 32.4% | |
| Secondary school | 195 | 41.5% | 37.0% | 46.1% | |
| College or higher | 131 | 27.9% | 23.9% | 32.2% | |
| Involuntary admissions | Yes | 91 | 19.4% | 15.9% | 23.2% |
| No | 379 | 80.6% | 76.8% | 84.1% | |
| Diagnoses | Depressive disorder | 179 | 38.1% | 33.7% | 42.6% |
| Anxiety disorder | 130 | 27.7% | 23.7% | 32.0% | |
| Schizophrenia | 110 | 23.4% | 19.6% | 27.5% | |
| Bipolar disorder | 33 | 7.0% | 4.9% | 9.7% | |
| Personality disorder | 14 | 3.0% | 1.6% | 4.9% | |
| Other diagnoses | 4 | 0.9% | --- | --- | |
| Psychoactive drug | Antidepressants | 194 | 41.3% | 36.8% | 45.9% |
| Anxiolytics | 126 | 26.8% | 22.9% | 31.1% | |
| Antipsychotics | 111 | 23.6% | 19.8% | 27.7% | |
| Mood stabilizers | 39 | 8.3% | 6.0% | 11.2% | |
| Polypharmacy | Monotherapy | 236 | 50.2% | 45.6% | 54.8% |
| Polypharmacy | 234 | 49.8% | 45.2% | 54.4% | |
Notes. DAI-10: Drug Attitude Inventory–10 items; BMQ: Belief about Medication Questionnaire; the variable is normally distribute;
Sidorkiewicz instrument translation. The guidelines for cross-cultural adaptation of self-report measures developed by Beaton, Bombardier, Guillemin, and Ferraz (2000), were used for this five-stage translation. In the first stage, the initial translation, two independent bilingual translators, both competent in English and Spanish and one of them aware of the concepts being examined in the questionnaire being translated, whose mother tongue is the target language (Spanish), translated the original questionnaire from English to Spanish. In the second step, synthesis of the translations, the translators reached a consensus on the translation of words, phrases and items based on the synthesis of translations, working from the original questionnaire, as well as the versions of the first and second translators. The third stage, the back translation, involving a new bilingual translator who was totally blind to the original version, translated the Spanish version of the questionnaire back into the original English language as a process of validity checking to make sure that the translated version reflected the same item content as the original version. The fourth stage, the expert committee phase, analyzed the cultural suitability and content validity testing; it was conducted by three independent psychiatrists and psychologists. These professionals rated the degree to which each item of the instrument covered the content that was supposed to be measured as an index of representativeness and content validity. They also evaluated the comprehension and equivalence of translation (semantic equivalence and content) between the English and Spanish versions. The final stage of the adaptation process, stage five, the test of the final version, was the field test of the new questionnaire. It sought to use the prefinal version with 30 patients from the target setting. These patients completed the questionnaire, and were interviewed to probe what they thought was meant by each questionnaire item and the chosen response. Both the meaning of the items and responses were explored, examining the distribution of responses. Appendix.
To explore the predictive validity (Nunnally & Bernstein, 1994) of the Sidorkiewicz instrument two scales were used: the 10-item Drug Attitude Inventory and the Beliefs about Medication Questionnaire Specific Scale. These two scales were chosen due to (1) our ample experience with them, (2) their consistency in predicting adherence to prescribed treatment in psychiatric care, (3) their ability to be used in any treatment context, and (4) their brevity, in order to minimize the burden for psychiatric patients who may be cognitively impaired.
Drug Attitude Inventory–10 items (DAI-10). The DAI-10 was created to measure attitudes toward psychiatric medications in adults (Hogan, Awad, & Eastwood, 1983). It is a self-report questionnaire consisting of true/false statements about the perceived effects and benefits of psychiatric drugs with which the patients can agree or disagree. The scoring equals the total sum of the items, ranging from−10 (very poor attitude) to+10 (best possible attitude). DAI-10 scores predicted adherence in different psychiatric disorders (De las Cuevas, de Leon, Peñate, & Betancort, 2017; De las Cuevas & Peñate, 2015a); it has been used as a validation standard for other scales (Chen, Tam, Wong, Law, & Chiu, 2005; Jeste et al., 2003). In our study we used the validated Spanish version of the scale (Cronbach's alpha: .67).
Beliefs about Medication Questionnaire. The BMQ-Specific (De las Cuevas et al., 2011; Horne & Weinman, 1999) assesses patient beliefs about the medication he/she is prescribed for a specific illness, examining perceptions of personal necessity for medication and concerns about potential adverse effects. The scale includes 10 items in two subscales: Concern and Necessity, each with five items. The degree of agreement with each statement is indicated on a five-point Likert scale, ranging from 1=strongly disagree to 5=strongly agree. The Necessity/Concern framework has proven to be a useful conceptual model for understanding patients’ perspectives on prescribed medicines and a fundamental factor in predicting their adherence to treatment (De las Cuevas, Peñate, & Cabrera, 2016a; Horne et al., 2013). In our study we used the validated Spanish version of the scale (Necessity subscale Cronbach's alpha: .70; Concern subscale Cronbach's alfa: .80).
Data analysisThe data were analyzed using SPSS version 22.2 for windows (IBM Corp. Released, 2013). Techniques and statistical tests used included: distribution of frequencies and percentages for qualitative variables; data exploration with normal-fit QQ graph, histogram, asymmetry coefficients and kurtosis/height together with the Kolmogorov-Smirnov goodness-of-fit test and description with the usual centrality (mean, median) and variability (standard deviation, range: Min/Max and interquartile range) for quantitative variables; and tests of difference of means (student's t and ANOVA) next to its non-parametric alternatives (Mann-Whitney and Kruskall-Wallis), Chi-square, ROC Curve, Binary Logistic Regression and CHAID Segmentation Tree for inferential analysis. For some analyses, original levels of adherence supplied by the tool were dichotomized into “adherent” (which included previous high (1), good (2), and moderate (3) levels) versus “non-adherent” (which included previous poor (4), very poor (5), and discontinuation (6) levels). The usual confidence level of 5% (significant if p <.050) was already set, except for the Kolmogorov-Smirnov normality test, which was considered to be a mismatch only if p <.010 (1%).
Statistical comments on differences between subjects and drugs. This study recruited a sample of 470 different patients. In each patient, we collected data regarding the adherence to one or more drugs prescribed (not always the same), providing a total of 897 drug records that we must consider as independent data since the answers given by a patient about a drug do not depend on the answers given by the same patient about another drug. These 897 records are considered to be a valid sample size for the analyses to be performed.
Studying predictive validity. According to Nunnally and Bernstein (1994), predictive validity is “using an instrument to estimate some criterion behavior that is external to the measuring instrument itself”. In this study, we use 3 external validators: attitudes toward psychiatric treatment, and beliefs about necessity and concern of prescribed psychiatric treatment to explore the predictive validity of the Spanish version of the Sidorkiewicz adherence instrument. An additional proof of predictive validity would be that demographic and clinical variables are not strong predictors of the scores on the Sidorkiewicz adherence instrument, unless their influence is mediated by the 3 external validators. To test this additional proof of predictive validity, we hypothesize that any significant socio-demographic or clinical variable in the univariate analyses will lose its significance in the multivariate analyses (logistic regression and CHAID segmentation).
ResultsSample descriptionFrom April to June 2017, 470 consecutive psychiatric outpatients were recruited. Table 1 describes their socio-demographic variables including a mean age of 45.7; approximately 52% were women, 42% completed secondary school, and 28% had a university degree. The most important main diagnoses were schizophrenia, 23%; bipolar disorder, 7%; depressive disorders, 38%; anxiety disorders, 27%; and personality disorders, 3%. Patients took a total of 897 medications; the most important classes were antidepressants in 35% of patients, antianxiety benzodiazepines in 35%, antipsychotics in 20%, and mood stabilizers in 11% (Table 1). The mean treatment duration was 86 months and the mean number of different psychoactive drugs prescribed per patient was 1.9. The rate of polypharmacy was 50%, which includes 25% of patients receiving two drugs, 14% receiving three, 7% receiving four, and 4% of the patients receiving five or more psychotropic drugs.
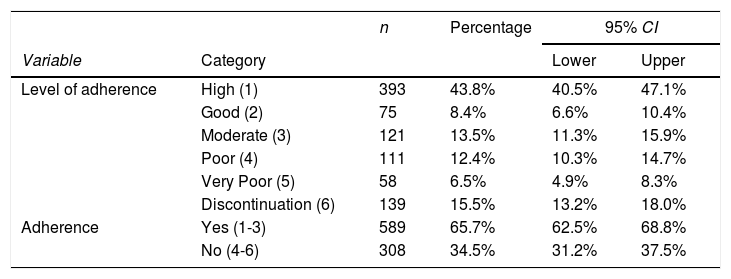
Results from the Sidorkiewicz adherence instrumentGlobal self-reported adherence, based on percentage, according to the Sidorkiewicz adherence tool at the drug level of the 897 drugs, disregarding who took them, was high in 44%, good in 8%, moderate in 13%, poor in 12%, very poor in 7% and discontinued the drug in 16% (Table 2). More than a third of polypharmacy patients reported discordance in adherence to their prescribed treatment (i.e., varying levels of adherence among the different psychoactive drugs used).
Descriptive analysis. Adherence to psychotropic drugs (N=897).
| n | Percentage | 95% CI | |||
|---|---|---|---|---|---|
| Variable | Category | Lower | Upper | ||
| Level of adherence | High (1) | 393 | 43.8% | 40.5% | 47.1% |
| Good (2) | 75 | 8.4% | 6.6% | 10.4% | |
| Moderate (3) | 121 | 13.5% | 11.3% | 15.9% | |
| Poor (4) | 111 | 12.4% | 10.3% | 14.7% | |
| Very Poor (5) | 58 | 6.5% | 4.9% | 8.3% | |
| Discontinuation (6) | 139 | 15.5% | 13.2% | 18.0% | |
| Adherence | Yes (1-3) | 589 | 65.7% | 62.5% | 68.8% |
| No (4-6) | 308 | 34.5% | 31.2% | 37.5% | |
To explore external evidences of validity, the adherence tool was used to compare results according to the patients’ socio-demographic variables, such as age, gender, and educational level, as well as according to clinical variables, such as psychiatric diagnosis, type of psychiatric drug used, treatment duration, and treatment complexity (polypharmacy).
Although women self-reported a higher adherence (67.4% vs. 63.8%), no differences were obtained in the level of adherence as a function of gender (X2=5.97, p=.309; r=.08) or dichotomized adherence (X2=1.29, p=.256; r=.03). However, a statistically significant correlation was found between the adherence tool and age (F (5, 891)=2.29, p=.000): self-reported adherence increased with patient age. The ROC analysis performed to find the cut-off point that maximizes this relationship between adherence and age confirmed the significant relationship (curve area: .56; 95% IC: .52- .60) and was suggestive of the age of 65 years, from which there is a greater probability of adherence. Concerning educational level, patients with lower educational level reported greater adherence (X2=9.40, p=.024; r=.19).
In relation to patient diagnosis, the adherence tool was able to differentiate between the five major groups of psychiatric disorders considered (i.e., schizophrenia, bipolar disorders, depressive disorders, anxiety disorders, and personality disorders) (level of adherence, X2=74.85, p=.001; r=.27); dichotomized adherence, X2=25.97, p=.001; r=.17). Patients with bipolar disorder self-reported the highest adherence (72.7%) while patients with personality disorder the lowest one (22.2%). No significant correlations were found as a function of treatment complexity (i.e., the presence of polypharmacy; level of adherence, X2=4.94, p=.423; r=.07); dichotomized adherence (X2=0.42, p=.519; r=.02), type of psychiatric drug used (level of adherence, X2=24.50, p=.057; r=.16); dichotomized adherence (X2=6.87, p=.076; r=.07) or treatment duration (F=0.05, p=.819).
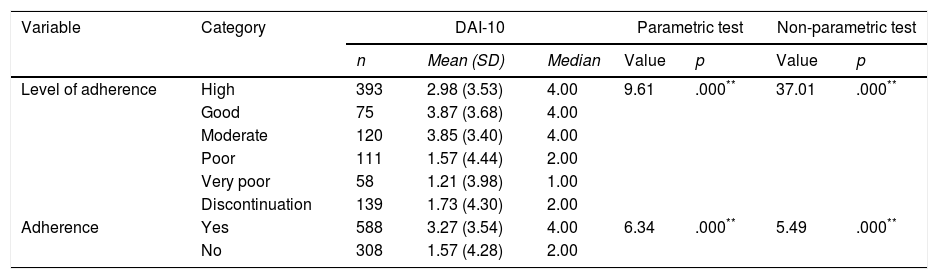
Predictive validity using three external validators in univariate analysesTable 3 shows the associations between adherence, attitudes toward psychiatric treatment and beliefs about necessity for and concern about prescribed psychiatric treatment. Concerning patients’ attitudes toward their psychiatric treatment, both in contrast to the level of adherence and in dichotomous adherence, a highly significant relationship (p <.001) (Table 3) was found such that, without doubt, the cases with higher adherence present higher scores on the Drug Attitudes Inventory (3.27 vs. 1.57; difference close to 2 points). Similar highly significant associations were evidenced between adherence and the perception of necessity for a specific psychiatric drug (BMQ-Necessity) and the concern about its adverse consequences (BMQ-Concern).
Inferential analysis. Univariate association between adherence, attitudes toward psychiatric treatment and beliefs about necessity and concern of prescribed psychiatric treatment.
| Variable | Category | DAI-10 | Parametric test | Non-parametric test | ||||
|---|---|---|---|---|---|---|---|---|
| n | Mean (SD) | Median | Value | p | Value | p | ||
| Level of adherence | High | 393 | 2.98 (3.53) | 4.00 | 9.61 | .000** | 37.01 | .000** |
| Good | 75 | 3.87 (3.68) | 4.00 | |||||
| Moderate | 120 | 3.85 (3.40) | 4.00 | |||||
| Poor | 111 | 1.57 (4.44) | 2.00 | |||||
| Very poor | 58 | 1.21 (3.98) | 1.00 | |||||
| Discontinuation | 139 | 1.73 (4.30) | 2.00 | |||||
| Adherence | Yes | 588 | 3.27 (3.54) | 4.00 | 6.34 | .000** | 5.49 | .000** |
| No | 308 | 1.57 (4.28) | 2.00 | |||||
| Variable | Category | BMQ-Necessity | Parametric test | Non-parametric test | ||||
|---|---|---|---|---|---|---|---|---|
| n | Mean (SD) | Median | Value | p | Value | p | ||
| Level of adherence | High | 393 | 3.63 (0.99) | 3.60 | 9.76 | .000** | 40.66 | .000** |
| Good | 75 | 3.78 (1.00) | 4.00 | |||||
| Moderate | 120 | 3.52 (0.94) | 3.60 | |||||
| Poor | 111 | 3.16 (1.03) | 3.40 | |||||
| Very poor | 58 | 3.30 (1.01) | 3.40 | |||||
| Discontinuation | 139 | 3.10 (1.15) | 3.20 | |||||
| Adherence | Yes | 589 | 3.63 (0.98) | 3.80 | 6.65 | .000** | 6.03 | .000** |
| No | 308 | 3.15 (1.08) | 3.40 | |||||
| Variable | Category | BMQ-Concern | Parametric test | Non-parametric test | ||||
|---|---|---|---|---|---|---|---|---|
| n | Mean (SD) | Median | Value | p | Value | p | ||
| Level of adherence | High | 393 | 2.68 (1.05) | 2.80 | 5.37 | .000** | 28.50 | .000** |
| Good | 75 | 2.61 (0.99) | 2.80 | |||||
| Moderate | 120 | 2.66 (1.05) | 2.60 | |||||
| Poor | 111 | 3.01 (0.98) | 3.20 | |||||
| Very poor | 58 | 3.03 (1.11) | 3.20 | |||||
| Discontinuation | 139 | 3.08 (1.17) | 3.40 | |||||
| Adherence | Yes | 589 | 2.66 (1.04) | 2.80 | 5.14 | .000** | 5.28 | .000** |
| No | 308 | 3.05 (1.09) | 3.40 | |||||
Note. Parametric tests included ANOVA and Student's t-test while non-parametric included Mann-Whitney and Kruskall-Wallis tests.
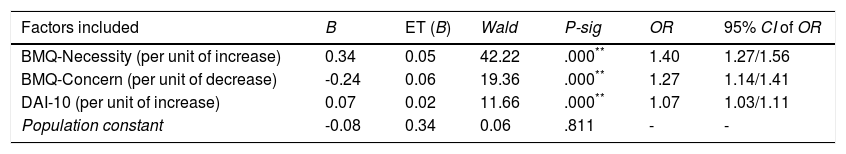
After these results and considering adherence in its dichotomous form as the main variable in the analysis, we proceeded to a multivariate study of these three variables using the binary logistic regression method. The results of this method are summarized in Table 4. The regression model presented is highly significant (p <.001 in the Omnibus Test), reaching a moderately high degree of adjustment (22.1%, according to Nagelkerke R2) and correctly classifying 93.5% of the cases with adherence and 69.3% of the total. Therefore, the model is very effective in predicting adherence, but not so much for the prediction of non-adherence to prescribed treatment. From this multivariate perspective, the necessity scale is revealed as the main factor (p <.001) for adherence prediction (OR=1.40 per unit increase in need) followed by the concern scale (p <.001; OR=1.27 per unit of reduction on this scale) and the attitudes scale (p <.001; OR=1.07 per unit of increase). Therefore, the three scales are associated in multivariate form with adherence, demonstrating their relationship with it. The inclusion of interactions between these three factors in the multivariate model did not add significance (p> .05).
Multiple logistic regression model. Predictive factors of adherence=Yes (N=896).
| Factors included | B | ET (B) | Wald | P-sig | OR | 95% CI of OR |
|---|---|---|---|---|---|---|
| BMQ-Necessity (per unit of increase) | 0.34 | 0.05 | 42.22 | .000** | 1.40 | 1.27/1.56 |
| BMQ-Concern (per unit of decrease) | -0.24 | 0.06 | 19.36 | .000** | 1.27 | 1.14/1.41 |
| DAI-10 (per unit of increase) | 0.07 | 0.02 | 11.66 | .000** | 1.07 | 1.03/1.11 |
| Population constant | -0.08 | 0.34 | 0.06 | .811 | - | - |
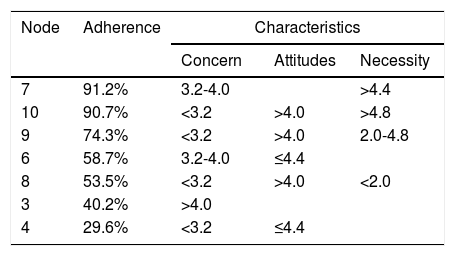
Finally, a Chi-square automatic interaction detection (CHAID) analysis was carried out to explain the patients’ responses to the categorical dependent variable (adherence: yes/no) in reference to the following variables: attitudes toward psychiatric treatment, perceived necessity of the medication and concerns about having to take it. The results of this tree classification method (see Supplementary Material) showed that the profile with the highest degree of adherence observed is the correspondence of patients with average values on the concern scale and high values on the necessity scale, regardless of their attitudes (91%). It follows the profile of cases with low values on the concern scale and neutral or positive values in attitudes toward medication, regardless of their perceived degree of necessity of them (74%). On the contrary, the profile with the lowest degree of adherence (30%) was found in those patients with low values on the concern scale and negative values (≤4) on the attitudes scale. As reader may have not be familiar with the interpretation of CHAID tree analyses, Table 5 provides a summary of the 7 terminal nodes order according to percentage of adherence.
Predictive validity demonstrated by three external validators eliminating the significance of socio-demographic and clinical variables in multivariate analysesSome of the socio-demographic and clinical variables, including age and some diagnoses, were significantly associated with the Sidorkiewicz adherence tool in the univariate analyses. None of these variables retained significance when the 3 external validators were introduced in the multivariate analyses, the logistic regression or the CHAID analysis. Thus, the socio-demographic and clinical variables of the patient seem not to have major relevance in adherence to treatment. Their effects in the univariate analyses appear to mainly reflect the patients’ attitudes towards their psychiatric medication, their perception of the need to have to use this medication and their concern for its possible side effects.
DiscussionTo our knowledge, this is the first study that assesses the psychometric properties of the Sidorkiewicz adherence tool for each individual drug taken by psychiatric patients. The original instrument was tested on a sample of consecutive patients in six general practice outpatient clinics and six academic general hospitals in France, and it was found to have acceptable validity and reliability for assessing adherence for each drug taken by patients, confirming its usability in hospital and primary care settings (Sidorkiewicz et al., 2016).
Medicine-taking is a complex human behavior and patients evaluate medicines, and the risks and benefits of medicines using the resources available to them (Nunes et al., 2009). The Necessity/Concern framework has demonstrated its utility in explaining non-adherence to prescribed medication (De las Cuevas et al., 2016a; Maidment, Livingston, & Katona, 2002) and shown that adherence in long-term conditions for psychiatric disorders is associated with stronger perceptions of necessity for drug treatment and fewer concerns about its adverse consequences (Horne et al., 2013).
Our results, both from the univariate and the multivariate perspectives (with logistic regression and CHAID segmentation analysis), support the significant relationships of this adherence tool with respect to factors such as attitudes toward psychiatric drug treatment, perceived necessity of use and concern about its adverse consequences. We consider that the adherence estimates evaluated by this tool at the drug level may be more accurate than those obtained with other instruments since the tool does not make value judgments about whether a patient is adherent or not, but rather evaluates specific behaviors for specific drugs with a “no-blame approach” approach, which would avoid social desirability by suggesting to the patient that non-adherence can be habitual and certainly his/her decision to respect. The high response rate obtained in our study supports this consideration and suggests good acceptability of the instrument.
The results obtained in this study are in line with the previous work of our research group, which emphasized the role played by the variables of the health belief model in adherence to the prescribed psychiatric treatment (De las Cuevas & de Leon, 2017; De las Cuevas et al., 2017; De las Cuevas et al., 2016a; De las Cuevas & Peñate, 2015a; De las Cuevas, Peñate, & Cabrera, 2016b; De Leon & de las Cuevas, 2017), although our prior research is limited because we used the Morisky Medication Adherence Scale of 8 items as an instrument for assessing adherence (De las Cuevas & Peñate, 2015b). Nevertheless, this new and better adherence tool, allowing the evaluation of each patient's psychoactive drug, has helped us to further establish evidence that socio-demographic and clinical variables of the patient may have no important role in adherence, while the patient's attitudes and beliefs toward his/her medication may have a very strong role. The patient's preference (Cooper & Norcross, 2016) and self-motivation (Marín-Navarrete et al., 2017) can help to select the best treatment (Beutler, Someah, Kimpara, & Miller, 2016) for each patient and contribute to improve adherence.
This study has focused on drug treatment adherence at the drug level. It remains to be established how to define adherence at the patient level when the patient shows different degrees of adherence to various prescribed psychotropic drugs. The authors of the original tool defined adherence at the patient level as “the adherence level for the drug for which the patient was the most non-adherent” (Sidorkiewicz et al., 2016). However, we believe that this aspect of adherence needs a detailed analysis that should be the subject of future works because adherence to some psychoactive drugs may not be relevant for adherence to other psychoactive drugs.
Some limitations concerning the methodology of this study need to be noted. Although the patients’ participation rate was really high, we cannot ignore the possible existence of a selection bias. Moreover, the patients studied are from a convenience sample of consecutive psychiatric patients who attended outpatient services and, therefore, may not be representative of the entire population of psychiatric patients. Finally, all questionnaires used were self-reports and therefore may be subject to response biases.
In conclusion, the present study advances evidence for the predictive validity of the Spanish version of the Sidorkiewicz instrument for assessing treatment adherence for each individual drug taken by a psychiatric patient, providing relevant information about medicine-taking behaviors with a new “drug by drug” perspective.
The authors thank Lorraine Maw, MA, for editorial assistance.