Response to psychological treatment for Obsessive-Compulsive Disorder (OCD) varies, and dropout and relapse rates remain troubling. However, while studies examining symptom reductions are favourable, outcomes are less encouraging when outcome is defined in terms of clinically significant change. Moreover, there is little understanding of what predicts treatment outcome. This study examined demographic, symptomatic and cognitive predictors of outcome in 79 participants undertaking individualised cognitive-behavioural therapy for OCD. After investigating differences between treatment completers and non-completers, we examined treatment response as defined by post-treatment symptom severity and clinically reliable change, as well as predictors of treatment response. Completers were less likely to present with co-morbidity. The treatment was highly efficacious irrespective of whether completer or intention-to-treat analysis was undertaken, with 58% of treatment completers considered “recovered” at post-treatment. Lower pre-treatment levels of OCD symptoms and greater perfectionism/intolerance of uncertainty were the best unique predictors of OCD severity outcomes at post-treatment. Changes in obsessional beliefs were associated with symptomatic change, although only perfectionism/intolerance of uncertainty was a significant unique predictor of post-treatment change. Recovery status was predicted only by pre-treatment OCD severity. In helping to identify those at risk for poorer outcomes, such research can lead to the development of more effective interventions.
La respuesta al tratamiento psicológico para el Trastorno Obsesivo-Compulsivo (TOC) es variable, y las tasas de abandono y recaída son preocupantes. Mientras los estudios que analizan la reducción de los síntomas son favorables, los resultados son menos alentadores cuando estos se definen en términos de cambio clínicamente significativo. Existe poco conocimiento de lo que predice el resultado del tratamiento. Este estudio examinó predictores demográficos, sintomáticos y cognitivos de los resultados en 79 participantes en terapia cognitivo-conductual individualizada para el TOC. Después de investigar las diferencias entre los que completaron el tratamiento y no lo finalizaron, se analizó la respuesta al tratamiento según la definición de gravedad post-tratamiento de los síntomas y el cambio clínicamente fiable, así como predictores de la respuesta al tratamiento. Los que completaron el tratamiento eran menos propensos a presentar comorbilidad. Baja intensidad de síntomas en el pre-tratamiento y mayor perfeccionismo/intolerancia a la incertidumbre fueron los mejores predictores de los resultados. Los cambios en las creencias obsesivas se asociaron con el cambio sintomático, aunque sólo perfeccionismo/intolerancia a la incertidumbre fue predictor del cambio post-tratamiento. Esta investigación puede conducir al desarrollo de - intervenciones más eficaces.
Obsessive Compulsive Disorder (OCD) is characterized by recurrent obsessions and compulsions that cause significant distress and impairment. The last 20 to 30 years has seen the development of psychological interventions that have been shown to be effective (Fisher & Wells, 2005; McKay et al., 2015; Öst, Havnen, Hansen, & Kvale, 2015; Romanelli, Wu, Gamba, Mojtabai, & Segal, 2014; Williams, Mugno, Franklin, & Faber, 2013). Subsequently, the prognosis for individuals with OCD has changed from poor to good, primarily with the application of behavioural and cognitive techniques (McKay et al., 2015; Öst et al., 2015), although in practice most treatment programs for OCD encompass both intervention types in the form of cognitive-behaviour therapy (CBT). Despite the relative success for those who complete these treatments, a significant percentage of those treated do not recover to a substantial degree and there is relatively little data available on the longer-term maintenance of gains, while drop outs and relapses remain high (Fisher & Wells, 2005).
Exposure with response prevention (ERP) is the most prominent intervention for OCD, although patients often encounter difficulties with the demands of ERP which may partly account for high drop-out rates and poor treatment adherence (Kyrios, 2003). Cognitive therapy (CT), which uses techniques such as behavioural experiments to correct erroneous beliefs and appraisals relevant to OCD (Olatunji, Davis, Powers, & Smits, 2013), appears to be a helpful additional treatment option in many cases (Wilhelm, Berman, Keshaviah, Schwartz, & Steketee, 2015), but may not provide the critical impact on reducing drop-outs and improving treatment response that was initially hoped (Olatunji et al., 2013).
Despite pronouncements about the relative efficacy and effectiveness of cognitive and behavioural interventions, comparison of treatment evaluations has been hampered by a number of methodological limitations. Firstly, the delivery of CBT remains unreliable, with few manualised or standardized formats available where treatment integrity can be evaluated. Secondly, symptoms still persist at moderate levels in most patients, but few studies report the degree of clinical change. Jacobson and Truax (1991) consider the notion of “clinically significant change” and specify a standardized methodology for examining substantial and reliable reduction in symptom severity. Fisher and Wells (2005) applied this standardized methodology to evaluate psychological outcome trials for OCD. They reported that ERP was the most effective treatment with 50-60% of patients recovering, but much lower recovery rates (25%) for both ERP and CBT when using asymptomatic criteria. This suggests that we may need to reflect on what methods we use to define treatment outcome, and examine which patients are at risk of dropping out of treatment or are likely to show a less significant treatment response.
The identification of predictors of reliable treatment outcomes represents one critical area requiring ongoing investigation (Olatunji et al., 2013). Studies of outcome determinants may allow the targeting or addition of specific treatment strategies for those at risk of poorer outcome. Predictor variables can be classified into eight broad classes: (a) demographic variables; (b) characteristics of OCD symptoms such as severity; (c) comorbidity and associated symptom severity; (d) cognitive influences; (e) motivational factors such as treatment expectations; (f) treatment factors (e.g. compliance, therapeutic alliance); (g) biological factors; and (h) other factors (e.g., personality, family, treatment-specific characteristic, see Keeley, Storch, Merlo, & Geffken, 2008; Kyrios, 2003).
A review of clinical predictors of response to CBT concluded that, despite inconsistencies in the literature, some salient predictors have emerged (Keeley et al., 2008), although there are inconsistencies in the literature (Olatunji et al., 2013; Ponniah, Magiati, & Hollon, 2013). This paper will focus on the first four factors as these are commonly assessed at time of presentation and would be useful in identifying predictors of outcome and appropriateness of CBT in the management of OCD.
Severity of OCD symptoms has been identified as a predictor of poorer outcome in numerous studies (for an overview see Knopp, Knowles, Bee, Lovell, & Bower, 2013), although not consistently. Using CT, Steketee et al. (2011) found a marginal effect for symptom severity on outcome. Consistent with older investigations or reviews of ERP (Steketee & Shapiro, 1995), a more recent meta-analysis investigating the efficacy of cognitive-behavioural therapies indicated that pre-treatment OCD severity did not predict outcome (Olatunji et al., 2013). However, using clinically significant change as a marker of successful outcome may lead to more consistent findings from treatment studies. Olatunji et al. (2013) also concluded that depression symptom severity also failed to predict outcome, although specific studies have supported the prognostic utility of depression with respect to poorer outcome (e.g. Thiel et al., 2014). The literature has also been inconsistent with respect to the utility of anxiety severity predicting poorer outcomes (Knopp et al., 2013; Steketee & Shapiro, 1995). However, more severe affect may have a differential effect on OCD treatment outcomes. Furthermore, there may be distinct effects on outcome for initial depression severity versus changes in depression during treatment. Investigating the effects of severe depression in ERP, Abramowitz, Franklin, Street, Kozak, and Foa (2000) divided OCD patients into groups depending on their initial depressive symptom severity. Severe depression was associated with worst outcome relative to those with moderate, mild, or no depression. In an adolescent residential cohort with OCD, Leonard, Jacobi, Riemann, Lake, and Luhn (2014) found that, while initial depression severity was associated with initial OCD severity, no relationship was found with post-treatment OCD severity after accounting for pre-treatment severity. However, greater amelioration of depression during treatment predicted post-treatment OCD severity after controlling for pre-treatment severity.
In an earlier review of predictors of outcome, Steketee and Shapiro (1995) concluded that not only did duration and severity of symptoms fail to predict outcomes, neither did age, gender, marital status, education level, nor living arrangements. In contrast, various studies have found that psychosocial factors play an important role in the long-term course of OCD. For instance, in a systematic review of predictors and moderators of response to psychological treatment for OCD, Knopp et al. (2013) found that unemployment and being single were predictors of poorer outcomes. Hence, there is no universal agreement about the predictive utility of severity and demographic factors in the treatment of OCD.
Adaptive cognitive changes have also been investigated as predictors of outcome. Belloch, Cabedo, and Carrió (2008) reported that both ERP and CT led to generally large magnitude changes in OCD-relevant cognitions, although they did not examine the relationship between outcome and cognitive changes. Emmelkamp, van Oppen, and van Balkom (2002) found that treatment responders and non-responders could be differentiated on the basis of their improvement on cognitive measures. Furthermore, Overton and Menzies (2005) reported that changes in perceptions of danger, intolerance of uncertainty and need to control thoughts correlated significantly with amelioration of checking symptoms. This was not the case for responsibility, overimportance of thoughts and confidence in memory. Aardema, Emmelkamp, and O’Connor (2005) found that patients decreasing symptoms pre- to post-treatment by more than 33% decreased significantly more on inferential confusion and secondary inference compared to non-responders. Interestingly, baseline cognitive measures failed to predict treatment outcome. In a recent study investigating mechanisms of change in CT for OCD, Wilhelm et al. (2015) reported that OCD-related beliefs such as perfectionism and intolerance of uncertainty mediated OCD severity at the end of treatment. More specially, these cognitive changes preceded behavioural symptom reduction. However, there is little clarity about the relationship between cognitive change and clinically significant symptom amelioration.
While these findings are promising in gaining a better understanding of how and for whom (i.e., what characteristics) psychological treatments work, there is still a lack of empirical evidence to understand the relative contributions of predictor variables on treatment outcomes, inclusive of treatment completion, end-treatment severity accounting for initial severity, clinically significant treatment response and relapse. Hence, the current study aimed to evaluate the efficacy of a manualised CBT treatment for OCD in a controlled study, and to examine a range of predictors of treatment non-completion, response, and relapse. We expected that, in accordance with existing literature (Fisher & Wells, 2005) CBT would affect statistically significant treatment amelioration, as well as clinically reliable change in around 50-60% of participants. We further expected that we would be able to identify predictors of symptom amelioration and characteristics of non-completers, non-responders, and relapsers. Although the literature is characterised by mixed results, on balance, it was expected that higher symptom severity, greater comorbidity, especially with respect to depression, and less adaptive cognitive factors would be associated with poorer treatment outcomes. It was hoped that examining predictors of clinically reliable symptomatic change would add some clarity to the outcome literature.
MethodParticipantsThe initial sample consisted of 79 participants (63.3% female) with a mean age of 36.2 years, referred to a university clinic from a range of sources (general practitioners, psychiatric services, private psychiatrists, self-referrals, consumer groups, psychologists), with a primary diagnosis of OCD. Each participant was assessed using clinical and structured diagnostic interviews to confirm diagnosis and Axis I comorbidity. Inclusion criteria were a primary diagnosis of OCD with a minimum symptom duration of 1 year, and being 18 years or older. Participants were excluded from the study if they had a comorbid psychotic disorder, or a neurological or substance related disorder. Participants were also excluded if they had received CBT within the last 6 months, or initiation or change of medication in the 3 months prior to initial assessment. Participants presented at assessment with the following primary OCD symptoms: checking compulsions and related concerns (43%), contamination fears and washing (27%), repeating rituals (26%), counting (13%), ordering or arranging rituals (3%), obsessions with no overt compulsions (25%), hoarding (4%), or miscellaneous concerns or compulsions (30%).
ProcedureAt intake assessment, participants were administered a structured diagnostic interview, given a detailed description of the treatment process, placed on a wait list, and completed symptomatic, and cognitive measures. Following an average 10 week wait list period (range 5–18 weeks), participants began a structured treatment program consisting of 16 weekly one-to-one 50minute sessions with a CBT trained therapist. Therapists used a manualised approach that allowed for specific interventions to be tailored to the participant (Kyrios & Hordern, 2006). The manual included an emphasis on both exposure and response prevention (ERP) and cognitive therapy (CT) strategies. Treatment was conducted by trainee psychologists under the weekly supervision of a senior clinician. All therapists and supervisors participated in regular group supervision to maintain treatment integrity. Following all sessions, therapists completed treatment integrity checklists. Supervision, recordings of sessions, and integrity checklists all indicated excellent adherence to the treatment protocol.
MeasuresThe Anxiety Disorders Interview Schedule for DSM-IV (ADIS-IV; Brown, DiNardo, & Barlow, 1994) was used to confirm the OCD diagnosis and the presence of other Axis I disorders at initial assessment. The ADIS-IV is a semi-structured interview designed to assess anxiety, mood, somatoform and substance abuse disorders according to DSM-IV criteria, and screen for additional disorders such as psychosis. The ADIS-IV has shown to exhibit adequate inter-rater reliability for principal DSM-IV disorders (Brown et al., 1994).
The following data was collected at four time points: initial assessment, beginning of treatment (pre), end of treatment (post) and 6-month follow-up.
The Yale-Brown Obsessive–Compulsive Scale (YBOCS; Goodman et al., 1989) is a semi-structured interview severity measure designed to identify the duration, control, and distress associated with obsessive and compulsive behaviours. The YBOCS is considered the gold standard measure of OCD severity and is the most widely used treatment outcome measure. The clinician administered version was used at pre-, post-treatment, and follow-up.
Beck Depression Inventory (BDI; Beck & Steer, 1987). The BDI is a 21-item questionnaire to rate the severity of depression, with excellent psychometric properties.
Beck Anxiety Inventory (BAI; Beck & Steer, 1990) is a 21-item measure of anxiety with a focus on physiological symptoms of anxiety, with excellent psychometric properties.
Obsessional Belief Questionnaire (OBQ; Obsessive Compulsive Cognitions Working Group, 2005) is a 44-item scale designed to measure the strength regarding beliefs associated with obsessions. Three factor-analytically derived subscales are scored: (a) inflated personal responsibility and harm overestimation; (b) perfectionism and intolerance of uncertainty; and (c) importance and control of intrusions. Internal consistency is high for the three subscales.
ResultsPreliminary analysesAttritionOf the 79 patients who were offered and accepted treatment, 59 (75%) completed treatment (completer) and 20 (25%) dropped out during treatment or were excluded due to a change in medication (non-completer). Participants were considered to have completed treatment if they attended at least eleven sessions and completed post-treatment assessment. Of the original treatment completers, 85% were available for follow-up assessment at 6 months.
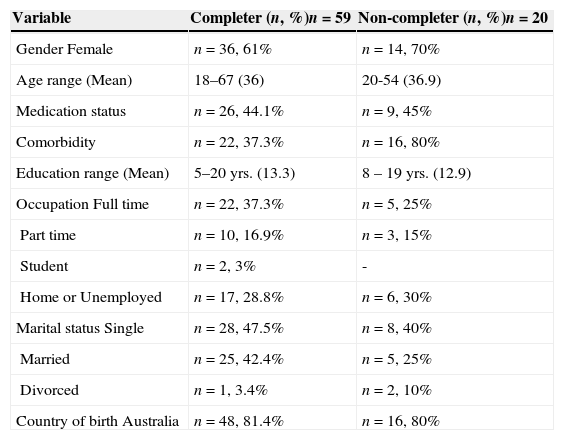
Treatment completersCharacteristics of treatment completers and non-completers are presented in Table 1. Completers (61% female) were an average age of 36 years (range=18–67). Their average years of education was 13.3 (range=5–20) and over 50% held either full or part-time employment. The sample was predominantly Australian by birth (81%), and English speaking (86%). Completers did not differ significantly from non-completers on age, gender, marital status, country of birth, employment status or medication use. However, completers were found to have a significantly lower rate of co-morbidity [χ2(1)=11.46, p=.001]. In particular, completers demonstrated lower rates of Major Depressive Disorder than non-completers (34% vs. 60%) [χ2(1)=5.33, p=.021]. However, independent samples t test performed on initial symptom levels found no significant differences between completers and non-completers on measures of severity for OCD symptoms (YBOCS), depression (BDI), or anxiety (BAI). Hence, further analyses focused on completers only, although intention-to-treat (ITT) analyses were also completed to confirm the pattern of findings.
Characteristics of treatment completers and non-completers.
| Variable | Completer (n, %)n=59 | Non-completer (n, %)n=20 |
|---|---|---|
| Gender Female | n=36, 61% | n=14, 70% |
| Age range (Mean) | 18–67 (36) | 20-54 (36.9) |
| Medication status | n=26, 44.1% | n=9, 45% |
| Comorbidity | n=22, 37.3% | n=16, 80% |
| Education range (Mean) | 5–20 yrs. (13.3) | 8 – 19 yrs. (12.9) |
| Occupation Full time | n=22, 37.3% | n=5, 25% |
| Part time | n=10, 16.9% | n=3, 15% |
| Student | n=2, 3% | - |
| Home or Unemployed | n=17, 28.8% | n=6, 30% |
| Marital status Single | n=28, 47.5% | n=8, 40% |
| Married | n=25, 42.4% | n=5, 25% |
| Divorced | n=1, 3.4% | n=2, 10% |
| Country of birth Australia | n=48, 81.4% | n=16, 80% |
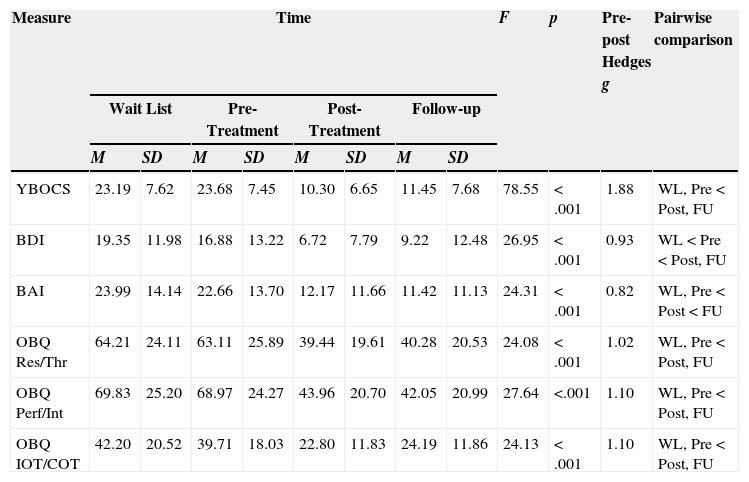
Means and standard deviations for outcome measures over the four time periods are presented in Table 2 for treatment completers. Repeated measures ANOVAs were conducted using treatment completers only (intention to treat analyses [ITT] yielded the same pattern of results). Analysis with the 59 participants who began and completed treatment showed significant treatment effects for OCD severity (YBOCS), depression (BDI) and anxiety levels (BAI), and obsessional beliefs (OBQ subscales) over the study period. Subsequent pairwise comparisons with post hoc analysis (Bonferroni adjusted) indicated significant change from pre- to post-treatment on all measures, with gains maintained at follow-up. Participants changed from pre- to post-treatment on average by 13.39 points on the YBOCS (pre-treatment range: 6–39, post-treatment range: 0–27), by 10.15 points on the BDI (pre-treatment range: 0–57, post-treatment range: 0–44), and by 10.58 points on the BAI (pre-treatment range: 0–62, post-treatment range: 0–51). There were no significant changes on measures from wait-list to beginning of treatment, except for BDI. Hedge's g was 1.88 for pre-to-post and 1.61 for pre-to-follow-up YBOCS scores, respectively, for treatment completers. The remaining analyses examined predictors of outcome and remission.
Means (M) and standard deviations (SD) on outcome measures and repeated measures ANOVAs for treatment completers.
| Measure | Time | F | p | Pre-post Hedges g | Pairwise comparison | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wait List | Pre-Treatment | Post-Treatment | Follow-up | |||||||||
| M | SD | M | SD | M | SD | M | SD | |||||
| YBOCS | 23.19 | 7.62 | 23.68 | 7.45 | 10.30 | 6.65 | 11.45 | 7.68 | 78.55 | <.001 | 1.88 | WL, Pre<Post, FU |
| BDI | 19.35 | 11.98 | 16.88 | 13.22 | 6.72 | 7.79 | 9.22 | 12.48 | 26.95 | <.001 | 0.93 | WL<Pre<Post, FU |
| BAI | 23.99 | 14.14 | 22.66 | 13.70 | 12.17 | 11.66 | 11.42 | 11.13 | 24.31 | <.001 | 0.82 | WL, Pre<Post<FU |
| OBQ Res/Thr | 64.21 | 24.11 | 63.11 | 25.89 | 39.44 | 19.61 | 40.28 | 20.53 | 24.08 | <.001 | 1.02 | WL, Pre<Post, FU |
| OBQ Perf/Int | 69.83 | 25.20 | 68.97 | 24.27 | 43.96 | 20.70 | 42.05 | 20.99 | 27.64 | <.001 | 1.10 | WL, Pre<Post, FU |
| OBQ IOT/COT | 42.20 | 20.52 | 39.71 | 18.03 | 22.80 | 11.83 | 24.19 | 11.86 | 24.13 | <.001 | 1.10 | WL, Pre<Post, FU |
Note. YBOCS=Yale Brown Obsessive Compulsive Scale Total; BDI=Beck Depression Inventory Total; BAI=Beck Anxiety Inventory Total; OBQ Res/Thr=Obsessional Belief Questionnaire: Personal responsibility and harm overestimation; OBQ Perf/Int=Obsessional Belief Questionnaire: Perfectionism and Intolerance of Uncertainty; OBQ IOT/COT=Obsessional Belief Questionnaire: Importance and control of intrusions.
A hierarchical linear regression analysis was conducted to examine the prediction of post-treatment OCD symptom severity from initial severity levels of OCD, depression and anxiety. Only pre-treatment OCD symptom severity significantly predicted post-treatment OCD outcome, and explained 20.6% of the variance in post-treatment YBOCS scores [t(57)=3.84, p<.001, β=.45].
Next, comorbidity and medication status were tested as predictors for post-treatment OCD severity (while controlling for initial OCD symptoms). Neither, comorbidity, nor medication significantly predicted OCD outcome.
Predicting treatment outcome from sociodemographic variablesSeparate hierarchical linear regression analyses were conducted predicting post-treatment OCD symptom severity from the following sociodemographic variables, respectively (while controlling for initial OCD severity): gender, age, relationship (single vs. in a relationship), and years of education. With the exception of years of education, no sociodemographic variable significantly predicted post-treatment OCD symptom severity. After controlling for initial OCD severity, years of education explained an additional 6.9% in post-treatment OCD severity scores, where more years spent in formal education were related to better outcomes in post-treatment OCD severity [t(52)=-2.23, p=.030, β=-.27].
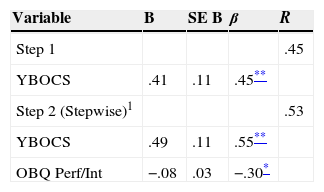
Predicting treatment outcome from initial assessmentWe examined pre-treatment predictors of post-treatment OCD symptom severity controlling for initial OCD severity scores (see Table 3). Pre-treatment level of OCD symptoms (YBOCS) was entered as step 1. Subsequent steps consisted of stepwise entry of measures of pre-treatment OCD-related beliefs (OBQ scales). Only pre-treatment perfectionism/intolerance of uncertainty was a significant predictor accounting for an additional 8.1% of variance in post-treatment YBOCS [F(1,56)=6.35, p=.015]. Both pre-treatment YBOCS and OBQ Perfectionism/Intolerance of Uncertainty were significant unique predictors of post-treatment OCD severity [t(56)=4.62, p<.001, β=.55, and t(56)=-2.52, p=.015, β=-.30, respectively]. Hence, lower pre-treatment levels of OCD symptoms and greater perfectionism/intolerance of uncertainty were the best unique predictors of better OCD severity outcomes at post-treatment.
Summary of hierarchical regression analysis predicting level of OCD symptoms at treatment end from pre-treatment variables.
| Variable | B | SE B | β | R |
|---|---|---|---|---|
| Step 1 | .45 | |||
| YBOCS | .41 | .11 | .45** | |
| Step 2 (Stepwise)1 | .53 | |||
| YBOCS | .49 | .11 | .55** | |
| OBQ Perf/Int | −.08 | .03 | −.30* |
Note.1 Variables in Step 2 were all at pre-treatment: YBOCS=Yale Brown Obsessive Compulsive Scale Total; OBQ Perf/Int=Obsessional Belief Questionnaire: Perfectionism and Intolerance of Uncertainty. R2=.20 for step 1 (p<.001); R2=.28 for step 2 (p=.015).
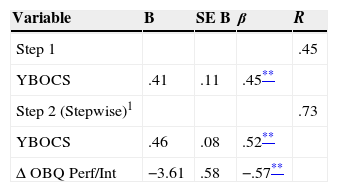
Next, we examined standardised pre- to post-treatment change scores in OCD-related beliefs as predictors of OCD symptom severity at post-treatment, while controlling for initial OCD severity scores (see Table 4). After controlling for initial OCD severity scores, standardised pre- to post-treatment change scores in OCD-related beliefs were entered stepwise. The same pattern of results were observed: only pre- to post-treatment change scores in perfectionism/intolerance of uncertainty was a significant predictor accounting for an additional substantial 32.6% of variance in post-treatment YBOCS [F(1,56)=39.01, p<.001]. Both pre-treatment YBOCS and pre- to post-treatment change scores in OBQ Perfectionism/Intolerance of Uncertainty were significant unique predictors of post-treatment OCD severity [t(56)=5.60, p<.001, β=.52, and t(56)=-6.25, p<.001, β=-.57, respectively]. Hence, lower pre-treatment levels of OCD symptoms and greater change in perfectionism/intolerance of uncertainty were the best unique predictors of better OCD severity outcomes at post-treatment.
Summary of hierarchical regression analysis predicting level of OCD symptoms at treatment end from change score in obsessional beliefs.
| Variable | B | SE B | β | R |
|---|---|---|---|---|
| Step 1 | .45 | |||
| YBOCS | .41 | .11 | .45** | |
| Step 2 (Stepwise)1 | .73 | |||
| YBOCS | .46 | .08 | .52** | |
| Δ OBQ Perf/Int | −3.61 | .58 | −.57** |
Note.1 Variables in Step 2 were all standardised change scores from pre- to post-treatment: YBOCS=Yale Brown Obsessive Compulsive Scale Total; Δ OBQ Perf/Int=standardised pre- to post-treatment change scores in Obsessional Belief Questionnaire: Perfectionism and Intolerance of Uncertainty. R2=.20 for step 1 (p<.001); R2=.53 for step 2 (p<.001).
To explore the relationship between post-treatment OCD symptom severity and change in OCD symptoms and change indices in obsessional beliefs, bivariate correlations were conducted. Moderate-to-large magnitude negative correlations were found between pre- to post-treatment changes in OCD severity and pre- to post-treatment changes in perfectionism/intolerance of uncertainty (r=-.58, p<.001), personal responsibility/harm overestimation (r=-.48, p<.001), and importance/control of intrusions (r=-.39, p<.001).
Clinically significant changeTo identify participants who exhibited “clinically reliable change”, we used the method suggested by Jacobson and Truax (1991) based on a combination of (a) reliable reduction in YBOCS total scores and (b) a post-treatment YBOCS score outside the dysfunctional range. “Recovered” participants were defined by a decrease in YBOCS of at least 10 points and a final score of 14 or less (Fisher & Wells, 2005). Of treatment completers, 34 (57.6%) were considered “recovered” at post-treatment assessment. At follow-up, 3 additional participants attained recovery status, but 8 no longer met the criteria for recovery. Given such low numbers of relapsers and inadequate power, it was not possible to examine differences between relapsers and maintainers.
Predicting clinically significant changeThere were no differences between recovered and non-recovered participants on gender [χ2(1)=1.15, p=284], medication status [χ2(1)=0.29, p=.594], or initial presence of major depression [χ2(1)=0.39, p=.534], or any co-morbid disorder [χ2(1)=0.15, p=.698]. Logistic regressions were performed to identify variables that predicted recovery status. In a logistic regression model, pre-treatment OCD severity symptoms were entered as the first step. Next, measures of pre-treatment OCD-related beliefs were entered stepwise to identify pre-treatment variables that predicted clinically reliable change. However, only pre-treatment OCD severity symptoms predicted post-treatment OCD outcomes [χ2(1)=4.40, p=.036, Exp(B)=1.09]. The overall model fit was poor [Hosmer and Lemeshow Test goodness-of-fit: χ2(7)=19.39, p=.007], and only classified 67.8% of participants’ recovery status correctly. None of the three OCD related beliefs added significantly predictive power to the model.
DiscussionThis study demonstrates the expected efficacy of a CBT program for individual treatment of OCD. Compared with the waitlist period, treatment saw significant reductions in OCD severity, anxiety and depression levels, and obsessional beliefs. These improvements occurred using a manualised treatment approach administered by trainee therapists under supervision. Completion, recovery and relapse rates compared well with previous research (McKay et al., 2015; Öst et al., 2015). Treatment completion without medication change or drop-out was associated only with lower rates of Major Depressive Disorder. Of particular note, mean YBOCS scores at pre-treatment were greater than 23, while end-treatment YBOCS were below 11. Both scores were similar to those from the most comparable published study using CBT and the self-report YBOCS (Whittal, Thordarson, & McLean, 2005). The recovery rate of 56% for treatment completers, as defined by clinically reliable change (Jacobson & Truax, 1991), is similar to that reported in previous research (50–60% recovery; Fisher & Wells, 2005). Despite this and the degree of symptom reduction, there was still a large proportion of participants who did not respond satisfactorily. After accounting for non-completers and relapsers, the findings highlight the need to search for additional intervention strategies that may enhance treatment. It is essential that we understand what factors determine who is not able to utilise current treatments in a way that impacts on dropout, clinically reliable symptom reduction, and relapse.
Consistent with expectations, findings indicated that higher initial OCD symptom severity was associated with poorer treatment outcome. Using different approaches, both Keeley et al. (2008) and Knopp et al. (2013) reported in their systematic reviews that symptom severity was a predictor of treatment response. For instance, Keeley et al. (2008) identified several studies reporting that greater initial OCD symptom severity was associated with poorer treatment outcomes (e.g. Mataix-Cols, Marks, Greist, Kobak, & Baer, 2002). In contrast, Olatunji et al. (2013) conducted a meta-analysis of CBT and found no relationship between outcome and initial OCD severity. Much of the variation in the literature may be accounted for by the specific type of CBT utilised. Our treatment protocol was based on a combination of ERP and CT, while previous studies have been based on CT (Steketee et al., 2011) or ERP (Steketee & Shapiro, 1995) alone. Furthermore, most previous literature has examined predictors of the extent of change in OCD symptoms rather than clinically significant change or recovery. We found that only pre-treatment OCD severity, was a significant predictor of recovery status. Consistent with our findings, Kempe et al. (2007) used logistic regression models to examine remission as defined by a YBOCS score lower than thirteen combined with a reduction of seven points compared to baseline. They also found that higher pre-treatment OCD severity was associated with poorer likely outcome. This study also used a 16-week treatment period, although their sample included a combination of cohorts undertaking CT, ERP or the combination of these with fluvoxamine. Future research needs to examine the importance of initial OCD severity in both symptom amelioration and recover, but also needs to consider how differing treatment protocols impact on findings.
That treatment completion was associated with incidence of co-morbid major depression is consistent with previous research (Thiel et al., 2014). While major depression was associated with drop-out or medication change, an interesting finding from our research was that this occurred independent of initial level of depressive symptom severity and that neither initial depression or anxiety levels, nor medication status predicted outcome. Perhaps a diagnosis of a MDD is more indicative for recurring or chronic high levels of depressive symptoms as distinct from temporally high levels of self-reported depressive symptoms, and therefore more likely to cause persistent interference in treatment engagement. In general, depression may impact on treatment success through its influence on motivation, behavioural activation and their effects on discouraging ERP. A study by Zitterl et al. (2000) found that as OCD symptoms decreased during CBT intervention, depression levels improved, too, and suggested that comorbid depression is not indicative of treatment prognosis in OCD. Consistent with Abramowitz (2004), our treatment protocol included an initial focus on behavioural activation, activity management and CT for mood problems which may account for our findings.
Given that recent research has highlighted the association between symptomatic amelioration and the adoption of more adaptive beliefs, we were particularly interested in examining cognitive predictors of treatment outcome. We found that conviction in all OCD-related cognitions decreased with treatment and that those changes were maintained at follow-up. While initial OCD-related beliefs did not predict recovery status, we found that changes in all OCD-related cognitions correlated significantly with changes in OCD severity. Of particular note, initial levels of perfectionism and intolerance of uncertainty, as well as changes in this cognitive style, were unique predictors of outcome.
Perfectionism can be conceptualised as involving attempts to minimise mistakes to dispel feelings of uncertainty provoked by one's intrusive thoughts (Obsessive Compulsive Cognitions Working Group, 2005). Perfectionism relating to doubts about one's actions has been found to correlate highly with OCD severity, and recent research has supported the role of perfectionism in impeding response to CBT especially with respect to post-treatment levels of compulsive symptoms (Wilhelm et al., 2015). Such findings are in line with Frost and DiBartolo's (2002) hypothesis that elevated perfectionism and personal rigidity may affect treatment response by interfering with a patient's ability to endure exposure, and therefore to examine the evidence regarding beliefs about intrusive thoughts. An intolerance for uncertainty or “pathological doubt” (Tolin, Abramowitz, Brigidi, & Foa, 2003) may be of importance not only as related to exaggerated beliefs about the probability and cost of unwanted outcomes, but also to heightened feelings of distress when faced with multiple possibilities. In treatment, a de-catastrophising of uncertainty (Tolin et al., 2003) is required which forces a weakening of the association between uncertainty and high levels of anxiety.
Future developments of treatment manuals may need to incorporate a stronger focus on changing perfectionistic beliefs in order to enhance treatment outcomes, possibly early in treatment. Wilhelm et al. (2015) found that changes in perfectionism and intolerance of uncertainty beliefs preceded behavioural symptom reduction for OCD patients and mediated successful treatment response. Furthermore, Manos et al. (2010) reported that change in perfectionism and uncertainty from pre- to post-treatment was a unique predictor for global change in OCD severity. Egan, Wade, and Shafran (2011) proposed perfectionism as a “transdiagnostic process” involved in numerous psychological disorders such as anxiety disorders, depression and eating disorders. Their model describes clinical perfectionism as a vicious cycle stemming from performance related behaviour, (e.g., constant performance checking), and counter-productive behaviours (e.g., avoidance, procrastination). Based on the model of clinical perfectionism, a CBT approach towards treating perfectionism has been developed (Egan, Wade, Shafran, & Antony, 2014). However, ongoing research is also required to further delineate which specific aspects of perfectionism are associated with poorer recovery in order to develop improved treatments. Furthermore, additional theoretical models have been proposed outlining the nature of perfectionism in OCD.
Previous theoretical discourse has identified perfectionism as a defensive strategy for protecting positive internal representations of the self (Guidano & Liotti, 1983). According to this theory, individuals with OCD have an ambivalent sense of self-worth based on early developmental influences and resulting insecure attachments. Hence, they are more likely to notice and become preoccupied with ego-dystonic intrusive experiences which conflict with their implicit sense of moral self. Self-ambivalence has been found to be positively associated with OCD severity and OCD-relevant beliefs such as perfectionism, with some evidence emerging of its relevance to treatment outcomes (Bhar & Kyrios, 2007; Bhar, Kyrios, & Hordern, in press). Bhar et al. (in press) reported that, although not directly addressed in treatment, self-ambivalence was found to predict symptom reduction. It remains to be seen whether a focus on self and morality-related aspect of OCD in treatment effects levels of perfectionism and, hence, improves outcomes. Nonetheless, a range of interventions focusing on the self have recently emerged that may usefully be adapted for OCD. For instance, narrative approaches have been used in the treatment of other anxiety disorders (Gonçalves & Stiles, 2011), while self construals are targeted either implicitly or explicitly in emerging theoretical perspectives and interventions; e.g., dialogical self (Hermans & Gieser, 2012), mindfulness (Segal, Williams, & Teasdale, 2012), Acceptance and Commitment Therapy (Hayes, Strosahl, & Wilson, 2011).
The relapse rate in the current study was too low to allow any reliable statistical analysis of the differences amongst groups. OCD is characterized as a chronic disorder that is prone to relapse particularly in times of high stress. Although the relapse rate of evidence-based psychological treatments for OCD is relatively low generally (e.g. McKay et al., 2015), it is still of importance to determine whether the addition of cognitive techniques might reduce relapse even further. For instance, as yet unpublished data (Bhar, 2004; Kyrios, Hordern & Bhar, 2001) found that resolution of self-ambivalence during treatment was associated with lower relapse in compulsions. Future studies with larger sample sizes might be better able to identify cognitive and self-related factors associated with relapse in order to indicate possibilities for additional intervention strategies.
There is an ongoing need to identify those at risk for poorer outcomes following treatment for OCD in order to develop more effective treatments. The present study identified symptomatic, and cognitive factors that were associated with recovery status as defined by end-treatment severity and clinically reliable change. On the basis of our findings, it would seem prudent for treatments to focus on such factors so as to maximize outcomes. However, we need to be cognisant of the likelihood that specific findings may reflect the nature of the treatments that we utilise and the nature of the cohorts that we treat in our clinics, although they may also point to other factors requiring targeting. At present the treatment outcome prediction literature is littered with inconsistencies, inclusive of how outcome is defined, specific variables used and identified as predictors of outcome, and the precise treatment protocols used. Future research will need to account for such issues before we are able to use the literature in order to base clinical decisions about the type of treatment recommended for individuals presenting with specific characteristics.
The authors would like to thank the University of Melbourne Psychology Clinic for their help in recruiting participants, as well as Drs. Sunil Bhar, Maja Nedeljkovic, Richard Moulding, Guy Doron, Barnaby Nelson, and Martina Jovev for their help in treating patients and collecting data. We also thank Dr. Richard Moulding for his help with earlier statistical analysis.