Background/Objective: The 11th revision of the International Classification of Diseases (ICD-11) will provide a new definition of adjustment disorder (AjD). The aim of the present study is to report on prevalence and correlates of ICD-11 AjD in a high-risk sample. Method: Three hundred thirty persons who had lost their job involuntarily were sampled by local job centres. The Munich Composite International Diagnostic Interview was administered with a new AjD module. Associations between AjD and correlates were investigated with logistic regression analyses. Results: 27.3% of the participants reported the AjD core symptom pattern. 13.8% men and 17.2% women met diagnostic guidelines of ICD-11 AjD. Prevalence increased with age and exposure to multiple stressors. The AjD core symptom pattern was associated with various sociodemographic correlates (e. g., lower financial household budget), whereas the full ICD-11 diagnosis including the exclusion algorithm was not. Regarding work-related factors, AjD occurred with a lower probability if the last job position had higher responsibilities and more general confidence for the future. Conclusions: ICD-11 AjD has a high prevalence among persons who lost their jobs involuntarily. Healthcare professionals should be aware of this problem. Research to investigate the ICD-11 AjD concept in the general populations and other subpopulations is needed.
Antecedentes/Objetivo: La versión beta de la undécima revisión de la Clasificación Internacional de Enfermedades (CIE-11) proporciona una nueva definición del trastorno de adaptación (TdA). Este estudio investiga la prevalencia y los correlatos del CIE-11 TdA en una muestra de personas de alto riesgo. Método: Se reclutaron trescientas treinta personas afectadas por una pérdida de trabajo involuntaria. Se aplicó la Munich Composite International Diagnostic Interview y un nuevo módulo del TdA. Se calcularon asociaciones entre TdA y correlatos mediante análisis de regresión logísticas. Resultados: El 27,3% de los participantes reportaron el patrón de síntomas principales de TdA. El 13,8% de los hombres y el 17,2% de las mujeres cumplieron con los criterios de diagnóstico del CIE-11 TdA. La prevalencia se relacionó con la edad y la exposición a múltiples estresores. Solamente el patrón de los síntomas principales, pero no el diagnóstico completo, correlacionó con factores socio-demográficos (e. g., presupuesto familiar). La probabilidad del TdA era más baja si el último puesto de trabajo fue de más responsabilidad y con más perspectivas de futuro. Conclusiones: Existe una prevalencia elevada del CIE-11 TdA en personas afectadas por una pérdida de trabajo involuntaria. Se precisa más investigación sobre el concepto del TdA en la CIE-11.
Adjustment disorder (AjD) can be a consequence of critical life events or other stressors, such as for example a serious illness. Mitchell et al. (2011) reported in their review and meta-analysis a high point prevalence of AjD of 19.4% of patients in oncological, and hematological care settings, and of 15.4% of patients in palliative care settings. Given that suicidality is common in this disorder (Gradus et al., 2010), these high estimates demand higher awareness and more recognition of AjD. The high prevalence in exposed samples has been confirmed by more recent studies (e. g., Hund et al., 2016). Most studies applied criteria of the Diagnostic and Statistical Manual of the American Psychiatric Association as for example DSM-IV (American Psychiatric Association APA, 1994) or used diagnostic guidelines of the 10th version of the International classification of diseases (ICD-10; World Health Organization WHO, 1992) to derive AjD diagnoses. Given that these diagnoses considered the respective exclusion rules in the presence of other disorders, the high prevalence estimates are even more considerable.
The major classification systems ICD-10 (World Health Organization WHO, 1992) and DSM-5 (American Psychiatric Association APA, 2013) define AjD as a time-limited transitional period occurring after the onset of stressors. They specify no unique AjD symptoms, but depression, anxiety, or merely emotional or behavioral symptoms constituting specific subtypes of psychopathological adjustment. That means that in these classification systems AjD has been defined with symptoms usually assigned to other disorders, mainly depressive or anxiety disorders, that exclude the AjD diagnosis when no stress or life event has occurred or symptoms could be an exacerbation of these disorders. Yet a distinction from a normal stress response is lacking, particularly in ICD-10 (World Health Organization WHO, 1992). Patra and Sarkar (2013) commented that these diagnostic principles have little diagnostic rigor and clinical utility. In fact, AjD was often unrecognized (Casey, 2014). In diagnostic instruments, AjD was until recently a residual category. Therefore, epidemiological studies on its prevalence in the general population are extremely rare. The reported 12- to 34-months estimates of 0.9% (Maercker et al., 2012) and 1% (Casey et al., 2006) are much lower than those in health care or other risk population groups shortly after or during stress exposure. For correlates and risk factors, it was reported that the probability of AjD varied by type and impact of the stressor and was associated with gender (Hund et al., 2016) and age (Chen, Chen, Chen, & Lung, 2011). Various intrapersonal factors as for example self-efficacy and coping (Forstmeier, 2013) and interpersonal factors as for example social support (Alvarado-Esquivel, Sifuentes-Alvarez, & Salas-Martinez, 2015) were identified as correlates. However, only few studies were conducted with general population samples and diagnostic assessment varies from clinical judgment (Chen et al., 2011) to questionnaires (Maercker et al., 2012) to the assessment with a standardized clinical interview module (Hund et al., 2016). Finally, there are very few prospective, longitudinal studies (Kocalevent, Mierke, Danzer, & Klapp, 2014; O’Donnell et al., 2016).
The working group of the World Health Organization (WHO) for the new category of “disorders specifically associated with stress” in the forthcoming 11th revision of the ICD was faced with the problem of few existing empirical knowledge when preparing the proposal for a new AjD concept (Maercker et al., 2013). They followed to a large extent a previously proposed stress-response model with AjD conceptualised as a maladaptive stress response, characterized by symptoms of preoccupation and failure to adapt to the stressor (Maercker, Einsle, & Kollner, 2007). The stressors will not be specified and can vary in severity and frequency of occurrence (World Health Organization WHO, 2015). The core symptom, “preoccupation with the stressor or its consequences”, is related to excessive worrying, recurrent and distressing thoughts about the stressor or constant rumination about its implications. The other core symptom, “failure to adapt to the stressor”, concerns interference with everyday functioning, such as difficulties concentrating or sleep disturbance resulting in performance problems at work or at school. Symptoms should not be of sufficient specificity or severity to justify another mental disorder diagnosis. They usually emerge within a month after the onset of the stressor and typically resolve within 6 months, unless a longer persistence of the stressor (World Health Organization WHO, 2015). To qualify for a diagnosis, symptoms must cause significant impairment in personal, familial, social, educational, occupational, or other important areas (World Health Organization WHO, 2015). ICD-11 AjD is excluded if at the same time an episode of a single episode - or recurrent depressive disorder, or a prolonged grief disorder is present. In childhood a separation anxiety disorder diagnosis is exclusive. Factors influencing health status, i.e. uncomplicated bereavement, burn-out, or acute stress reaction should also be regarded (World Health Organization WHO, 2015).
To explore basic epidemiological parameters of AjD as proposed for ICD-11 the following research questions will be investigated in a high-risk sample of persons who lost their jobs involuntary: (a) What is the prevalence of ICD-11 AjD assessed by a standardized diagnostic clinical interview? (b) Which types of stressors occur and what is the conditional probability of ICD-11 AjD? (c) Which sociodemographic and work-related characteristics are associated with ICD-11 AjD?
MethodParticipants and proceduresData from the baseline assessment of the Zurich Adjustment Disorder Study were used. This longitudinal study includes baseline assessment, 6-months- and 12 months follow-up. It is designed to investigate the prevalence, risk factors, course, and outcome of AjD as proposed for ICD-11 in participants of the Zurich region who had lost their job involuntarily within 9 months prior to the first assessment. The study was approved by the local ethics committee in June 2015. Recruitment started in September 2015 and baseline assessment was conducted from October 2015 to August 2016. Most participants were recruited consecutively via job centers in the greater Zurich area by employees of the job center. Other means of recruitment were three local newspaper articles. Persons were excluded if they were under age 18 years, did not speak German fluently, or were not able to participate due to a severe physical disease, severe mental disorder, or serious disabilities. Four hundred and sixty-three persons were interested in participation. Ninety-eight did not meet inclusion criteria, twenty-one could not be reached again, ten persons refused to participate, and four did not return questionnaires or missed the diagnostic interview. This resulted in a sample of 330 participants at the baseline assessment. Most of them had been contacted by their job centers (80%), 10.9% were recruited through newspapers, and the rest by word of mouth. All participants gave written consent after they had been informed about the aims and procedures of the study. If we detected an actual mental disorder or other serious problems during the assessment, contact information for help was provided.
Of the 330 participants, 50.6% were male and 49.4% were female. The average age of the sample was 44 years. Females (42 years) were slightly younger than males (45 years; z=-2.32, p<.05). Among the participants, 37.0% reached a high school diploma. The proportion of participants with academic job training was 43.2% due to a remarkable number of participants with a technical college entrance qualification (17.0%). There was no gender difference related to high school diploma (z=0.02, p=.87) nor to academic job training (z=-0.40, p=.69). 31.5% were married or living in a civil partnership. 37.9% had a household budget below 4000 Swiss francs. This concerned more women (43.6%) then men (32.3%, z=2.1, p<.05). 30.1% rated themselves as belonging to a low social class. This was unrelated to gender (z=0.97, p=.33) and age (z=0.77, p=.44).
InstrumentsAjD diagnosis. The diagnostic status of AjD was assessed with a new AjD module (Perkonigg, Strehle, Lorenz, Beesdo-Baum, & Maercker, 2015) of the computer-assisted Munich Composite International Diagnostic Interview (DIA-X/M-CIDI; Wittchen & Pfister, 1997). The DIA-X/M-CIDI is a standardized clinical interview that allows for the assessment of symptoms, syndromes, and diagnoses of mental disorders according to the criteria of DSM-IV (American Psychyiatric Association APA, 1994) and ICD-10 (World Health Organization WHO, 1992). Furthermore, data on onset and recency, duration, severity, and psychosocial impairment, related to the specific disorders, as well as sociodemographic information of the respondent are collected. Test–retest reliability and validity of the DIA-X/M-CIDI (Reed et al., 1998) as well as of the AjD-CIDI Module (Perkonigg, Venz, Lorenz, Beesdo-Baum, & Maercker, 2017) are fair to good. The AjD module was developed according to the new diagnostic concept for ICD-11 (World Health Organization WHO, 2015; World Health Organization's Global Clinical Practice Network, 2016) and also allows to assess DSM-5 criteria (American Psychiatric Association APA, 2013). It starts with the assessment of stressors and their characteristics during the 12 months prior to the interview. If at least one stressor is endorsed, symptoms occurring in response to the one or the most severe event as indicated by the participant before, are assessed. In a third step, information about onset and recency of symptoms, and about impairment related to work, to household, school, or leisure activities, or to social contacts is collected. The diagnostic algorithm for ICD-11 AjD considers the triggering event and the occurrence of at least one of the preoccupation core symptoms (intrusive thoughts, constant worries related to the event) as well as of at least two of the failure to adapt symptoms (concentration problems, difficulties in work/daily activities, loss of interest in social network or leisure activities, sleep problems, loss of self-confidence when with family or relatives). The one-month period from the occurrence of the stressor to the onset of symptoms and impairment due to symptoms is also regarded. The symptom frequencies among participants with or without the diagnosis are available upon request. To apply the full diagnosis, exclusive disorders have been recognized as follows.
ICD-11 AjD diagnosis and exclusive disorders. If a depressive episode of a recurrent depressive disorder or a single episode depressive disorder was present, we excluded an AjD diagnosis (World Health Organization WHO, 2015). In order to apply the ICD-11 diagnostic guidelines for these disorders, we used the ICD-11 draft guidelines (World Health Organization's Global Clinical Practice Network, 2016) and generated an algorithm with the existing depression data of the DIA-X/M-CIDI. This algorithm covers the guidelines of a depressive episode for ICD-11. Only the symptom of “hopelessness about the future” was not available. The 12-months prevalence of ICD-11 depressive episodes was high at 18.8%. We also excluded two cases with a co-occurring generalized anxiety disorder. With respect to prolonged grief disorder or uncomplicated bereavement disorder we dropped another two cases who reported the full set of ICD-11 AjD symptoms due to the death of family members or close others.
Correlates. Sociodemographic characteristics were covered by the first section of the DIA-X/M-CIDI. Specific work-related information, as for example “duration of last appointment”, was assessed with a questionnaire prepared for the study.
Statistical analysisTwo outcome variables for AjD were used. The first one operationalises the proposed stressor criterion, the symptom criteria as well as impairment in important areas of functioning (described as “core symptom pattern”). The second one uses the same diagnostic elements but considers exclusive diagnoses according to the ICD-11 Beta draft (World Health Organization WHO, 2015) and is described as “full AjD diagnoses”. 12-month prevalence proportions of AjD with 95% confidence intervals were calculated. Logistic regression analysis adjusted for gender and age were conducted to investigate associations between correlates and stressors. Odds ratios (OR) and 95% confidence intervals (95%CI) on associations between the outcomes and sociodemographic or work-related correlates are reported.
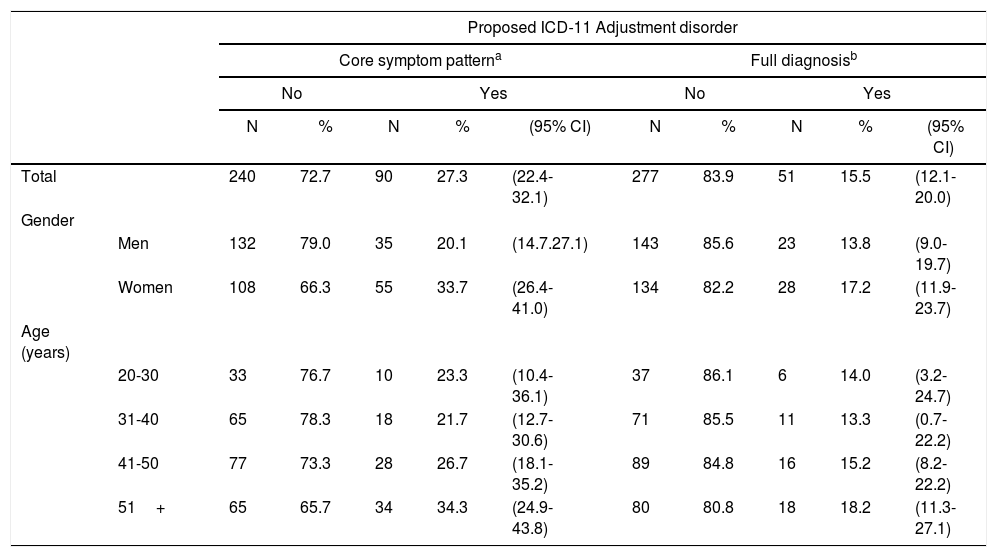
ResultsPrevalence of ICD-11 AjDAs shown in Table 1, prevalence estimates of AjD in this sample were high. 27.3% reported the presence of the AjD “core symptom pattern” occurring within one month after the stressor and associated with significant impairment. Applying the exclusion algorithm, the 12-month prevalence of the full AjD diagnosis was 15.5%. It was higher in women (17.2%) than in men (13.8%) and increased with age. More than one third of participants older than 50 years endorsed the symptom pattern, and a large proportion met the full AjD diagnosis (18.2%).
12-month prevalence estimates of ICD-11 adjustment disorder in the ZADS sample.
| Proposed ICD-11 Adjustment disorder | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Core symptom patterna | Full diagnosisb | ||||||||||
| No | Yes | No | Yes | ||||||||
| N | % | N | % | (95% CI) | N | % | N | % | (95% CI) | ||
| Total | 240 | 72.7 | 90 | 27.3 | (22.4-32.1) | 277 | 83.9 | 51 | 15.5 | (12.1-20.0) | |
| Gender | |||||||||||
| Men | 132 | 79.0 | 35 | 20.1 | (14.7.27.1) | 143 | 85.6 | 23 | 13.8 | (9.0-19.7) | |
| Women | 108 | 66.3 | 55 | 33.7 | (26.4-41.0) | 134 | 82.2 | 28 | 17.2 | (11.9-23.7) | |
| Age (years) | |||||||||||
| 20-30 | 33 | 76.7 | 10 | 23.3 | (10.4-36.1) | 37 | 86.1 | 6 | 14.0 | (3.2-24.7) | |
| 31-40 | 65 | 78.3 | 18 | 21.7 | (12.7-30.6) | 71 | 85.5 | 11 | 13.3 | (0.7-22.2) | |
| 41-50 | 77 | 73.3 | 28 | 26.7 | (18.1-35.2) | 89 | 84.8 | 16 | 15.2 | (8.2-22.2) | |
| 51+ | 65 | 65.7 | 34 | 34.3 | (24.9-43.8) | 80 | 80.8 | 18 | 18.2 | (11.3-27.1) | |
Notes. 95% CI, 95% confidence interval (rounded).
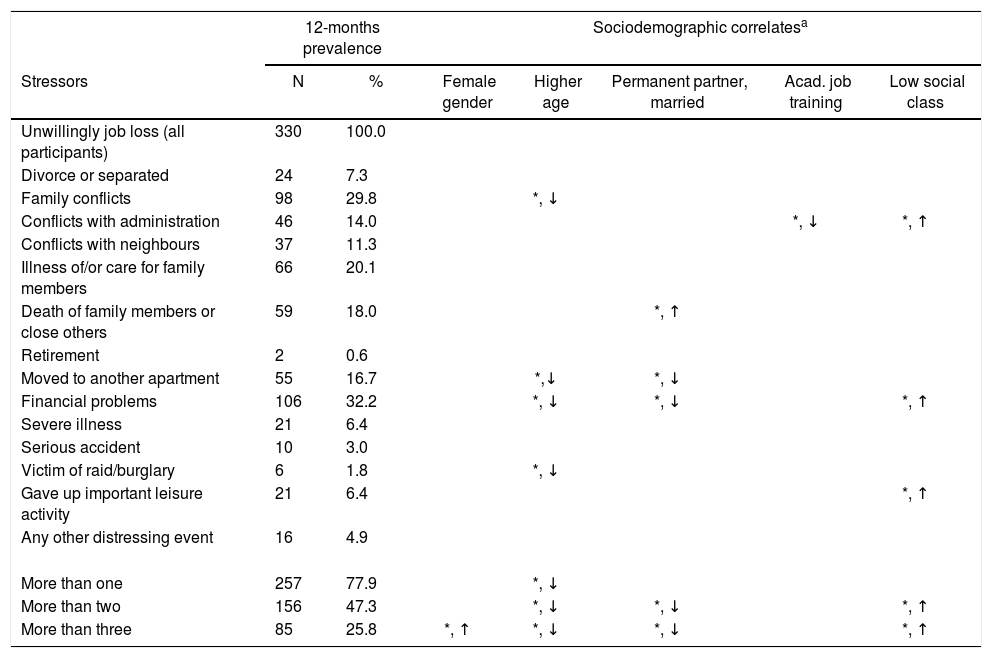
The types of stressors that were reported in the sample are shown in Table 2. All participants were exposed to involuntary job loss. Among other additional (“secondary”) stressors, financial problems were most frequent (32.2%). The five columns on the right side of Table 2 show that older age groups and participants who were married or in a permanent partnership endorsed this type of stressor significantly less often. In contrast, “financial problems” were more likely reported among participants belonging to a lower social class. The lower part of Table 2 shows that 77.9% of the sample reported more than one stressor and nearly half more than two stressors. Female gender, younger age, being unmarried or without a permanent partnership and belonging to a lower social class was associated with this group.
Types of specific stressors and their sociodemographic correlates.
| 12-months prevalence | Sociodemographic correlatesa | ||||||
|---|---|---|---|---|---|---|---|
| Stressors | N | % | Female gender | Higher age | Permanent partner, married | Acad. job training | Low social class |
| Unwillingly job loss (all participants) | 330 | 100.0 | |||||
| Divorce or separated | 24 | 7.3 | |||||
| Family conflicts | 98 | 29.8 | *, ↓ | ||||
| Conflicts with administration | 46 | 14.0 | *, ↓ | *, ↑ | |||
| Conflicts with neighbours | 37 | 11.3 | |||||
| Illness of/or care for family members | 66 | 20.1 | |||||
| Death of family members or close others | 59 | 18.0 | *, ↑ | ||||
| Retirement | 2 | 0.6 | |||||
| Moved to another apartment | 55 | 16.7 | *,↓ | *, ↓ | |||
| Financial problems | 106 | 32.2 | *, ↓ | *, ↓ | *, ↑ | ||
| Severe illness | 21 | 6.4 | |||||
| Serious accident | 10 | 3.0 | |||||
| Victim of raid/burglary | 6 | 1.8 | *, ↓ | ||||
| Gave up important leisure activity | 21 | 6.4 | *, ↑ | ||||
| Any other distressing event | 16 | 4.9 | |||||
| More than one | 257 | 77.9 | *, ↓ | ||||
| More than two | 156 | 47.3 | *, ↓ | *, ↓ | *, ↑ | ||
| More than three | 85 | 25.8 | *, ↑ | *, ↓ | *, ↓ | *, ↑ | |
Notes. * p<.05; p, probability: ↑, means higher probability of the stressor; ↓, means lower probability of the stressor.
Associations were investigated with logistic regression analyses. Only significant associations between the stressor types and the covariates of: female gender, higher age, living in a permanent partnership or married, an academic job training and the self-rating ‘belonging to a low social class’ are shown.
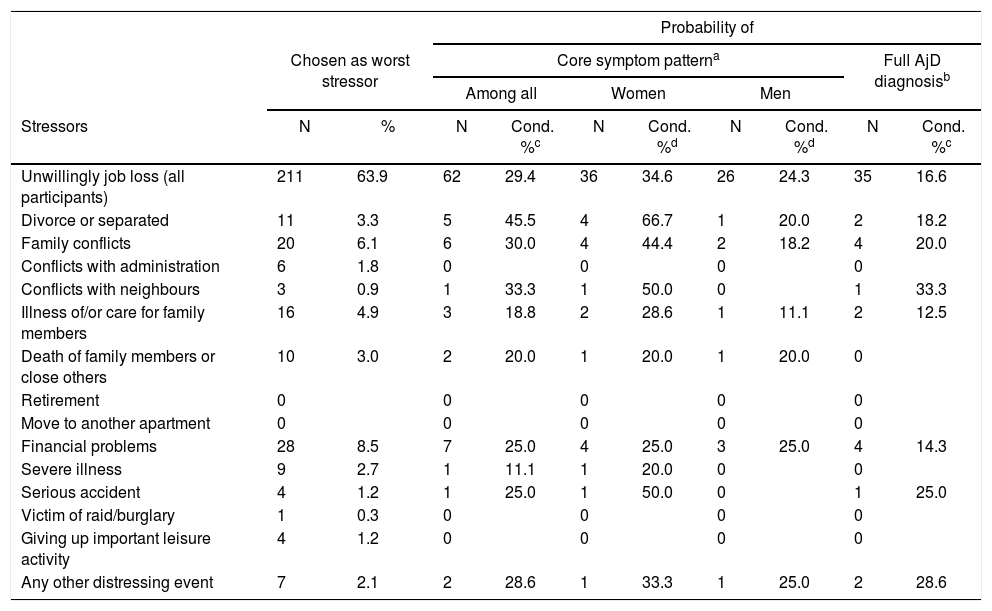
Table 3 shows the proportions of the stressors that were qualified for symptom assessment and the conditional probabilities of AjD. For the majority (63.9%) “involuntary job loss” was the only or the worst stressor. 29.4% of them developed the AjD core symptom pattern and 16.6% met the full AjD diagnosis. The stressors with the highest probability of the core symptom pattern (45.5%) were ‘divorce or separation’ from a permanent partner. The probability of a full AjD diagnosis was much lower (18.2%. Not shown in Table 3 is that if more than two stressors were reported, participants were more than two times more likely to report the symptom pattern (OR=2.1; 95%CI, 1.3-3.6). There was no more significant increase in the conditional probability of AjD if more than three events were reported.
Conditional probability of ICD-11 AjD by particular stressor types.
| Probability of | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Chosen as worst stressor | Core symptom patterna | Full AjD diagnosisb | ||||||||
| Among all | Women | Men | ||||||||
| Stressors | N | % | N | Cond. %c | N | Cond. %d | N | Cond. %d | N | Cond. %c |
| Unwillingly job loss (all participants) | 211 | 63.9 | 62 | 29.4 | 36 | 34.6 | 26 | 24.3 | 35 | 16.6 |
| Divorce or separated | 11 | 3.3 | 5 | 45.5 | 4 | 66.7 | 1 | 20.0 | 2 | 18.2 |
| Family conflicts | 20 | 6.1 | 6 | 30.0 | 4 | 44.4 | 2 | 18.2 | 4 | 20.0 |
| Conflicts with administration | 6 | 1.8 | 0 | 0 | 0 | 0 | ||||
| Conflicts with neighbours | 3 | 0.9 | 1 | 33.3 | 1 | 50.0 | 0 | 1 | 33.3 | |
| Illness of/or care for family members | 16 | 4.9 | 3 | 18.8 | 2 | 28.6 | 1 | 11.1 | 2 | 12.5 |
| Death of family members or close others | 10 | 3.0 | 2 | 20.0 | 1 | 20.0 | 1 | 20.0 | 0 | |
| Retirement | 0 | 0 | 0 | 0 | 0 | |||||
| Move to another apartment | 0 | 0 | 0 | 0 | 0 | |||||
| Financial problems | 28 | 8.5 | 7 | 25.0 | 4 | 25.0 | 3 | 25.0 | 4 | 14.3 |
| Severe illness | 9 | 2.7 | 1 | 11.1 | 1 | 20.0 | 0 | 0 | ||
| Serious accident | 4 | 1.2 | 1 | 25.0 | 1 | 50.0 | 0 | 1 | 25.0 | |
| Victim of raid/burglary | 1 | 0.3 | 0 | 0 | 0 | 0 | ||||
| Giving up important leisure activity | 4 | 1.2 | 0 | 0 | 0 | 0 | ||||
| Any other distressing event | 7 | 2.1 | 2 | 28.6 | 1 | 33.3 | 1 | 25.0 | 2 | 28.6 |
Notes. Cond.%, conditional probability.
As shown in Table 4, women were nearly two times more likely than men to endorse the core symptom pattern (OR=1.9; 95%CI, 1.2-3.1). However, gender was unrelated to a full AjD diagnosis (OR=1.3; 95%CI, 0.7-2.4). Increasing age in this sample (OR=1.1; 95%CI, 1.1-1.1) was also significantly associated with the symptom pattern but not the full diagnosis (OR=1.0; 95%CI, 1.0-1.0). Among the other sociodemographic characteristics, the available household budget with fewer than 4000 SFr. or a bad financial situation of the participant was related to the symptom pattern (OR=1.8; 95%CI, 1.1-2.7).
Sociodemographic correlates of the sample with and without ICD-11 adjustment disorder.
| Without ICD-11 AjD | With ICD-11 AjDa | Core symptom patternb | Full AjD diagnosisc | |||
|---|---|---|---|---|---|---|
| Correlates | N | % | N | % | OR (95%CI)d | OR (95%CI)d |
| Gender | ||||||
| Men | 132 | 79.0 | 35 | 21.0 | ||
| Women | 108 | 66.3 | 55 | 33.7 | 1.9 (1.2-3.1)* | 1.3 (0.7-2.4) |
| Age | ||||||
| 20-30 | 33 | 76.7 | 10 | 23.3 | ||
| 31-40 | 65 | 78.3 | 18 | 21.7 | ||
| 41-50 | 77 | 73.3 | 28 | 26.7 | ||
| 51+ | 65 | 65.7 | 34 | 34.3 | 1.1 (1.1-1.1)e,* | 1.0 (1.0-1.0)e |
| School graduation | ||||||
| Ordinary | 151 | 72.6 | 57 | 27.4 | ||
| High school | 89 | 73.0 | 33 | 27.0 | 1.0 (0.6-1.7) | 1.0 (0.6-2.0) |
| Job training | ||||||
| Vocational | 134 | 72.4 | 51 | 27.6 | ||
| Academic | 104 | 73.8 | 37 | 26.2 | 1.1 (0.7-1.8) | 1.3 (0.7-2.4) |
| Marital status | ||||||
| Not married | 157 | 69.5 | 69 | 30.5 | ||
| Married | 83 | 79.8 | 21 | 20.2 | 0.6 (0.3-1.2) | 0.9 (0.5-1.9) |
| Children | ||||||
| Without | 142 | 71.7 | 56 | 28.3 | ||
| With | 98 | 74.2 | 34 | 25.8 | 0.8 (0.4-1.3) | 0.9 (0.5-1.7) |
| Living alone | ||||||
| No | 152 | 73.4 | 55 | 26.6 | ||
| Yes | 88 | 71.5 | 35 | 28.5 | 1.1 (0.6-1.7) | 0.6 (0.3-1.1) |
| Financial situation | ||||||
| Not bad | 178 | 76.7 | 54 | 23.3 | ||
| Bad | 62 | 63.3 | 36 | 36.7 | 1.9 (1.2-3.3)* | 1.5 (0.8-2.9) |
| Household budget less than 4.000 SFr. | ||||||
| No | 157 | 76.6 | 48 | 23.4 | ||
| Yes | 83 | 66.4 | 42 | 33.6 | 1.8 (1.1-2.7)* | 1.9 (1.0-3.5) |
| Social class (subjectively) | ||||||
| Middle or higher | 173 | 75.9 | 55 | 24.1 | ||
| lower | 64 | 65.3 | 34 | 34.7 | 1.7 (1.0-2.8) | 1.3 (0.7-2.5) |
Notes. * p<.05; OR, odds ratio; 95% CI, 95% confidence interval (rounded).
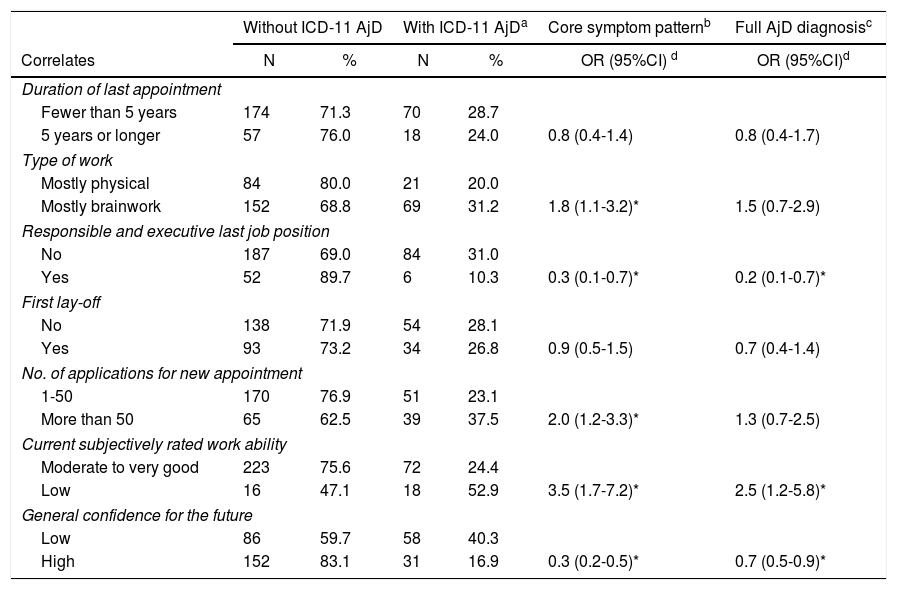
Endorsing the AjD symptom pattern was related to ‘type of work’ and ‘number of applications’ for a new appointment (see Table 5). On the other hand, if participants held a last job position with more responsibilities or executive tasks, they were significantly less likely to endorse the full symptom pattern (OR=0.3; 95%CI, 0.1-0.7) and to meet the full AjD diagnosis (OR=0.2; 95%CI, 0.1-0.7). Both AjD outcomes were associated with less confidence for the future (OR=0.3; 95%CI, 0.2-0.5; OR=0.7; 95%CI, 0.5-0.9). Further, participants with a full AjD diagnosis rated their work ability about two and a half times lower than participants without AjD (OR=2.5; 95%CI, 1.2-5.8).
Work-related correlates of ICD-11 adjustment disorder.
| Without ICD-11 AjD | With ICD-11 AjDa | Core symptom patternb | Full AjD diagnosisc | |||
|---|---|---|---|---|---|---|
| Correlates | N | % | N | % | OR (95%CI) d | OR (95%CI)d |
| Duration of last appointment | ||||||
| Fewer than 5 years | 174 | 71.3 | 70 | 28.7 | ||
| 5 years or longer | 57 | 76.0 | 18 | 24.0 | 0.8 (0.4-1.4) | 0.8 (0.4-1.7) |
| Type of work | ||||||
| Mostly physical | 84 | 80.0 | 21 | 20.0 | ||
| Mostly brainwork | 152 | 68.8 | 69 | 31.2 | 1.8 (1.1-3.2)* | 1.5 (0.7-2.9) |
| Responsible and executive last job position | ||||||
| No | 187 | 69.0 | 84 | 31.0 | ||
| Yes | 52 | 89.7 | 6 | 10.3 | 0.3 (0.1-0.7)* | 0.2 (0.1-0.7)* |
| First lay-off | ||||||
| No | 138 | 71.9 | 54 | 28.1 | ||
| Yes | 93 | 73.2 | 34 | 26.8 | 0.9 (0.5-1.5) | 0.7 (0.4-1.4) |
| No. of applications for new appointment | ||||||
| 1-50 | 170 | 76.9 | 51 | 23.1 | ||
| More than 50 | 65 | 62.5 | 39 | 37.5 | 2.0 (1.2-3.3)* | 1.3 (0.7-2.5) |
| Current subjectively rated work ability | ||||||
| Moderate to very good | 223 | 75.6 | 72 | 24.4 | ||
| Low | 16 | 47.1 | 18 | 52.9 | 3.5 (1.7-7.2)* | 2.5 (1.2-5.8)* |
| General confidence for the future | ||||||
| Low | 86 | 59.7 | 58 | 40.3 | ||
| High | 152 | 83.1 | 31 | 16.9 | 0.3 (0.2-0.5)* | 0.7 (0.5-0.9)* |
Notes. * p<.05; OR, odds ratio; 95% CI. 95% confidence interval (rounded).
The aim of the present study was to describe the prevalence, stressors, and correlates of adjustment disorder according to the new ICD-11 definition in a high-risk sample. The estimated prevalence of 15.5% shows that AjD according to the new definition occurs relatively frequently in a sample of involuntarily laid-off persons exposed to stressors that can occur in everyone's life for a circumscribed period. Although based on the proposed ICD-11 concept, the prevalence estimate is in line with findings from other high-risk populations (Gradus et al., 2010; Hund et al., 2016; Mitchell et al., 2011). It remains yet unclear whether the cases with AjD diagnoses according to the ICD-11 proposal would remain cases if diagnoses according to ICD-10 or DSM-5 would have been used. As exclusive other mental disorders will still be recognized to some extent, it seems that the new diagnostic algorithm does not largely change the prevalence of the disorder in exposed populations. The change between ICD-10 and ICD-11 occurs in the consideration of unique core symptoms (preoccupation and failure to adapt) and functional impairment. Persons with AjD in our study may also present with depressive or anxiety symptoms as described in DSM-5. However, one rationale behind ICD-11 is that these symptoms do not describe the core of maladaptive stress responses directly emanating from the realization and assimilation of the stressor. Therefore, they cannot justify a specific stress related disorder that may have another course and impact as for example a depressive disorder or a generalized anxiety disorder. However, particularly with respect to suicidality it is important to note that the AjD core symptoms may increase risk of suicidal ideation, intention or even suicide attempts (Gradus et al., 2010).
Prevalence estimates of the AjD core symptoms including impairment were higher among women than men in this sample. However, when the diagnostic exclusion algorithm was applied, this difference vanished and differences among age groups became distinctively apparent. In the study of Maercker et al. (2012), women were also significantly more likely reporting core symptoms. Contrary to Chen et al. (2011) where younger males were more likely to be screened with DSM-IV AjD, the job loss in our study could be more existentially threatening to women and may have a higher impact on older participants eventually due to missing financial resources or because consequences represent a more serious threat to their prosperity. Furthermore, we also found high rates of secondary stressors particularly among women that increased probability of AjD core symptoms. Some of them might have qualified for a depressive episode as the full diagnosis was not met.
Among the sociodemographic correlates, the unsatisfactory financial situation of the household of the participants was associated with a full AjD diagnosis in this sample. This factor is in line with the reports of secondarily distressing financial problems and it may be a specific correlate in this population. We also found that participants who held a more responsible position before were less likely to meet the full diagnosis during unemployment. This could be a marker of more available financial resources once the job has been lost. On the other hand, persons that did not meet diagnostic guidelines of AjD might have generally more personal resources including more self-efficacy that helps them to appraise the situation more challenging than dangerous and to cope with it more efficiently.
This study is outstanding as it offers the first prevalence estimates and correlates of ICD-11 AjD based on a standardized clinical interview which may have improved the diagnostic process that seems more difficult in respect of the new diagnostic guidelines of AjD (Keeley et al., 2016). Yet, it has various limitations. First, results are based on cross-sectional data and do not allow any causal interpretations. Second, data refer to self-reports. Recall bias cannot be excluded, although it is less likely, given the face-to-face interview and a relatively short 12-month assessment period of AjD symptoms. Third, results from this urban Swiss sample, with a relatively high socioeconomic status despite unemployment, might not be representative of other subpopulations. Fourth, finding on specific stressor must be carefully interpreted when reported as the one or qualified as worst stressor because they may not be independent of the involuntarily job loss that had been experienced by all participants. Fifth, as the aim of this paper was to estimate the prevalence and to investigate more sociodemographic correlates of ICD-11 AjD, we could not additionally compare persons with and without the diagnosis in respect of specific psychological constructs. Analyses of psychological factors as for example self-efficacy will be an objective of other papers that could then help to interpret the results more comprehensively. Finally, it is important to note that due to the involuntarily job loss as major characteristic of the sample, results cannot be generalized to other high-risk groups.
To conclude, the relatively high proportion of AjD in this sample may reflect a need for specific interventions for persons who lost their job involuntarily. Self-help interventions for AjD that were recently successfully investigated in another context (Bachem & Maercker, 2016) could be adapted to this distressing situation. It has further to be recognized that a large proportion of our participants also met diagnostic guidelines of depressive episodes. These persons might benefit from interventions related to an improvement of personal and social resources but also from targeted psychotherapeutic interventions for depression. Finally, it is important to examine the new AjD diagnosis in general population samples. Only such data will show whether the new diagnostic concept with a smaller list of exclusive other mental disorders is a serious mental disorder that will become a full recognizable diagnosis and will no longer remain an ill-defined category.
Funding and acknowledgementsThis work was supported by a grant of the Swiss National Science Foundation (#100019_159436) and financial support by the Jacobs Foundation. Funding sources were not involved in the conception and writing of the manuscript, the interpretation of the findings or the decision to submit it for publication. This work is part of the Zurich Adjustment disorder study. Principal investigators are Drs. Andreas Maercker and Axel Perkonigg. Coordination manager is MSc. Louisa Lorenz. We thank all respondents of the study for their participation. We also appreciate Lisa Makowski and Désirée Thommen for data collection and data processing. We acknowledge the Office of Economy and Labour Zurich for cooperation on respondents’ recruitment and Drs. Beesdo-Baum, Wittchen and Dipl. math. Jens Strehle (TU Dresden) for collaboration on the AjD CIDI module. Thanks to Dr. Eva Heim and MSc. Iara Meili, for Spanish language editing.