Background/Objective: Lower levels in well-being have been observed in individuals with Major Depression (MDD) and Social Phobia (SP), but well-planned direct comparisons with control individuals, not suffering from a mental disorder, are lacking. Furthermore, MDD is highly comorbid with anxiety disorders, and SP with depressive disorders. This study is among the first to examine differences in well-being in individuals with a clinical diagnosis of MDD or SP compared to individuals with no such diagnosis and to test differences in well-being within the combined diagnostic categories respective with and without anxiety-depressive comorbidity. Method: Participants were 119 individuals with a diagnosis of MDD, 47 SP and 118 controls. Results: Results revealed that overall well-being as well as emotional, psychological, and social well-being were lower in the MDD and SP group compared to the control group. Individuals with comorbidity reported lower well-being than individuals without comorbidity. Conclusions: These findings have clinical implications as presence of comorbidity may require a different therapeutic approach than with no comorbidity.
Antecedentes/Objetivo: Se han observado niveles bajos de bienestar en individuos con depresión grave (DG) y fobia social (FS). Sin embargo, las comparaciones directas planificadas con individuos controles que no padecen ningún trastorno mental son escasas. Además, la DG se suele presentar con trastornos de ansiedad, y la FS con trastornos depresivos. Este estudio es uno de los primeros en examinar las diferencias entre el bienestar en individuos con un diagnóstico clínico de DG o FS, comparados con individuos sin dicho diagnóstico y en comprobar las diferencias de bienestar dentro de cada categoría de diagnóstico en realación a individuos con y sin comorbilidad. Método: Participaron 119 individuos con un diagnóstico de DG, con base en la SCID, 47 con FS y 118 controles. Resultados: Los resultados revelaron que el bienestar general, así como el bienestar emocional, psicológico y social eran inferiores en el grupo de DG y FS en comparación con el grupo control. Los individuos con comorbilidad informaron un menor bienestar que los individuos sin comorbilidad. Conclusiones: Estos resultados tienen repercusión clínica, pues la presencia de la comorbilidad puede requerir un acercamiento terapéutico diferente al de un único trastorno.
Major depressive disorders (MDD) and Social Phobia (SP) are among the most frequent mental disorders (Kessler, Chiu, Demler, & Walters, 2005) affecting a substantial number of individuals every year and with ranges between 17.2-19 million for MDD and 5.4-9.3 million for SP in Europe (Wittchen et al., 2011). Both MDD and SP are associated with high drop out rates in the labor market and economic costs ( Banerjee, Chatterji, & Lahiri, 2014; Chiu, Lebenbaum, Cheng, Oliveira, & Kurdyak, 2017; Jia & Lubetkin, 2017; Wittchen et al., 2011). Further, MDD and SP are related to a high burden by impairments in social role performance, and disturbed relationships (Richards et al., 2016; Wittchen, Nelson, & Lachner, 1998).
Comorbidity between mood and anxiety disorders is common (Beesdo et al., 2007; Jacobi et al., 2004; Kessler et al., 2005). Among individuals with MDD, 57.5% also meet criteria for at least one other 12-month anxiety disorder (Kessler, Merikangas, & Wang, 2007). Similarly, among individuals with SP 14.9% meet lifetime criteria for MDD (Kessler, Stang, Wittchen, Stein, & Walters, 1999) and 60% of individuals in treatment for SP meet criteria for depression (Merikangas & Angst, 1995). The combination of high prevalence, comorbidity and impairment make MDD and SP important disorders from a public health perspective. Research has shown that individual and economic difficulties are even more pronounced in individuals with comorbid depression and anxiety disorders (Beesdo et al., 2007; Cavicchioli et al., 2018; Kessler et al., 2003). Furthermore, the presence of comorbidity is associated with higher severity, mortality and longer duration of symptoms (Abreu et al., 2018; Kessler et al., 2005; Meier et al., 2016), and higher risk for treatment resistance (Rizvi et al., 2014).
Given the high impact of depressive and anxiety disorders on everyday life, many individuals seek professional help (Boerema et al., 2016; Johansson, Carlbring, Heedman, Paxling, & Andersson, 2013; Magaard, Seeralan, Schulz, & Brütt, 2017). However, efforts to treat MDD and SP tend to aim to reduce specific symptoms (Lorenzo-Luaces, Keefe, & DeRubeis, 2016), thereby assuming that well-being will increase as well. Interestingly, there is accumulating evidence showing that the absence of mental disorders or symptoms are only moderately related to the presence of well-being (Lamers, Westerhof, Glas, & Bohlmeijer, 2015; Trompetter, Lamers, Westerhof, Fledderus, & Bohlmeijer, 2017). This relation has been formulated in a two-continua model that states that although they are related, “mental health and mental illness are not opposite ends of a single continuum” (Keyes, 2005, p. 546). According to that model (Keyes, 2005), well-being includes emotional well-being, psychological well-being and social well-being. Emotional well-being refers to feelings of pleasure and happiness including life satisfaction. Psychological well-being refers to feelings of self-acceptance, environmental mastery and positive relations to others. Social Well-Being refers to feelings of social contribution, integration and acceptance. The model implies that an individual experiencing many symptoms of psychopathology is more likely to experiencing low well-being. However, this association is only moderate. Thus, an individual may be suffering from mental illness and still experience well-being at the same time (Keyes, 2005). To date, there is no research yet that examined the implications of the two-continua model in terms of differences in well-being in adults with and without MDD and SP.
In the light of the high depression-anxiety comorbidity and its clinical implications, it is important to understand whether comorbidity renders further reduction in well-being. The gained knowledge may help to improve current interventions. Perhaps, in clinical practice well-being should be addressed more in individuals with comorbidity. As for the depression-anxiety comorbidity, research to date is mainly on quality of life (Rapaport, Clary, Fayyad, & Endicott, 2005; Zhou et al., 2017) and there is little research comparing quality of life in individuals with depression-anxiety comorbidity to individuals with no comorbidity (Johansson et al., 2013; Norberg, Diefenbach, & Tolin, 2008). These studies consistently showed lower quality of life in individuals with depression-anxiety comorbidity when compared to individuals without comorbidity. For instance, individuals with anxiety-depressive comorbidity had lower health related quality of life than those with no comorbidity (Riihimäki et al., 2016). Another study showed that anxiety-depressive comorbidity was associated with lower overall quality of life compared to the comparative community sample (Rapaport et al., 2005). To date, no study has examined comorbidity in respect to well-being in individuals with MDD and SP.
This study aimed to address this gap in research while building on the relevance of well-being (Keyes, 2002) and examines differences in well-being in individuals with a primary MDD or SP diagnosis compared to controls as well as in individuals with a comorbid anxiety or depressive disorders. We hypothesized that (1a) individuals with MDD report lower well-being than controls, (1b) Individuals with SP report lower well-being than controls, and that (2) Individuals with comorbidity within the combined diagnostic categories report lower well-being than individuals without comorbidity.
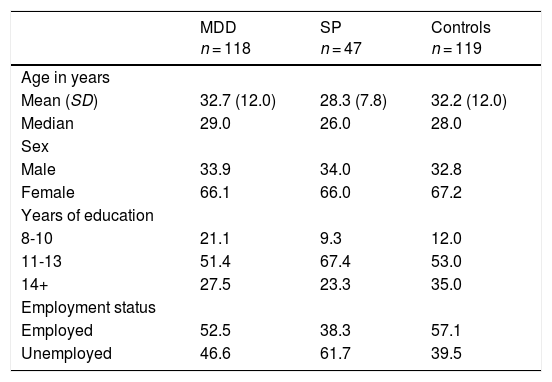
MethodParticipantsParticipants were recruited from March 2014 to August 2016 through leaflets, Internet advertisements, and through three (university) clinics in Germany and Switzerland (Gloster, Miché et al., 2017) as well as private practices in Switzerland. Participants consisted of n = 118 with primary DSM-IV MDD, n = 47 with primary DSM-IV SP, and n = 119 with neither MDD nor SP (controls). For the purpose of comparisons across participant groups, the clinical groups were subdivided on the basis of presence of current comorbidity: MDD (n = 74 with comorbid anxiety disorders; n = 44 without comorbid anxiety disorder) and SP (n = 9 with comorbid depressive disorders and n = 38 without comorbid depressive disorder). Comorbid anxiety disorders included Social Phobia, Specific Phobias, and Panic disorder with or without agoraphobia, and Generalized Anxiety Disorder. Comorbid depressive disorders included MDD and Dysthymic Disorder. Individuals in the MDD group could present multiple anxiety comorbidities, and individuals in the SP group could present multiple depressive comorbidities. Current primary diagnoses (i.e. last four weeks) were determined with the Structured Clinical Interview for DSM- IV Axis I Disorders (SCID; Wittchen, Wunderlich, Gruschwitz, & Zaudig, 1997). All comorbid diagnoses refer to the past month (e.g. Social Phobia, Specific Phobias, and Panic disorder with or without agoraphobia), except for Generalized Anxiety Disorder that refers to the last six months and Dysthymic Disorder that refers to the last two years. Demographic information can be seen in Table 1.
Demographic information of sample and sample characteristics.
| MDD n = 118 | SP n = 47 | Controls n = 119 | |
|---|---|---|---|
| Age in years | |||
| Mean (SD) | 32.7 (12.0) | 28.3 (7.8) | 32.2 (12.0) |
| Median | 29.0 | 26.0 | 28.0 |
| Sex | |||
| Male | 33.9 | 34.0 | 32.8 |
| Female | 66.1 | 66.0 | 67.2 |
| Years of education | |||
| 8-10 | 21.1 | 9.3 | 12.0 |
| 11-13 | 51.4 | 67.4 | 53.0 |
| 14+ | 27.5 | 23.3 | 35.0 |
| Employment status | |||
| Employed | 52.5 | 38.3 | 57.1 |
| Unemployed | 46.6 | 61.7 | 39.5 |
This study used a subset of a quasi-experimental, intensive, longitudinal study with diagnostic status of group as the quasi-experimental factor examining symptom fluctuations and memories thereof by means of event sampling methodology (for details see Gloster, Klotsche et al., 2017). Trained psychology graduate and doctoral students collected the data. For the present study, data from the baseline assessment of participants in the MDD, SP and control group were used. The study team rated diagnoses on the Clinical Rating Scale (adapted: Unnewehr, Schneider, & Margraf, 1995), in which the highest rating corresponded to the primary diagnosis. Participants across the three groups were matched by age and sex. Further inclusion criteria were age between 18-65 years and the ability to understand German. Exclusion criteria were active current suicidal intent and substance dependence. All procedures were approved by the local ethics committee.
MeasuresStructured Clinical Interview for DSM- IV Axis I Disorders (SCID; Wittchen et al., 1997). Diagnoses of mental disorders were assessed with the Structured Clinical Interview for DSM- IV Axis I Disorders (SCID; Wittchen et al., 1997). The SCID is a semistructured interview for clinicians and trained researchers for making DSM- IV Axis I diagnoses. The interview is separated into different sections corresponding categories of diagnoses. Sections begin with an entry question that allow the interviewer to skip the associated questions if the entry conditions are not met. Symptoms are coded as present, or absent. Studies on the psychometric properties of the SCID indicated good reliabilities (Skre, Onstad, Torgersen, & Kringlen, 1991; Williams et al., 1992). Inter-rater agreement has been reported to be between .72 was SP and .93 for MDD (Skre et al., 1991).
Mental Health Continuum-Short Form (MHC-SF; Keyes, 2005)
The MHC-SF (Keyes, 2005) is a 14-item questionnaire that measures well-being on a scale from 1 (never) to 6 (every day), whereas the emotional well-being (3 items), social well-being (5 items) and psychological well-being (6 items) in the last month was captured. For each aspect of well-being a mean score across the respective items was calculated. Higher scores indicate greater emotional, social and psychological well-being (Keyes, 2005; Lamers, Westerhof, Bohlmeijer, Klooster, & Keyes, 2011). The MHC-SF has presented good psychometric properties across various age groups and countries (Cronbach's α = .74-.89; Lamers, Westerhof, Bohlmeijer, Klooster, & Keyes, 2011; Westerhof & Keyes, 2010).
Statistical analysisData were analyzed using Statistical Package for the Social Sciences (SPSS) version 22.0. Prior to analysis data was tested for normality and outliers. Our hypotheses that individuals with a diagnosis report lower well-being than controls (hypothesis 1a and 1b), and that individuals with comorbidity within the combined diagnostic categories report lower well-being than individuals without comorbidity (hypothesis 2) were tested by means of a general linear model with orthogonal contrasts. The two a priori defined contrasts were a) control group versus MDD or SP groups, and b) comorbidity versus no comorbidity within the combined MDD and SP groups. We controlled for the recruitment location. The α level for statistical significance for all analyses was set to .05. Between-group effect sizes were calculated according to Cohen's d. Effect sizes of 0.2, 0.5, and 0.8 refer to small, moderate, and large effects, respectively (Cohen, 1988).
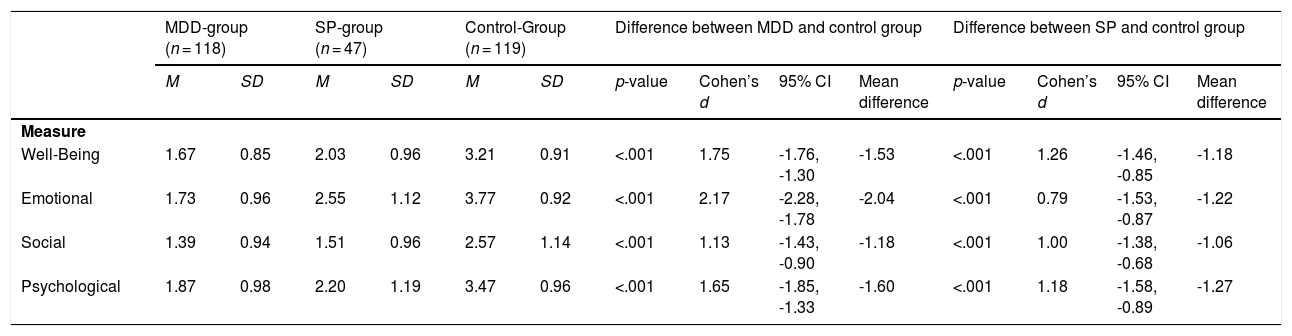
ResultsDescriptive statisticsDescriptive statistics of all measures involved in the analyses are shown on the left-hand side of Table 2.
Descriptive Measures of all outcome measures and results of group comparisons.
| MDD-group (n = 118) | SP-group (n = 47) | Control-Group (n = 119) | Difference between MDD and control group | Difference between SP and control group | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | p-value | Cohen’s d | 95% CI | Mean difference | p-value | Cohen’s d | 95% CI | Mean difference | |
| Measure | ||||||||||||||
| Well-Being | 1.67 | 0.85 | 2.03 | 0.96 | 3.21 | 0.91 | <.001 | 1.75 | -1.76, -1.30 | -1.53 | <.001 | 1.26 | -1.46, -0.85 | -1.18 |
| Emotional | 1.73 | 0.96 | 2.55 | 1.12 | 3.77 | 0.92 | <.001 | 2.17 | -2.28, -1.78 | -2.04 | <.001 | 0.79 | -1.53, -0.87 | -1.22 |
| Social | 1.39 | 0.94 | 1.51 | 0.96 | 2.57 | 1.14 | <.001 | 1.13 | -1.43, -0.90 | -1.18 | <.001 | 1.00 | -1.38, -0.68 | -1.06 |
| Psychological | 1.87 | 0.98 | 2.20 | 1.19 | 3.47 | 0.96 | <.001 | 1.65 | -1.85, -1.33 | -1.60 | <.001 | 1.18 | -1.58, -0.89 | -1.27 |
Note. CI = Confidence Interval; MDD = Major Depressive Disorder; SP = Social Phobia; Mean differences refer to the difference between the respective clinical group and the control group.
Overall well-being as well as emotional, social and psychological well-being were all significantly lower in individuals with MDD compared to the control participants, with large effect sizes throughout (Table 2).
Individuals with a SP report lower well-being than controls (Hypothesis 1b)Likewise, individuals with SP endorsed in significantly lower overall well-being, emotional, social and psychological well-being compared to the control group, with large effect sizes, respectively (Table 2).
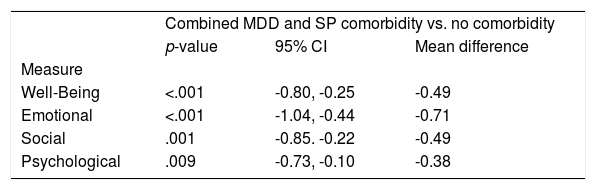
Individuals with comorbidity within the combined diagnostic categories report lower well-being than individuals without comorbidity (Hypothesis 2)Significant differences were found among individuals with and without comorbidity within the combined diagnostic categories (i.e. MDD and SP) in overall, as well as emotional, social and psychological well-being (Table 3). Thus, individuals with comorbidity reported lower overall, as well as emotional, social and psychological well-being.
Descriptive measures of clinical groups with and without anxiety-depressive comorbidity and results of group comparison.
| Combined MDD and SP comorbidity vs. no comorbidity | |||
| p-value | 95% CI | Mean difference | |
| Measure | |||
| Well-Being | <.001 | -0.80, -0.25 | -0.49 |
| Emotional | <.001 | -1.04, -0.44 | -0.71 |
| Social | .001 | -0.85. -0.22 | -0.49 |
| Psychological | .009 | -0.73, -0.10 | -0.38 |
Note. CI = Confidence Interval; MDD = Major Depressive Disorder; SP = Social Phobia. Mean differences refer to the difference between the respective clinical group and the control group.
The aim of this study was to investigate differences in well-being in individuals with a diagnosis of MDD or SP and in individuals with comorbidity within the combined diagnostic groups, respectively. To the best of our knowledge, this is the first study to examine differences in individuals with MDD or SP in well-being with an explicit control group. As hypothesized, we found that individuals with a diagnosis showed lower well-being compared to controls. This finding supports previous literature reporting low to medium ranges in quality of life in individuals with MDD and SP (Rapaport et al., 2005). A previous study compared well-being to a community norm (Rapaport et al., 2005), however, we are unaware of any studies that tested these patterns of well-being against an control group matched for age and sex. While previous studies used quality of life as outcome measures to examine differences in individuals with a clinical diagnosis compared to those without a clinical diagnosis (Johansson et al., 2013; Norberg et al., 2008), we used an explicit measure of well-being. In contrast to quality-of-life measures, the well-being measure applied in the present study incorporates the presence of emotional, social and psychological well-being and thus is taking different aspects of well-being into account. Importantly, this concept of well-being can be directly linked to the definition of well-being of the World Health Organization, WHO (2004), which states that well-being is present when “the individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to his or her community” (World Health Organization, WHO, 2004). Furthermore, it is known that individuals with MDD and SP experience lower positive affect, emotions and evaluate events as less pleasant and more stressful compared to individuals without MDD and SP (Blanco & Joormann, 2018; Dunkley et al., 2017), factors that likely contribute to a generally lower well-being in individuals with MDD and SP. The association of well-being and depression is further interlinked with age in that younger adults experience higher symptoms of depression (Schönfeld, Brailovskaia, & Margraf, 2017). Moreover, individuals with MDD and SP are clearly limited in daily activities (e.g. missed work days, throwbacks at work) in comparison to individuals without MDD and SP (e.g. Broadhead, Blazer, George, & Tse, 1990).
As hypothesized, individuals with comorbidity reported lower well-being than individuals with no anxiety-depressive comorbidity. Although there is research in the field of quality of life, a construct that is sharing similarities with well-being, there is no research so far in terms of differences in well-being in adults with and without anxiety-depressive comorbidities. Our findings are consistent with those studies reporting lower quality of life (Cavicchioli et al., 2018; Norberg et al., 2008; Zhou et al., 2017) in individuals with comorbid disorders, perhaps due to the higher symptom burden, compared to individuals no comorbidity. For instance, a study examining associations of anxiety-depression comorbidity and quality of life found that comorbidity to depression in anxiety disorders is linked to lower quality of life (Norberg et al., 2008). We extended their findings by including a depression diagnosis group, showing that depression was associated with low well-being ratings already. Likewise, a study investigating comorbidity in anxiety disorders indicated that well-being decreased as individuals moved from having one disorder to having multiple disorders (Sherbourne et al., 2010). This indicates that clinicians should be aware for patients presenting depression-anxiety comorbidity and that there is greater burden on those with comorbidity. The presence of comorbidity may require a different therapeutic approach than with single disorders. Indeed, there is evidence that acceptance- and mindfulness-based interventions are linked to improved outcomes for patients with comorbidity, and traditional Cognitive-Behavioral Therapy (CBT) more helpful for single disorders (Arch & Ayers, 2013). This is in line with previous research, e.g. a switching trial from CBT to Acceptance and Commitment Therapy (ACT) in treatment-resistant patients, that presented a high comorbidity rate (Gloster et al., 2015; Gloster, Klotsche et al., 2017).
Furthermore, we observed a descriptive pattern in well-being in that individuals in the control group reported the highest well-being, followed by individuals with SP without comorbidity and ultimately individuals with MDD without comorbidity. This pattern corresponds to one found in earlier studies (Rapaport et al., 2005; Riihimäki et al., 2016), which found that impairments in quality of life were higher in individuals with MDD than in individuals with SP. This suggests that SP may have a rather specific impact on well-being in individuals’ lives, while MDD may have a more general and overarching impact on peoples’ lives.
This study needs to be interpreted in the light of several limitations. First, we relied on self-reported measurements to assess well-being. These are prone to biases inherent in this assessment approach. Additional analyses of information stemming from other sources (e.g., friends and family or employers) may have resulted in different overall findings as self-report measures may not capture well-being in their full complexity. Second, the study sample is limited to participants with and without MDD and SP. This and because of the potential effects of self-selection and treatment, the results may raise the question of generalizability. Third, we had no data on the long-term and chronic course of the two clinical disorders. Thus findings cannot be generalized to individuals with chronic depression and their association to well-being.
With these limitations in mind, the current study extended the existing body of literature by explicitly investigating differences in well-being in individuals with and without MDD or SP, as well as in the subgroups of MDD or SP with and without comorbidity to anxiety disorders or to depressive disorders. Also, this is the first study examining the implications of the 2-continua model in terms of well-being in adults with and without MDD and SP. Future studies should, for instance, investigate the role of well-being in different samples other than depressive or anxiety disorders to determine whether results are not limited to these particular clinical groups. It may also be helpful to incorporate well-being measures in addition to treatment outcome assessments to evaluate treatment outcomes in an additional informative way and to augment symptom-based treatment change analyses. Moreover, studies should clarify the temporal relationship of a clinical diagnosis of MDD or SP and low well-being. This is important as well-being are both diminished in individuals with a clinical diagnosis and evaluating (temporal) pathways may allow to intervene with targeted psychological help.
Our findings not only suggest that individuals with a clinical diagnosis (i.e. MDD or SP) clearly differed from individuals with no clinical diagnosis of MDD or SAD (i.e. controls) in respect to well-being, but also that individuals with comorbidity within both diagnostic categories engage in lower well-being than those without comorbidity. Thus, our findings are of clinical importance and may indicate the need to enhance well-being (Keyes, 2007) in individuals with a clinical diagnosis. One intervention that promotes well-being is ACT (Ciarrochi & Kashdan, 2013).