This study aimed to analyze the effects of psychological treatments on quality of life among cancer patients and survivors. Additionally, it was explored the moderating influence of some medical- and treatment-related features on these effects. Scientific studies published between 1970 and 2012 were analyzed. Seventy-eight studies were included in a meta-analysis. Concerns related to samples, interventions, and standard of methodological evidence were explored across the studies. A significant overall effect size of psychological interventions was revealed (g=.35). Clinical state and use of adjuvant psychological treatment for managing medical side effects moderated this result (p<.05). Furthermore, a meta-regression model was showed significant (R2=.30) so as to explain the quality of life change associated with psychological interventions. The psychotherapeutic benefits on depressive symptomatology were included as a moderating factor. To sum up, quality of life is improved by psychological interventions, especially when patients have to cope with medical treatment or with adjustment after the disease is treated. Psychological treatments tend to promote better outcomes when depressive symptomatology is managed. These findings support that providing psychological treatments should be considered as crucial for the patient's health in cancer contexts.
Este estudio pretende conocer el efecto de los tratamientos psicológicos sobre la calidad de vida de pacientes y supervivientes de cáncer, así como la influencia moderadora de variables médicas y propias del tratamiento sobre dicho efecto. Para ello, se realizó un meta-análisis que incluyó 78 trabajos publicados entre 1970 y 2012. Se analizaron aspectos relacionados con la muestra, el tratamiento y la calidad metodológica de estos estudios. Como resultado, se encontró un tamaño del efecto significativo de los tratamientos psicológicos sobre la calidad de vida (g=0,35). Dicho efecto estaba moderado por el estado clínico del paciente y la adyuvancia del tratamiento psicológico con el médico (p<0,05). También se observó que mayores reducciones de sintomatología depresiva debidas al tratamiento llevaban a mayores beneficios sobre la calidad de vida según las meta-regresiones ejecutadas (R2=0,30). En conclusión, los tratamientos psicológicos pueden mejorar la calidad de vida de pacientes oncológicos, principalmente cuando deben afrontar tratamientos médicos, así como de los supervivientes. Además, cuando se reduce la sintomatología depresiva la calidad de vida suele mejorar. Estos resultados destacan la influencia decisiva de los tratamientos psicológicos para la salud integral en contextos oncológicos.
Quality of life (QoL) refers to a whole, integrated state of physical, mental and socioemotional well-being. This multidimensional construct is eminently subjective and may be measured through varying indicators, such as health status or personal functioning (Ferguson & Cull, 1991; World Health Organization, WHO, 1948). QoL entails more than a mere absence of disease, although it is profoundly associated with its severity (Amedro et al., 2014; Hogg, Peach, Price, Thompson, & Hinchliffe, 2012; Pagels, Söderkvist, Medin, Hylander, & Heiwe, 2012). For cancer patients, QoL is a crucial concern both when cancer is present and when the disease has been treated (Cheng et al., 2012; Costa-Requena, Rodríguez, & Fernández-Ortega, 2013). Oncologic medical treatments lead to QoL improvements, but sometimes a wide variety of side effects can arise and bring about significant health-related complaints (Decat, de Araujo, & Stiles, 2011; Gogou et al., 2015; Goh, Steele, Jones, & Munro, 2013). Likewise, when cancer is treated, patients show higher levels of QoL, but physical and psychological sequelae often diminish it (Bardwell & Fiorentino, 2012; Duijts et al., 2014; Howard-Anderson, Ganz, Bower, & Stanton, 2012).
Facing a cancer or its sequelae may lead to significant psychological distress and psychiatric symptomatology, such as sleep difficulty, excessive worries regarding survival and depressive mood. These symptoms are often associated with lower QoL and well-being (Bornbaum et al., 2012; Oh, Seo, Jeong, & Seo, 2012). A wide range of psychological interventions may be applied to ameliorate the psychological distress and the adjustment to being a cancer patient, subsequently enhancing QoL (Badr & Krebs, 2013; Preyde & Synnott, 2009). Rehse and Pukrop (2003) conducted a meta-analytic review in order to study the overall effect of psychological treatments throughout the cancer recovery process. They found a medium overall effect size (d=.65), though treatment length showed a significant moderating effect.
More recently, another meta-analysis was conducted with similar purposes. Faller et al. (2013) studied the effect of psychological treatments on emotional distress and QoL. In this case, psychological treatments were observed to yield a small overall effect size for QoL (d=.26). Moreover, type of treatment was found to be a significant modulating factor regarding this effect, pointing to healthier outcomes when relaxation programs were applied, for instance. These results differed from those found in the prior meta-analysis, probably due to the differences in sample selection criteria for both studies; as well as the different conceptualizations of QoL and psychological treatment.
Because of these discrepancies, this study aimed to analyze the overall effect size of psychological treatments on QoL in cancer patients and survivors. It thereby considered following the methodology proposed by Rehse and Pukrop (2003) for this purpose; however, QoL was studied from a multidimensional point of view. Furthermore, this study aimed to test whether effect sizes should be considered regarding disease-based features, treatment-related considerations, or methodology-related variables. Finally, the presence of significant models to explain QoL effects of these treatments in relation to medical-related concerns, and psychopathology was studied.
MethodsStudy selection criteriaThis meta-analysis is reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses for Protocols 2015 (PRISMA-P 2015) statement (Moher et al., 2015) and Botella and Gambara (2006) recommendations. Eligibility criteria for studies are detailed according to the PICOS framework as follows.
Participants. Studies with samples composed of adults who suffer from malignant tumors or cancer survivors were selected. Studies that included patients suffering from a benign tumor were ruled out.
Interventions. Studies focusing on analyzing the effect of a psychological intervention on QoL were included. Psychological intervention was defined as nonpharmacologic intervention using psychological procedures: psycho-education, coping skills training, counselling, relaxation, alone or in combination, and psychotherapy (see Hodges et al., 2011). These interventions are applied in order to improve either mental or health-related outcomes. Studies with non psychological interventions, such as physiotherapy, physical training or others were excluded.
Controls. Studies that compared the effect of a psychological treatment with a control group (either a placebo group or a wait-list group) were selected.
Outcomes. Primary outcome was quality of life (measured by self-reports), conceptualized from a multidimensional point of view (WHO, 1948); namely, perceived state of well-being as a whole, including physical, mental and socioemotional aspects. This outcome can be measured through direct indicators (health status and well-being) as well as more indirect ones (patient's functioning tests). Secondarily, other self-reported outcomes were considered: anxiety (measured mainly by using BAI, HADS, STAI), depression (BDI, CES-D, HADS as most used instruments), and fatigue (FSI, MFI, a subscale of FACT-F, as most commonly used instruments).
Studies. Randomized controlled trials published between 1970 and 2012 in scientific press (written in English and Spanish languages) were selected. Papers that did not give enough data to extract the required effect sizes were ruled out.
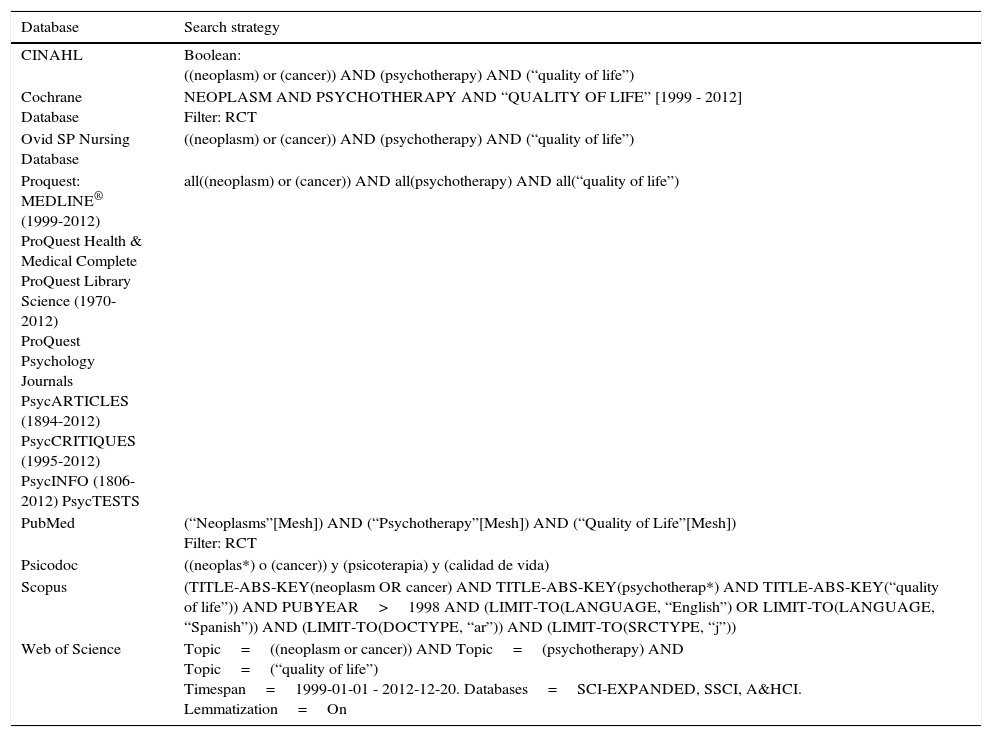
Study selection procedureStudies were selected by reviewing the meta-analysis of Rehse and Pukrop (to select articles between 1970-1999) and four issue-related ones (Badr & Krebs, 2013; Faller et al., 2013; Osborn, Demoncada, & Feuerstein, 2006; Preyde & Synnott, 2009). Additionally, it was conducted some database searches (March, 2013). As key terms, ‘neoplasm(s)’, ‘psychotherapy’, and ‘quality of life’ were considered; as was the reference study (Rehse & Pukrop, 2003). Search queries are attached in Table 1.
Search strategy adaptations for each database.
| Database | Search strategy |
|---|---|
| CINAHL | Boolean: ((neoplasm) or (cancer)) AND (psychotherapy) AND (“quality of life”) |
| Cochrane Database | NEOPLASM AND PSYCHOTHERAPY AND “QUALITY OF LIFE” [1999 - 2012] Filter: RCT |
| Ovid SP Nursing Database | ((neoplasm) or (cancer)) AND (psychotherapy) AND (“quality of life”) |
| Proquest: MEDLINE® (1999-2012) ProQuest Health & Medical Complete ProQuest Library Science (1970-2012) ProQuest Psychology Journals PsycARTICLES (1894-2012) PsycCRITIQUES (1995-2012) PsycINFO (1806-2012) PsycTESTS | all((neoplasm) or (cancer)) AND all(psychotherapy) AND all(“quality of life”) |
| PubMed | (“Neoplasms”[Mesh]) AND (“Psychotherapy”[Mesh]) AND (“Quality of Life”[Mesh]) Filter: RCT |
| Psicodoc | ((neoplas*) o (cancer)) y (psicoterapia) y (calidad de vida) |
| Scopus | (TITLE-ABS-KEY(neoplasm OR cancer) AND TITLE-ABS-KEY(psychotherap*) AND TITLE-ABS-KEY(“quality of life”)) AND PUBYEAR>1998 AND (LIMIT-TO(LANGUAGE, “English”) OR LIMIT-TO(LANGUAGE, “Spanish”)) AND (LIMIT-TO(DOCTYPE, “ar”)) AND (LIMIT-TO(SRCTYPE, “j”)) |
| Web of Science | Topic=((neoplasm or cancer)) AND Topic=(psychotherapy) AND Topic=(“quality of life”) Timespan=1999-01-01 - 2012-12-20. Databases=SCI-EXPANDED, SSCI, A&HCI. Lemmatization=On |
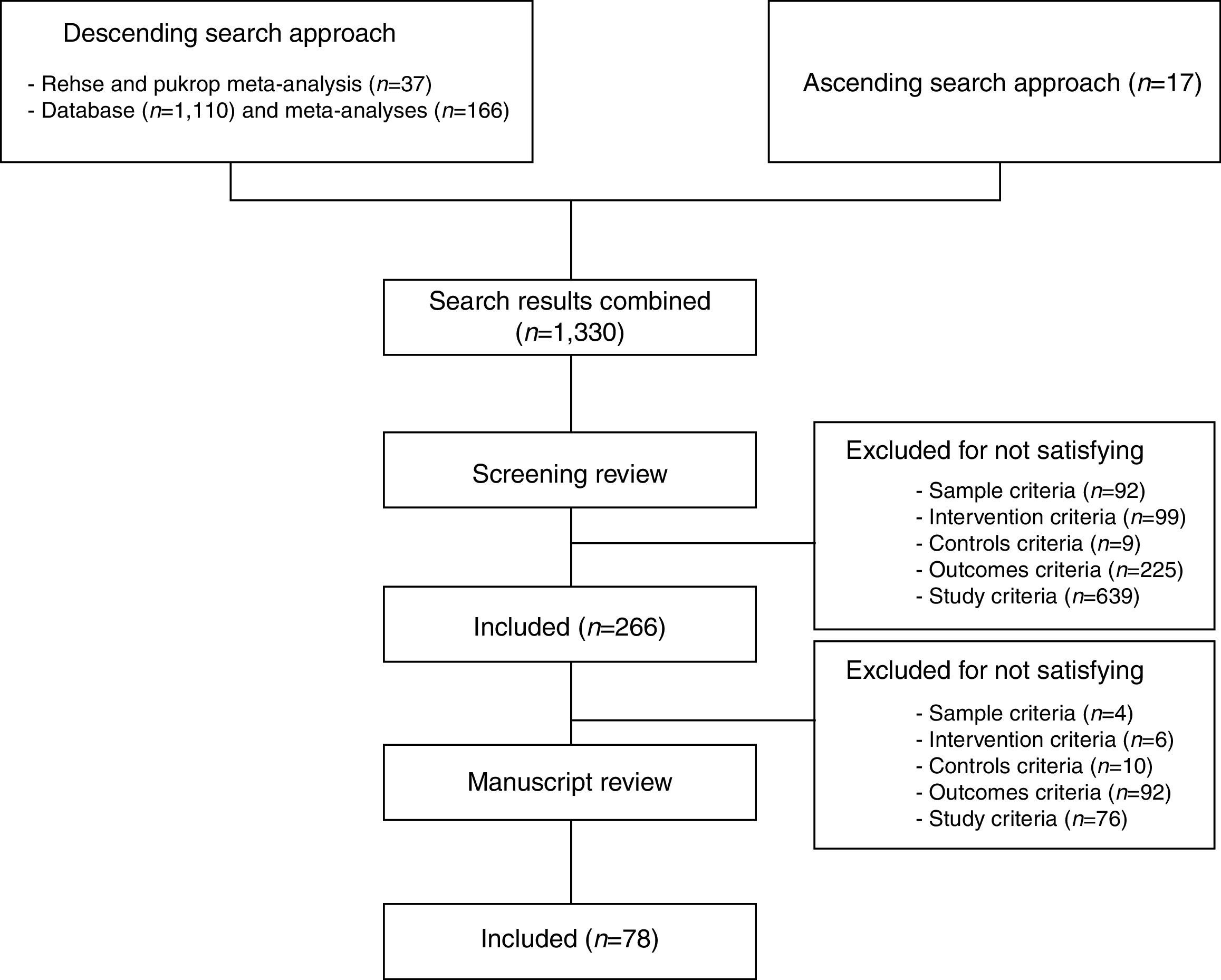
Each study was selected when two reviewers independently considered it satisfied the selection criteria. Thus, papers were screened through an initial review of title, abstract, and keywords. Afterwards, the pre-selected manuscripts were read fully to endorse the selection criteria were satisfied. Meanwhile, a descendent search process was performed: all the articles cited in selected manuscripts were reviewed.
Outcome domains and coded variablesRelevant data of the studies were extracted and coded using a database developed for these purposes by a reviewer. Furthermore, the other one tested coding tools by reading and categorizing a random selection of the study sample. This selection encompassed 25% of the total sample. As a result, 80% of the relevant data were equally coded by the two reviewers, χ2 (1)=63.00, p<.01. Disagreements were resolved by discussion.
As a dependent variable, the effect size, extracted by comparing QoL scores between experimental and control group after psychological treatment was applied, was calculated. Data were collected by validated instruments that assessed QoL from concepts such as integrated sense of well-being, as well as integrated perception of health and functioning. Most used instruments are stated in Ferguson and Cull (1991).
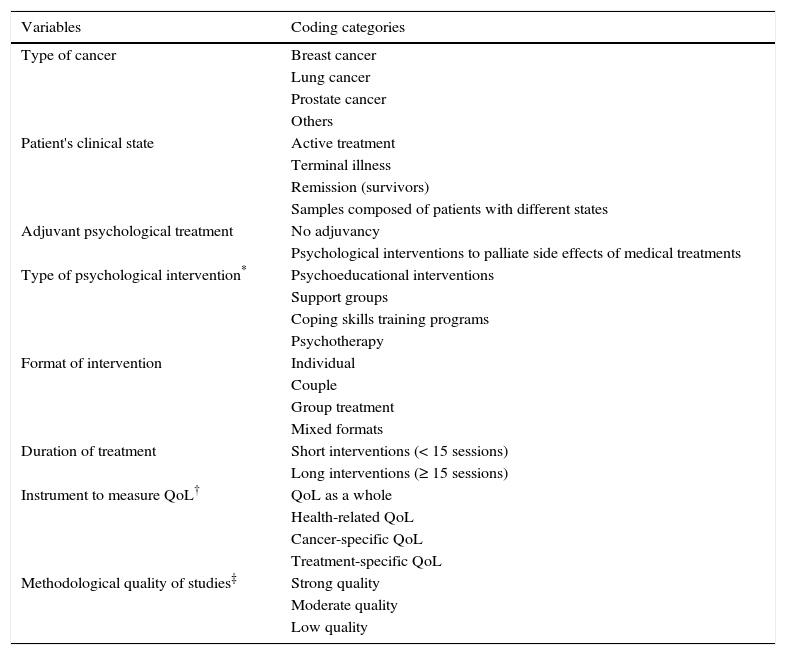
Eight categorical factors were considered in this meta-analysis (see Table 2). Additionally, several quantitative moderating factors were studied: the mean age of participants, gender-related proportions within samples and clinical symptomatology (levels of depression, anxiety, and cancer-related fatigue).
Categorical variables considered in this meta-analysis.
| Variables | Coding categories |
|---|---|
| Type of cancer | Breast cancer |
| Lung cancer | |
| Prostate cancer | |
| Others | |
| Patient's clinical state | Active treatment |
| Terminal illness | |
| Remission (survivors) | |
| Samples composed of patients with different states | |
| Adjuvant psychological treatment | No adjuvancy |
| Psychological interventions to palliate side effects of medical treatments | |
| Type of psychological intervention* | Psychoeducational interventions |
| Support groups | |
| Coping skills training programs | |
| Psychotherapy | |
| Format of intervention | Individual |
| Couple | |
| Group treatment | |
| Mixed formats | |
| Duration of treatment | Short interventions (< 15 sessions) |
| Long interventions (≥ 15 sessions) | |
| Instrument to measure QoL† | QoL as a whole |
| Health-related QoL | |
| Cancer-specific QoL | |
| Treatment-specific QoL | |
| Methodological quality of studies‡ | Strong quality |
| Moderate quality | |
| Low quality |
Note.
Classified according to Cunningham (1995), although spiritual/existential therapies were considered a branch of psychotherapies.
According to Murphy, Ridner, Wells, and Dietrich (2007). The fourth category was included because there are many instruments adapted for each type of definite oncologic intervention instead of symptom-specific QoL (in this meta-analysis QoL was considered as a multidimensional construct).
Assessed using the Quality Assessment Tool for Quantitative Studies (Thomas, Ciliska, Dobbins, & Micucci, 2004).
A single effect size was calculated for each study, for the dependent variable as well as for the quantitative clinical factors. These calculations were based on the standardized difference of group means after psychological treatment by using the Hedges’ g statistic (Botella & Gambara, 2002; Hedges & Olkin, 1985). The unbiased estimator of g based on gamma function was therefore applied (see Equation 1). Effect sizes were interpreted according to the guidelines by Cohen (1988).
Different rules were used in order to avoid dependency between measures. Firstly, if there was more than one experimental group, the group whose psychological treatment was more common was considered. If there was more than one instrument to measure QoL in a study, only the instrument showing the highest reliability was chosen. Additionally, the overall effect size was calculated. This was weighted by the inverse of variance of the single effect sizes (see Equation 2), which is obtained through the single intra-study variability and an estimate of the between-study variance (Botella & Gambara, 2002).
Afterwards, homogeneity between studies was tested for by using the Qt statistic and the I2 index (Hedges & Olkin, 1985; Higgins & Thompson, 2002). If the null hypothesis was rejected for this test, the presence of explanatory models had to be studied in order to find factors related to these systematic variations.
Explanatory model fitting was therefore considered. We firstly analyzed the magnitude of moderating effects derived from coded categorical factors by means of analogues of analysis of variance (Hedges & Pigott, 2004). Forest plots were attached to complement these analyses visually.
All of these calculations were conducted assuming random effects models (Hedges & Pigott, 2004; Sánchez-Meca, Marín, & Huedo, 2006).
Meanwhile, quantitative model fitting was also tested by means of multiple meta-regression. The factors considered were incorporated into two different models: one comprising sociodemographic and medical related factors (gender, sample age, clinical state, use of adjuvant psychological interventions for managing the side effects of medical treatment, and fatigue); another that involved emotional symptomatology (anxiety and depression). Model estimations were extracted by using maximum likelihood based methods (Botella & Gambara, 2002; Hedges & Pigott, 2004).
Finally, publication bias was assessed by using contour-enhanced funnel plots and the Egger's regression test (see Mavridis & Salanti, 2014).
SPSS v. 19 (script by Lipsey & Wilson, 2001) and R x64 3.0.1 (METAFOR 1.9-1 package) were used to conduct these analyses.
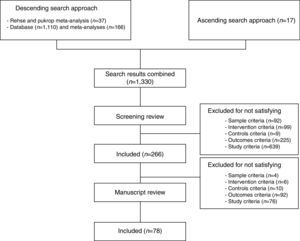
ResultsFigure 1 depicts the steps followed to obtain the study sample. An initial sample of 1330 original papers was reviewed. Upon the study selection stage was over, 78 studies were definitely included in this meta-analysis*. Study reviewers agreed on sample selection. All of these studies were written in the English language. The bulk of studies showed a medium level of methodological quality (60.20% of sample) in contrast with strong and weak levels (24.40% and 15.40%, respectively).
A total of 7,342 individuals composed the studies. Mean age of participants was 54.82 years old (SD=7.36). Regarding the type of oncologic disease, almost half of the studies were focused on samples with breast cancer (46.20% of studies). Moreover, the studies were mainly focused on samples under oncologic medical treatment (82.90% of studies, respectively).
Regarding the use of adjuvant psychological treatment, 14.10% of studies tested the effects of psychological treatment on adverse symptomatology derived from a medical treatment. Regarding the type of psychological treatment, the most common type was psychotherapy (46.80% of studies); while the most common format was individual treatment (54.10% of studies) and short-term ones (76.30% of studies).
Considering how QoL was assessed, more than the half of the studies used instruments that evaluate health-related QoL; fewer studies used instruments that measure generic QoL cancer-specific or treatment-specific QoL (24.40%, 19.20% and 3.80% of studies, respectively).
Instruments used to measure QoL showed adequate levels of reliability, as Cronbach's alpha statistic confirmed (Mdn=.89, range=[.69, .95]), as well as those used to measure depression (Mdn=.82, range=[.70, .91]), anxiety (Mdn=.85, range=[.74, .93]), and cancer-related fatigue (Mdn=.93, range=[.82, .97]).
Distribution of effect sizesSingle effect sizes in relation to the effect of psychological treatment on QoL ranged between -.41 and 2.37 and study variances between .01 and .59. Regarding overall effect size, it was found that g=.35, CI95=(.25, .45), with contrast statistic Zc=7.51; p<.01. The between-study variability was v=.10 among the 78 studies analyzed. These results suggest the presence of a small-to-medium overall effect size of psychological treatments on QoL.
Afterwards, the homogeneity tests revealed a significant heterogeneity between studies, Qt (77)=243.80; p<.01; and I2=68.42%. These findings suggest that differences between single effect sizes were too large to consider being due to random effects.
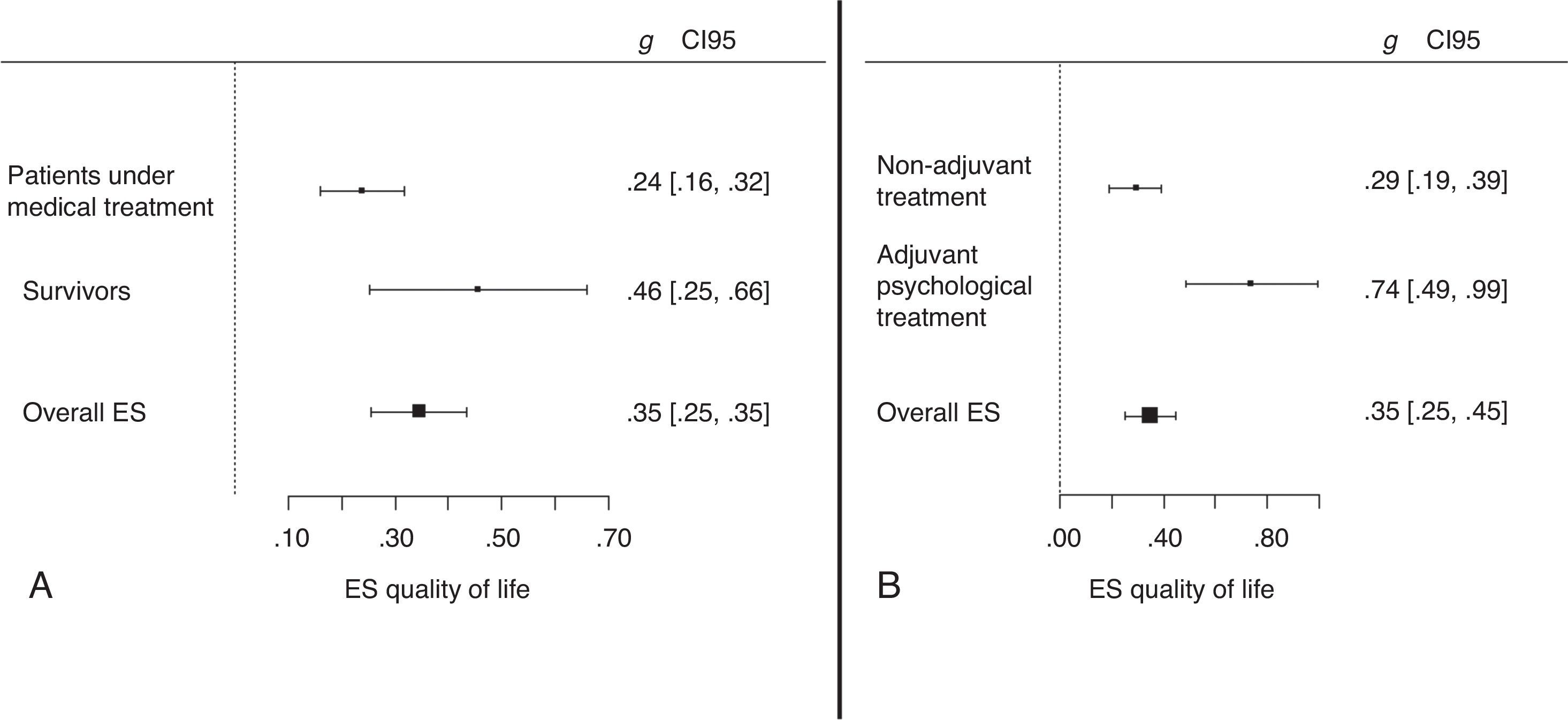
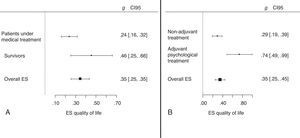
Categorical model fittingCategorical models were tested separately to analyze the influence of each moderating factor on the effect of psychological treatments. As a result, two significant models showed differences between categories. The first model was related to patient's clinical state, with Qb (2)=10.37; p<.01. Although, we reconsidered these analyses in order to clarify the true effect of this moderator. Thus, we discarded the studies with mixed samples and the studies with terminal patients due to the small sample of studies. Hence, clinical state model was recalculated using two categories: survivors (k=9), and cancer patients under medical treatment (k=58). As a result, significant differences were again found between categories, Qb (1)=3.89; p<.05. Figure 2 shows the overall effect sizes of these categories. Thus, a small-to-medium overall effect size was observed in studies which analyzed the effects of psychological treatments on survivors. Studies with people under medical treatment showed a lower effect size.
Overall effect sizes in relation to significant categorical models.
Note. This figure includes overall effect sizes in function of two categorical factors. The Graph A depicts overall effect sizes regarding patient's clinical stage. Likewise, overall effect sizes in function of whether the psychological intervention is applied for reducing the effects of ongoing medical oncologic treatments (adjuvant treatment) or not, are presented in the Graph B.
Overall effect sizes for all categories with confidence interval (between square brackets) are included. ES=Effect size.
Furthermore, significant differences between categories were found regarding the use of adjuvant psychological treatment (see Figure 2), with Qb (1)=10.78; p<.01. Thus, when psychological treatment was applied while a medical treatment was ongoing (k=11), in order to ameliorate the side effects, the overall size effect was greater than when treatment was not applied for these purposes (k=67).
Quantitative model fittingOverall effect size was calculated for the quantitative moderating factors, observing small overall effect sizes for fatigue (g=.21, CI95=[.07, .34]; Zc=2.99, p<.01) and depression (g=.38, CI95=[.21, .54]; Zc=4.45, p<.01); and a medium overall effect size for anxiety (g=.54, CI95=[.33, .76]; Zc=4.88, p<.01).
Afterwards, the meta-regressive models were estimated independently. The model composed of sociodemographic and medical factors was tested first, but a non-significant effect was found for that (p>.05). The model based on emotional factors was then tested. Thus, significant fitting was observed for this model, with QR (2)=15.10; p<.01. This model was calculated from a sample of 32 studies and a considerable explained variance of criterion was found, R2=.30. However, factorial loading for depression, and not anxiety, was revealed as significantly different from zero; with B=.73, CI95=(.35, 1.11); and Zc=3.78; p<.01.
These results highlight the importance of depressive symptomatology ameliorations in order to delimit the yielded effect of psychological treatments on QoL.
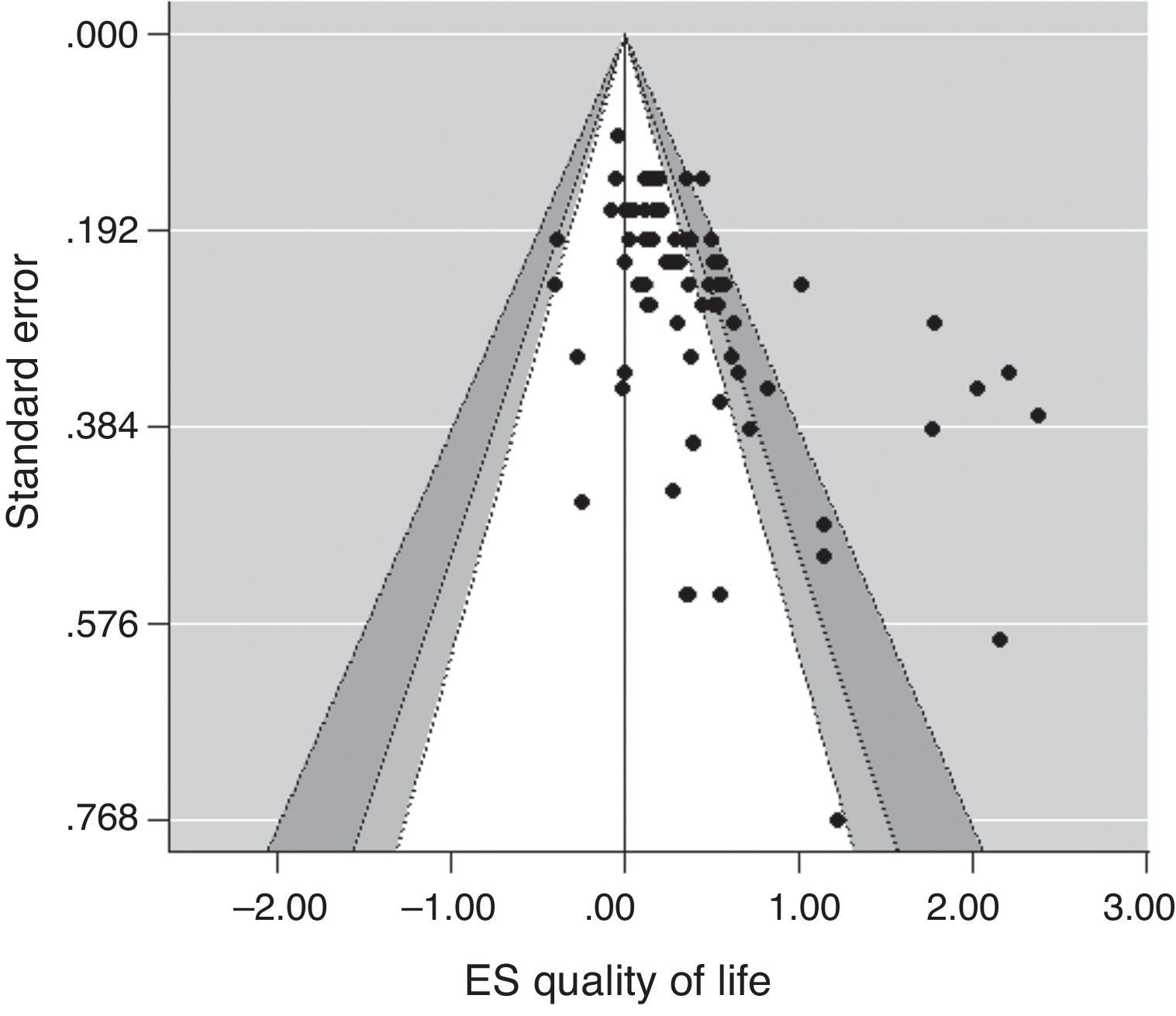
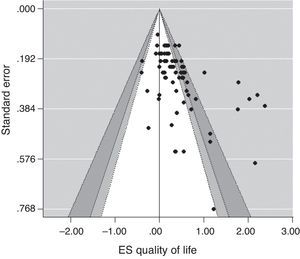
Publication biasA contour-enhanced funnel plot was conducted and explored first (see Figure 3). As a result, it was possible to visualize that a publication bias may affect the results of this meta-analysis, due to the presence of some asymmetry within the graph. Egger's regression test supported this finding, with Z=5.75, p<.05. This result means that significant asymmetry was found, and the results derived from this meta-analysis should be considered cautiously.
DiscussionQuality of life and related constructs become more relevant over time (e.g., see Miret et al., 2015). In fact, QoL is one of the most important concerns for cancer patients and survivors. This state should be considered as multidimensional in order to promote integrative patient-centered care. It is therefore recommended that multidisciplinary approaches are taking within oncologic contexts. Psychological treatments should take part in this context. These enable a better therapeutic management of emotional symptomatology and the promotion of more adaptive coping skills in order to fight against cancer. Consequently, psychological treatments lead to improving the global adjustment to daily environment and increasing the sense of well-being (Andersen et al., 2010; Cordella & Poiani, 2014).
This study aimed to shed light on the true effects of psychological treatments in cancer contexts. Concretely, the effect of these treatments on the QoL of people who suffer from cancer or survivors. Moreover, we studied whether different moderators might influence this outcome.
According to our results, a statistically significant overall effect size of psychological treatments was observed regarding the integrated sense of QoL of cancer patients and survivors. Concretely, a small-to-medium overall effect size was highlighted. This result enables us to suggest that psychological treatments yield significant benefits on QoL in cancer patients. This effect size is smaller than the results found by Rehse and Pukrop (2003); although it tends to agree more with the ones shown in the recent meta-analysis by Faller et al. (2013). These authors showed an even smaller overall effect size than the current study. It is likely that divergences between the results derived from these two meta-analyses and the current one could be related to protocol keeping between the studies. Firstly, it is important to highlight that the current study considers QoL from a multidimensional perspective. Moreover, psychological treatments were conceptualized according to Hodges et al. (2011), and coded following the classification of Cunningham (1995). This classification is focused on patients’ needs and levels of involvement in their recovery process along the disease trajectory (Hopkins & Mumber, 2009). Conversely, Faller et al. (2013) assumed sample selection criteria based only partially on these referenced frameworks (i.e., only face-to-face treatments were considered within the study, ruling out treatments that incorporated other forms of delivery); indeed, they followed another classification of psychological treatments.
On the other hand, the current study and the reference ones agree upon the fact that psychological treatments cannot show a unified effect size. In our meta-analysis, two of the studied variables were revealed as significant moderating factors in this regard. The first one was the patient's clinical state. Thus, it was found that psychological treatments promote greater QoL for survivors. The benefits of psychological treatments seemed to fade away in patients under active treatment. Medical treatments toward the healing may be rather more crucial throughout cancer healing process. Nevertheless, psychological treatments become more effective when patients had to cope with the side effects of ongoing medical treatments, such as surgery, chemotherapy or radiotherapy (Cheung, Molassiotis, & Chang, 2003; Svensk et al., 2009). Hence, the effect of reducing somatic anxiety, sleep problems or other symptomatology which are a consequence of medical treatments is noteworthy. Furthermore, when cancer is treated, psychological treatments can play a more important role, as the results of this meta-analysis highlight. A person who recovers from a cancer has to adapt to daily life in different conditions than before. Thus, survivors tend to show some physical and psychological sequelae, situations of disability and handicap, and important contextual changes (job loss, new familiar roles, etc.). These events taken together impact well-being and QoL and can be coped with more effectively by the aid of psychological treatments (Mann et al., 2012; Osborn et al., 2006).
It also is noteworthy that this study found no significant effects of other moderators. Thus, neither other medical factors nor intervention-related aspects studied showed a significant influence on the psychological-treatment effects on QoL. This fact is not aligned with findings from the aforementioned works (Faller et al., 2013; Rehse & Pukrop, 2003), probably due to different conceptualizations and the incorporation of more recent studies. Regarding other modulating factors, the role of depressive symptomatology ameliorations should be highlighted to address the benefits of psychological treatments within oncologic contexts. In this sense, the psychological treatments that promoted greater reductions in depressive symptomatology yielded greater benefits on QoL. This statement was endorsed by the results derived from the meta-regressive analyses. No other statistically significant loadings were found neither for sociodemographic features of patients, medical factors nor anxiety ameliorations.
These results highlight that psychological treatments which ameliorate depressive symptomatology can promote greater levels of QoL in oncologic contexts. Depression, and its related symptomatology, is considered a risk factor of cancer incidence and progression (Boyd et al., 2012; Currier & Nemeroff, 2014). Hypothalamus-pituitary-adrenal (HPA) dysregulation and immunological alterations are implied in this status (Lutgendorf & Sood, 2011; Sotelo, Musselman, & Nemeroff, 2014; Thornton, Andersen, & Blakely, 2010). Depressive symptomatology therefore impacts defensive immune-mediated responses against cancer. Additionally, tumor expansion is encouraged by HPA-mediated responses that are characteristic of depressive symptomatology. Consequently, decrements of depressive symptomatology may lead to cancer-related adverse effects being buffered and QoL becoming higher (Barrera & Spiegel, 2014; Howren, Christensen, Karnell, & Funk, 2010).
To sum up, this study highlights a significant small-to-medium overall effect size of psychological treatments on QoL, within cancer contexts. This effect should be considered when taking into account medical variables (the patient's clinical state and the application of psychological treatments to palliate side effects of a medical one). Moreover, it recommends that components for reducing depressive symptomatology are incorporated into psychological treatment.
As strengths, this meta-analysis includes a wide amount of studies, encompassing both more classical and more recent ones, keeping well-validated protocols which were used in the reference study. Indeed, robust definitions were considered and a multidimensional perspective to view QoL was followed. These strengths enable us to provide some evidence in order to complement prior prominent findings (Faller et al., 2013; Rehse & Pukrop, 2003). This study therefore suggests that psychological treatments yield significant improvements on QoL, provided that the medical state of patient is taken into account.
As limitations, this meta-analysis could have incorporated other types of studies (i.e., pre-experimental studies) even though these studies had a lower methodological quality. However, in this case, variables related to the absence of experimental controls could have been added and could have stained the actual results of this meta-analysis. On the other hand, other modulating factors could have been considered (i.e., experience of implementers, personality traits of patients, etc.). Future research should incorporate these in order to clarify the true effects of psychological treatments. Finally, the presence of publication bias is pointed out in this study as well as in other related meta-analyses (Faller et al., 2013; Osborn et al., 2006); this involves that these results should be considered cautiously.
This study intends to contribute toward understanding the disease burden of cancer and the importance of psychological interventions, as well as suggesting populations most likely to help. Psychological treatments play a significant role in integrated care within cancer contexts. These treatments help improve mental health and personal well-being throughout the trajectory of the potentially life-threatening cancer experience. Well-being and QoL remain as crucial factors to promote successful adjustment to daily environments after overcoming this disease.