The aim of the study was to examine the factor structure and psychometric properties of the Spanish version of the Mini-Mental Adjustment to Cancer Scale (Mini-MAC) in a large sample of patients with non-metastatic, resected cancer.
MethodsProspective, observational, multicenter study for which 914 patients were recruited from 15 Spanish hospitals. Exploratory and confirmatory factor analyses, validity and reliability analyses were conducted.
ResultsFactor-analytic results indicated a 4-factor structure of the Spanish version of the Mini-MAC. Three subscales have psychometric properties similar to those of Helplessness, Anxious preoccupation, and Cognitive avoidance of the original the Mini-MAC. The Fighting spirit and the Fatalism subscales were combined on the Positive attitude scale. The four factor-derived scale scores exhibited acceptable accuracy for individual measurement purposes, as well as stability over time in test-retest assessments at 6 months. Validity assessments found meaningful relations between the derived scale scores, and Brief Symptom Inventory depression and anxiety scores and Functional Assessment of Chronic Illness Therapy spiritual well-being scores.
ConclusionsThe Spanish version of the Mini-MAC provides reliable and valid measures for patients with non-metastatic, resected cancer, and results corroborate the instrument’s cross-cultural validity.
El objetivo de este estudio fue analizar las propiedades psicométricas de la versión Española del Mini-Mental Adjustment to Cancer Scale (Mini-MAC) en pacientes con cáncer resecado, no metastásico.
MétodoEstudio multicéntrico, prospectivo y observacional con 914 pacientes reclutados en 15 hospitales de España. Se llevaron a cabo análisis factorial exploratorio y confirmatorio, así como análisis de la validez y fiabilidad de las puntuaciones de la escala.
ResultadosLos resultados de los análisis factoriales sugieren que la estructura más apropiada para la versión española del Mini-MAC es la de cuatro factores. Tres subescalas derivadas de esta estructura tienen propiedades psicométricas similares a la escala original: Desesperanza, Preocupación ansiosa y Evitación cognitiva. Las subescalas Espíritu de lucha y Fatalismo se combinaron en la escala Actitud positiva. Las puntuaciones en las cuatro escalas mostraron una fiabilidad aceptable para su utilización en la evaluación individual, así como estabilidad a lo largo del tiempo en evaluaciones test-retest a los seis meses. Se obtuvieron evidencias de validez en forma de relaciones significativas con las escalas de ansiedad y depresión del BSI, y de bienestar espiritual del FACIT.
ConclusionesLa versión Española del Mini-MAC proporciona puntuaciones fiables y válidas para evaluar las estrategias de afrontamiento en pacientes con cáncer y los resultados añaden evidencia a favor de la validez transcultural del instrumento.
Mental adjustment to cancer is an individual’s cognitive and behavioral response to the neoplasm (Ghanem et al., 2020). It is an adaptive response to the multiple changes that appear during the diagnosis of cancer and its treatment (Kang et al., 2008; Wang, Tu, Liu, Yeh, & Hsu, 2013). Coping is an appealing concept for clinicians and researchers, as it offers a means by which to adjust and recover the feeling of control in the oncological process and enhance patients’ quality of life (Zucca, Lambert, Boyes, & Pallant, 2012).
The Mini-MAC Adjustment to Cancer (Mini-MAC; Watson et al., 1994) is one of the most popular scales to gauge coping strategies in cancer patients and has been translated into multiple languages. The 29-item questionnaire exhibits psychometric properties (α coefficients .63-.89) comparable to the original 40-item MAC scale, and includes the same five subscales: Fighting spirit (FS, e.g., “I try to fight the illness”), Helplessness (HH, e.g., “I can’t handle it”), Anxious preoccupation (AP, e.g., “I am apprehensive”), Fatalism (FA, e.g., “I count my blessings”), and Cognitive avoidance (CA, e.g., “Not thinking about it helps me cope”).
The factorial structure of the Mini-MAC has been studied; however, as has occurred with its predecessor, MAC, results are inconsistent. In the Chinese version, three factors were found to FS + FA (Positive attitude), HH + AP (Negative emotion), and CA (Ho, Kam Fung, Chan, Watson, & Tsui, 2003). Four factors were found in the Norwegian (Bredal, 2010) and Korean (Kang et al., 2008) versions: the original HH, AP, and CA, and the combination of FS + FA (PA). The remaining studies have confirmed the original 5-factor structure (Anagnostopoulos, Kolokotroni, Spanea, & Chryssochoou, 2006; Fong & Ho, 2014; Grassi et al., 2005; Patoo, Allahyari, Moradi, & Payandeh, 2015; Vaillo, Pérez, López, & Retes, 2018; Wang, Tu et al., 2013). The original structure aside, Anagnostopoulos et al., 2006) also identified a second-order bifactorial structure they called adaptive (FS + FA + CA) and maladaptive (HH + AP) coping. From a practical standpoint, this simplification is valuable for clinicians, insofar as it facilitates the interpretation and clinical application of the results.
The inconsistency in the factorial structure has been attributed to various causes, such as the heterogeneity of the samples’ medical characteristics (type of tumor, stage, treatment), patient variables (age, socio-economic level, coping styles), methodological issues (the use of the explanatory factorial analysis (EFA) in most studies) (Bredal, 2010; Grassi et al., 2005; Kang et al., 2008; Wang, Tu et al., 2013, prospective study designs, or insufficient sample sizes that range from 115 to 573 participants (Bredal, 2010; Grassi et al., 2005; Wang, Tu et al., 2013), and finally, cultural traits, including the very attitude toward the disease itself (Bredal, 2010; Grassi et al., 2005; Kang et al., 2008; Wang et al., 2013). All these factors have contributed to the tremendous variability and discrepancy in the Mini-MAC’s factorial structure in the different studies (Anagnostopoulos et al., 2006; Kang et al., 2008).
In contrast, the Mini-MAC has provided meaningful evidence of validity with respect to psychosocial factors (e.g., anxiety, depression, quality of life). Thus, HH and AP scores correlate positively with anxiety and depression, whereas FS displays a negative correlation, and FA exhibits no correlation with these symptoms (Grassi et al., 2005; Kang et al., 2008). While some authors find that CA scores correlates positively with anxiety and depression (Bredal, 2010; Wang, Kelly, Liu, Zhang, & Hao, 2013; Watson et al., 1994) others do not (Ho et al., 2003; Kang et al., 2008; Patoo et al., 2015). FA and FS have been deemed in Asian societies to be positive coping styles, linked to spirituality (Ho et al., 2003; Kang et al., 2008).
In response to these limitations, this study presents a large, prospective sample of individuals with cancer, using both the EFA as well as the confirmatory factorial analysis (CFA) to evaluate the factorial structure of the Spanish version of the Mini-MAC. Therefore, the objective of the present instrumental study (Carretero-Dios & Pérez, 2007) was to provide a parsimonious factorial solution for the Mini-MAC from which scores with suitable internal consistency, test-retest reliability, and validity relations with psychological symptoms could be derived.
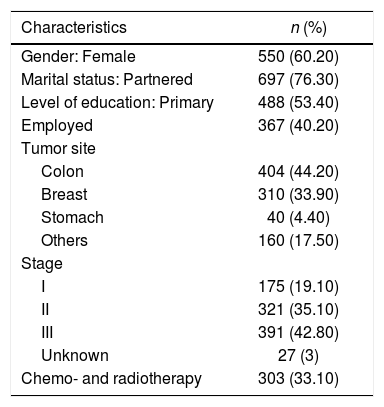
MethodParticipantsA total of 914 patients were eligible and completed the questionnaires at baseline; 550 answered the questionnaires upon completing adjuvant chemotherapy. Most of the sample was female (60.20%); mean age was 59.40 years (SD = 12.20, range 24-84). Likewise, most were married (76.30%); 53.40% had fewer than 12 years of education, and 40.20% were employed. The most common neoplasm was colorectal (n = 404), followed by breast (n = 310), stomach (n = 40), and others (n= 160). By stage, half were stage I-II (54.20%) and 74.20% of the participants had an excellent performance status (Eastern Cooperative Oncology Group [ECOG] 0). While all received adjuvant chemotherapy, 33.10% also received radiotherapy. Baseline socio-demographic and clinical characteristics of the sample can be seen in Table 1.
Baseline socio-demographic and clinic characteristics of the sample (N = 914).
| Characteristics | n (%) |
|---|---|
| Gender: Female | 550 (60.20) |
| Marital status: Partnered | 697 (76.30) |
| Level of education: Primary | 488 (53.40) |
| Employed | 367 (40.20) |
| Tumor site | |
| Colon | 404 (44.20) |
| Breast | 310 (33.90) |
| Stomach | 40 (4.40) |
| Others | 160 (17.50) |
| Stage | |
| I | 175 (19.10) |
| II | 321 (35.10) |
| III | 391 (42.80) |
| Unknown | 27 (3) |
| Chemo- and radiotherapy | 303 (33.10) |
Note. n: number, %: percentage.
The 29-item Mini-MAC (Watson et al., 1994), Spanish version (Vaillo et al., 2018). This self-rated questionnaire examines five cancer-specific coping strategies: (1) Fighting spirit (FS: the illness is experienced as a challenge and the patient has some degree of control over the situation (4 items); (2) Helplessness (HH: the individual senses irreparable loss, fears death, and lacks insight into their situation (8 items); (3) Anxious preoccupation (AP: the patient is afraid and doubts whether there is any possibility of exerting some control over the situation (8 items); (4) Cognitive avoidance (CA: the threat and need for personal control are downplayed (4 items), and (5) Fatalism (FA: the individual believes that their disease cannot be controlled and passively accepts it (5 items). Each item is scored using a 4 point Likert scale. The higher the subscale score, the more that coping strategy is used. The Spanish version of the scale was used for this study. The original Mini-MAC scores had reliability estimates (Cronbach’s alpha) ranging from .62 to .88 (Bredal, 2010). The Spanish version scores ranged from .60 to .90 (Vaillo et al., 2018).
Anxiety and depression were measured by the Brief Symptom Inventory (BSI; Derogatis, 2001). The 12-item BSI probed into patients’ sense of feeling tense, worried, depressed, and irritable, by inquiring about affective aspects of anxiety (6 items) and depression (6 items). Each item is rated from 0 to 4. Gender-specific normative data from non-patient normal were used to convert raw scores into T-scores. Higher results denote greater anxiety or depression. Alpha coefficients were between .83 and .89 (Calderon et al., 2020).
Spiritual well‐being was appraised by the validated Spanish version of the Functional Assessment of Chronic Illness Therapy-Spiritual Well‐Being Scale (FACIT-Sp; Jimenez-Fonseca et al., 2018; Peterman, Fitchett, Brady, Hernandez, & Cella, 2002). This instrument consists of 12 items scored on a five‐point scale and contains two subscales Meaning/Peace and Faith; the higher the score, the greater the person’s wellbeing. Reliability for scale ranged from .85-.86 in the Spanish sample (Jimenez-Fonseca et al., 2018).
ProcedureThe sample was taken from the NEOcoping study that enlisted 15 Spanish hospitals and 28 medical oncologists between June 2015 and February 2019. It consists of a multicenter, prospective, observational study sponsored by the Continuous Care Group of the Spanish Society of Medical Oncology (SEOM).
To be eligible, subjects had to be aged >18 years, have a histologically confirmed diagnosis of non-advanced, resected solid tumor, and be candidates for adjuvant treatment. Exclusion criteria included metastatic disease, receiving adjuvant therapy for the first time, preoperative treatment with radio- or chemotherapy, or with adjuvant hormonal or radiotherapy without chemotherapy. Of the 1,016 patients screened, 102 were disqualified (23 failed to meet inclusion criteria; 28 met exclusion criteria, and data were missing for 51). Additionally, 550 subjects participated in a test–retest reliability evaluation over a 6-month period.
A multicenter Research Ethics Committee and the Spanish Agency of Medicines and Medical Devices (AEMPS) approved this study. The study was explained and an invitation to participate was extended; all participants consented in writing before being given the questionnaires, and prior to clinical data being collected. Patients completed the questionnaires at home and returned them at the following appointment for adjuvant cancer treatment to be initiated. Subjects were followed until adjuvant treatment was ended and questionnaires were filled out again after approximately 6 months.
Statistical analysisAnalyses were conducted in five stages. First, both item and sample descriptive statistics were obtained. Secondly, EFA solutions between 1 and 5 factors were fitted in half of the sample randomly divided to ascertain the most appropriate dimensionality of the Mini-MAC. Provided that stage 2 yielded a clear, reproducible structure, a CFA was fitted in the other half of the sample at stage 3. The appropriateness and accuracy of the scores derived from the chosen FA solution for individual assessment was evaluated in the fourth stage, using a multi-faceted approach that also included a temporal-stability assessment. Finally, evidence of validity based on relations to other variables was obtained in stage 5 in two ways. Empirical validity coefficients were first obtained attained as the product-moment correlations between Mini-MAC subscale scores and anxiety, depression, and spiritual well-being scores. Secondly, model-based, theoretical evidence was determined by fitting a structural model in which the CFA in stage 2 was extended to include the external scores.
ResultsEFA solutionsStage 1 results reveal that distribution of some items is greatly skewed in both directions. Additionally, item scores are ordered-categorical, and the sample is large. Thus, the authors deemed that the non-linear item factor analysis model based on an underlying-variables approach (see e.g., Ferrando & Lorenzo-Seva, 2013, 2018) be suited the data. In order to compute the non-linear factor analysis, we followed the procedure described in Ferrando & Lorenzo-Seva, 2014: the matrix that was factor analyzed was the polychoric correlation matrix, the estimation method was Robust Unweighted Least Squares, and the fit statistics were mean and variance corrected. This general model was used in all structural analyses conducted in the study (EFAs, CFAs, and extended validity), and proved feasible in all cases. To start with, the data proved to be appropriate. The KMO index (.89) and Barlett’s test (χ2 = 10390.50, df = 406, p < .001) suggested that inter-item consistency sufficed to fit the FA model.
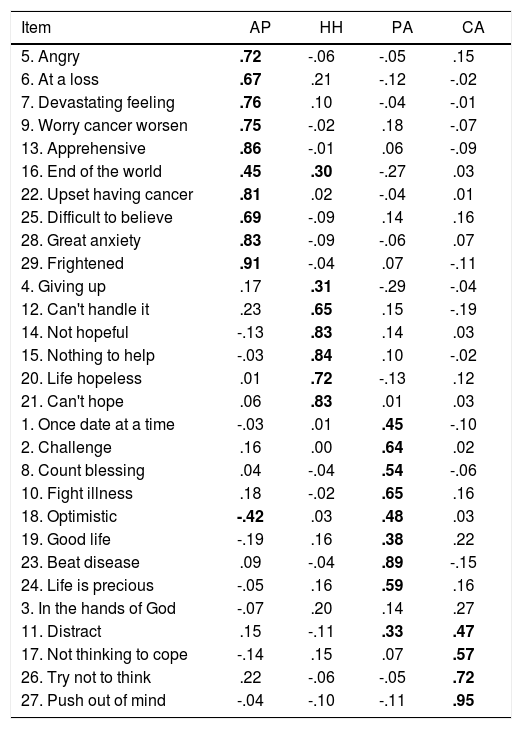
The various EFA solutions were fitted to the data from half the sample as detailed above using the FACTOR software (Ferrando & Lorenzo-Seva, 2018). Briefly put, the sequence of solutions resulted in the following. One and 2 factor solutions clearly had an unacceptable fit, whereas the 5-factor solution overfitted the data and yielded split factors when rotated. Both the three- and four-factor solutions were acceptable in purely goodness-of-fit terms. However, Schwarz’s Bayesian Information Criterion (BIC) results pointed to the four-factor solution as the best in terms of parsimony vs. fit trade-off. Likewise, this rotated solution was the most interpretable in substantive terms and the one that related most closely to the previous analyses. Goodness-of-fit results for the four-factor solution (with .95 confidence intervals) were (a) standardized root-mean-square residual (SRMS): .037 (.037; .038); (b) root-mean-square error of approximation (RMSEA): .023 (.011; .031), and (c) comparative fit index (CFI) .993 (.992; .994). Measure (a) indicates absolute fit; measure (b) denotes relative fit, and (c) is a measure of comparative fit with respect to the null independence model. In all cases, the fit is excellent (Schermelleh-Engel, Moosbrugger, & Müller, 2003). Factor analysis was rotated obliquely using the robust promin criterion (Lorenzo-Seva & Ferrando, 2019). Table 2 shows the obtained pattern matrix.
Rotated pattern matrix obtained in the exploratory factor analysis.
| Item | AP | HH | PA | CA |
|---|---|---|---|---|
| 5. Angry | .72 | -.06 | -.05 | .15 |
| 6. At a loss | .67 | .21 | -.12 | -.02 |
| 7. Devastating feeling | .76 | .10 | -.04 | -.01 |
| 9. Worry cancer worsen | .75 | -.02 | .18 | -.07 |
| 13. Apprehensive | .86 | -.01 | .06 | -.09 |
| 16. End of the world | .45 | .30 | -.27 | .03 |
| 22. Upset having cancer | .81 | .02 | -.04 | .01 |
| 25. Difficult to believe | .69 | -.09 | .14 | .16 |
| 28. Great anxiety | .83 | -.09 | -.06 | .07 |
| 29. Frightened | .91 | -.04 | .07 | -.11 |
| 4. Giving up | .17 | .31 | -.29 | -.04 |
| 12. Can't handle it | .23 | .65 | .15 | -.19 |
| 14. Not hopeful | -.13 | .83 | .14 | .03 |
| 15. Nothing to help | -.03 | .84 | .10 | -.02 |
| 20. Life hopeless | .01 | .72 | -.13 | .12 |
| 21. Can't hope | .06 | .83 | .01 | .03 |
| 1. Once date at a time | -.03 | .01 | .45 | -.10 |
| 2. Challenge | .16 | .00 | .64 | .02 |
| 8. Count blessing | .04 | -.04 | .54 | -.06 |
| 10. Fight illness | .18 | -.02 | .65 | .16 |
| 18. Optimistic | -.42 | .03 | .48 | .03 |
| 19. Good life | -.19 | .16 | .38 | .22 |
| 23. Beat disease | .09 | -.04 | .89 | -.15 |
| 24. Life is precious | -.05 | .16 | .59 | .16 |
| 3. In the hands of God | -.07 | .20 | .14 | .27 |
| 11. Distract | .15 | -.11 | .33 | .47 |
| 17. Not thinking to cope | -.14 | .15 | .07 | .57 |
| 26. Try not to think | .22 | -.06 | -.05 | .72 |
| 27. Push out of mind | -.04 | -.10 | -.11 | .95 |
Note: Values equal or larger than .30 are printed in bold. AP: Anxious Preoccupation; HH: Helplessness/hopelessness; PA: Positive Attitude; CA: Cognitive Avoidance.
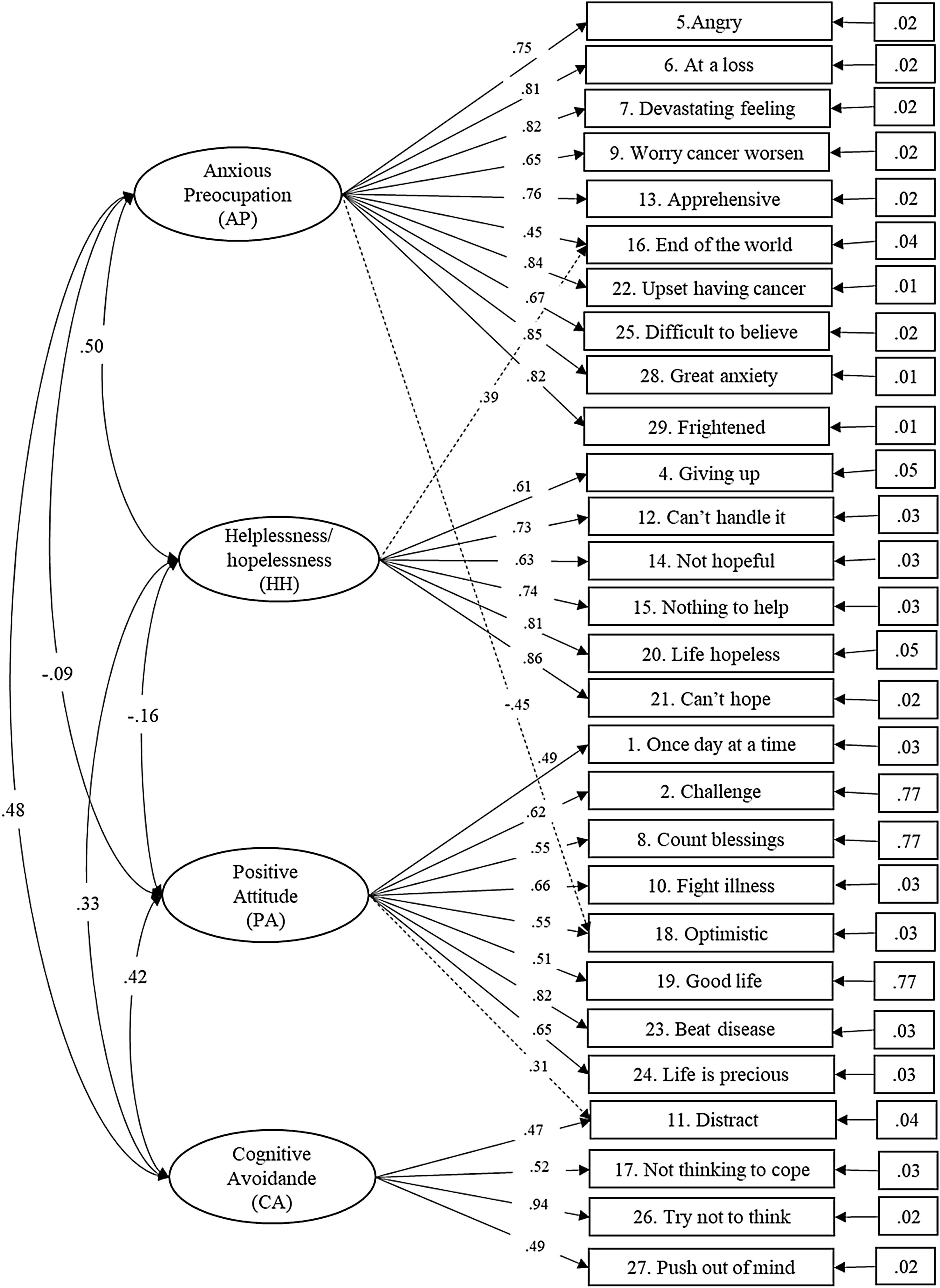
The rotated four-factor EFA solution closely approached a simple structure (Bentler’s simplicity index, was .99) and only three factorially complex items were detected. Thus, a CFA solution based on the previous EFA structure was fitted in the remaining half sub-sample with good results. Consequently, to benefit most from all the information available, the CFA model was reported based on the entire sample as the most powerful and stable for the test’s general target population. The pattern for the CFA solution was defined by: AP (items 5, 6, 7, 9, 13, 16, 18, 22, 25, 28, and 29), HH (items 4, 12, 14, 15, 16, 20, and 21), PA (items 1, 2, 8, 10, 11, 18, 19, 23, and 24), and CA (items 11, 17, 26, and 27), and the model was fitted using Mplus version 5.1 (Muthén, & Muthén, 2007). Goodness-of-fit analyses yielded RMSEA = .065 (.062; .068) and CFI = .93 which is acceptable taking into account the model’s complexity. Fig. 1 presents the model estimates in standardized metrics with the inter-factor correlation matrix. The solution was remarkably robust and replicable: The H replicability indices (see Ferrando & Lorenzo-Seva, 2018) were: .94 (F1-AP), .91 (F2-HH), .88 (F3-PA), and .90 (F4-CA).
Measurement accuracyThe suitability and accuracy of the Mini-MAC scores for individual assessment (the main use for which the test is intended) were examined in two ways. First, the (marginal) reliability of the factor score estimates derived directly from the four-factor solution above was verified. Second, McDonald’s omega estimate was used to examine the reliability of the simpler sum scale scores as proxies for the factor scores. The results are summarized as follows. The marginal reliability of the factor score estimates were: .94 (F1-AP), .95 (F2-HH), .94 (F3-PA), and .94 (F4-CA). The omega estimates corresponding to the sum scores were: .90 (F1-AP), .79 (F2-HH), .77 (F3-PA), and .76 (F4-CA). For all four factors, then, the factor score estimates directly derived from the factorial solution are highly accurate for individual assessment. In contrast, the reliability of the simple sum scores, while still acceptable (factors 1 and 2, in particular), clearly falls short of that of the factor score estimate. So, if the Mini-MAC is to be used for accurate clinical assessment, factor score estimates are preferable to simple sum scores.
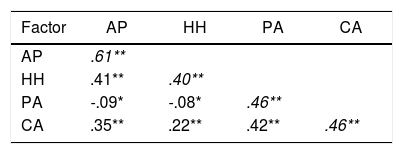
Test-retest measures obtained at the beginning and 6 months later were available for 550 patients. Table 3 illustrates test-retest estimates (stability coefficients) for the sum scale scores that range from .64 to .89. Given the protracted retest interval, these results are acceptable and consistent with the internal-consistency estimates (omega coefficients) above.
Correlations and test-retest reliability estimates of Mini-MAC scale scores.
| Factor | AP | HH | PA | CA |
|---|---|---|---|---|
| AP | .61** | |||
| HH | .41** | .40** | ||
| PA | -.09* | -.08* | .46** | |
| CA | .35** | .22** | .42** | .46** |
Note. Test-retest reliability coefficients are shown in italics on the diagonal (n = 550). AP, Anxious preoccupation; HH, Helplessness; PA, Positive attitude; CA, Cognitive voidance. *p < .05; **p < .001.
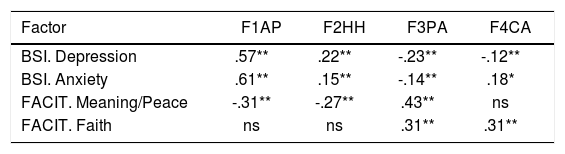
The upper panel of Table 4 shows the empirical validity coefficients previously described.
Evidence of validity.
| Factor | F1AP | F2HH | F3PA | F4CA |
|---|---|---|---|---|
| BSI. Depression | .57** | .22** | -.23** | -.12** |
| BSI. Anxiety | .61** | .15** | -.14** | .18* |
| FACIT. Meaning/Peace | -.31** | -.27** | .43** | ns |
| FACIT. Faith | ns | ns | .31** | .31** |
| (a) Model-based theoretical validity estimates | ||||
|---|---|---|---|---|
| Factor | F1AP | F2HH | F3PA | F4CA |
| BSI. Depression | .63** | .27** | -.25** | -.18** |
| BSI. Anxiety | .66** | .19** | -.15** | .24** |
| FACIT. Meaning/Peace | -.37** | -.32** | .48** | ns |
| FACIT. Faith | -.10** | ns | .38** | .27** |
| (b) Model-based standardized regression weights | ||||
|---|---|---|---|---|
| Factor | F1AP | F2HH | F3PA | F4CA |
| BSI. Depression | .67** | ns | -.18** | ns |
| BSI. Anxiety | .76** | .19** | ns | ns |
| FACIT. Meaning/Peace | -.26** | ns | .45** | ns |
| FACIT. Faith | -.18** | ns | .25** | .25** |
Note. AP: Anxious preoccupation; HH: Helplessness; PA: Positive attitude; CA: Cognitive avoidance; BSI: Brief Symptom Inventory; FACIT: Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being. *p < .05; **p < .001.
The two tables below present the results of the extended structural model based on the 4-factor CFA solution. The goodness-of-fit results are acceptable: RMSEA = .064 (.061; .066) and CFI = .91. The table in the middle contains the model-based structural validity coefficients, interpreted as disattenuated estimates in which the Mini-MAC scores are corrected for measurement error. The bottom of the table shows the standardized regression coefficients (i.e., beta weights) of the external variables on the factors.
The pattern of validity relations is similar in both approaches (empirical and model-based), albeit theoretical estimates logically tend to be higher, given the correction for measurement error, accentuating the differential results and facilitating the validity profile interpretation. Furthermore, the standardized regression coefficients (Beta) estimates suggest that AP contributes significantly to predicting anxiety and depression (.19-.45), while PA would predict meaning/peace (-.18-.45). As for the remaining evidence, the Mini-MAC factor scores that correlated significantly with all the psychological scales (particularly, AP) displayed strong positive correlations with depression and anxiety subscales (.63-.66); PA had a moderate, positive correlation with meaning/peace and faith (.38-.48).
DiscussionThis study examines the factorial structure and psychometric properties of the Spanish version of the Mini-MAC. It detects a 4-factor factorial structure, similar to that of the Norwegian (Bredal, 2010) and Korean (Kang et al., 2008) samples: AP, HH, CA, and FS + FA (PA), this last one also found in the Chinese sample (Ho et al., 2003). The first three dimensions are similar to the original scale, while PA encompasses the original scale’s FA and FS items. The structure obtained in this study agreed with previously reported results (Bredal, 2010; Ho et al., 2003; Kang et al., 2008), and was strong, replicable, and simple. Scores derived from it exhibit good psychometric properties, including good test-retest stability: the correlations obtained over the 6-month period, are similar to other studies (Fong & Ho, 2014; Kang et al., 2008). However, factor score estimates using all the information from the FA results are substantially more reliable than simple sum scores and, thus, recommended when seeking an accurate individual clinical evaluation.
As for interpretation, the first AP factor (10 items) is characterized by responding with persistent anxiety, fear, and uncertainty toward the future when faced with a diagnosis of cancer. The second factor, Hopelessness (7 items), reveals that the diagnosis of cancer is perceived as a loss and patients adopt a pessimistic attitude toward the disease. The third factor obtained is the combination of fighting spirit and fatalism resulting in a factor of positive attitude (9 items), the signature of which is acceptance of the diagnosis and searching for information about their illness to shed light on their situation. The last factor, CA (4 items), reflects the tendency to avoid direct confrontation with any and all aspects concerning the disease.
In spite of the simplicity of the factorial solution, 3 items: 11, 16 and 18 were found to have non-negligible cross-loadings onto multiple factors. In line with previous research (Bredal, 2010; Ho et al., 2003; Kang et al., 2008). Item 11 (“I distract myself when thoughts about my illness come into my head”) can be interpreted as a strategy to avoid facing the situation (HH) and, in early stages of the disease, can prove to be a good mechanism by which to deflect overwhelm (PA). As for items 16 (“I think it is the end of the world”) and 18 (“I am very optimistic”) some authors suggest that they depend on how the participants interpret their efforts to manage the demands of stressful illness-related issues (Zucca et al., 2012).
In our 4-factor model, item 3 (“I've put myself in the hands of God”) of the FA factor was eliminated because it failed to contribute significantly to the structure, in line with other studies that suggest it be removed from the questionnaire (Vaillo et al., 2018; Zucca et al., 2012).
In this study, scores derived from the AP and HH factors achieved the highest reliability estimates and led to the strongest evidence of validity with respect to the relevant external variables of anxiety and depression. These results are similar to findings of early studies and underpin the notion that these factors are good indicators of maladaptive coping (Anagnostopoulos et al., 2006) or Negative Adjustment (NA) (Bredal, 2010; Fong & Ho, 2014). Hence, AP would be a good predictor of anxiety and depression; i.e., unchecked preoccupation, fear of treatment, changes in body image, and fear of appointments and medical testing can generate emotional anguish and feelings of affliction due to these losses and changes. In these cases, in which the main coping strategy is AP, it would be advisable to involve the person in conversations in which they can share their fears and in pleasurable activities, promoting physical activity, and consulting the specialist.
AP- and HH-derived scores associated weakly with PA, as seen by other studies (Bredal, 2010; Kang et al., 2008). This can be explained by taking into account that the strategies follow a time pattern and do not appear simultaneously. AP reflects the emotional perception of cancer (feeling despondent, anxious, worried, fearful…), whereas HH would represent the more cognitive aspect (beliefs about the loss of control of the situation, feeling adrift, incapable of confronting the situation…) (Anagnostopoulos et al., 2006). Both scales can help the person re-examine their circumstances and life, avoid intrusive thoughts (CA), and look for an explanation beyond their experience or bolster their trust in destiny to adopt a more active attitude toward disease (PA). In this way, AP and HH would correspond to the emotional and mental representation of the disease and precede other coping strategies.
Positive attitude (PA), the new factor, provided reliable scores similar to those obtained in the Chinese (Ho et al., 2003) and Korean (Kang et al., 2008), samples. As for evidence of validity, PA scores exhibited moderate positive correlations with CA, meaning/peace, and faith, and weak negative correlations with AP, anxiety, and depression. These results would point toward a positive attitude being a strategy of the patient’s positive predisposition to confront the disease and/or accept reality or destiny; the latter might differ depending on culture and religious beliefs (Bredal, 2010; Kang et al., 2008), although in our study, participants considered it to be a positive attitude toward disease. Specifically, positive attitude would predict the patient’s spiritual wellbeing (meaning/peace and faith), not only reflecting acceptance of unavoidable destiny, but also an active, positive form of coping (Finck, Barradas, Zenger, & Hinz, 2018; Fong & Ho, 2014; Kang et al., 2008; Kuba et al., 2019). Its positive implication with spirituality (Alarcón, Cerezo, Hevilla, & Blanca, 2020; Bellver-Pérez, Peris-Juan, & Santaballa-Beltrán, 2019; Jimenez-Fonseca et al., 2018) might suggest that positive attitude helps patients to deal with the situation, to provide meaning, and would help decrease psychological distress.
Likewise, CA scores were associated moderately and positively with AP, HH and PA, and weakly with anxiety and depression. These results, which are consistent with those found in the original study (Watson et al., 1994), might lead us to think that CA is an indicator of poor mental adjustment in Spanish patients with cancer. Nevertheless, as suggested by other authors, CA need not necessarily be detrimental (Bredal, 2010; Calderón et al., 2018; Fong & Ho, 2014). The CA items describe an active attitude by the patient to avoid thinking about the disease and its implications (García-García et al., 2019; Ghanem et al., 2020), and that strategy can help them to achieve better affective regulation and foster the use of coping strategies that focus more on the problem. In our sample, CA was positively associated with hope (faith), unlike HH and AP; hence, the use of CA may have had a positive function in our patients, helping to tolerate, minimize, or accept the circumstances that cause them great anxiety. This would account for CA being a more effective strategy than remaining vigilant (as measured by the AP scale) (Ho et al., 2003) and a more adaptive long-term strategy, enabling the patient to elude the anguish caused by their situation (Anagnostopoulos et al., 2006; Tu, Yeh & Hsieh, 2020).
This study has several limitations. First, despite the larger sample size compared to that of other studies, it consisted of individuals with localized cancer resected with curative intent; therefore, our results cannot be generalized to patients with advanced or unresectable cancer. It would also be worthwhile to probe into differences in coping style according to tumor site. Second, this study relies on self-report measures that entail inherent biases. Finally, exploration of the dynamic nature of the pattern of strategies would be pertinent, as well as the analysis of the predictive value of the Mini-MAC dimensions with psychosocial outcomes.
In conclusion, the Spanish version of the Mini-MAC (see Appendix 1) has a clear, robust structure; it generates scores that are reliable enough to yield accurate assessments in patients with resected, non-metastatic cancer and correlates to relevant external variables with significant validity. Furthermore, results in this population corroborate earlier research on this measure, thereby upholding its cross-cultural validity.
FundingThis work was funded by the Spanish Society of Medical Oncology (SEOM) in 2015.
The authors grateful the investigators of the Neocoping study and the Supportive Care Working Group of the Spanish Society of Medical Oncology (SEOM) for their contribution to this study. We would like to thank Priscilla Chase Duran for editing and translating the manuscript. The IRICOM team for the support of the website registry and specially Natalia G. Cateriano.
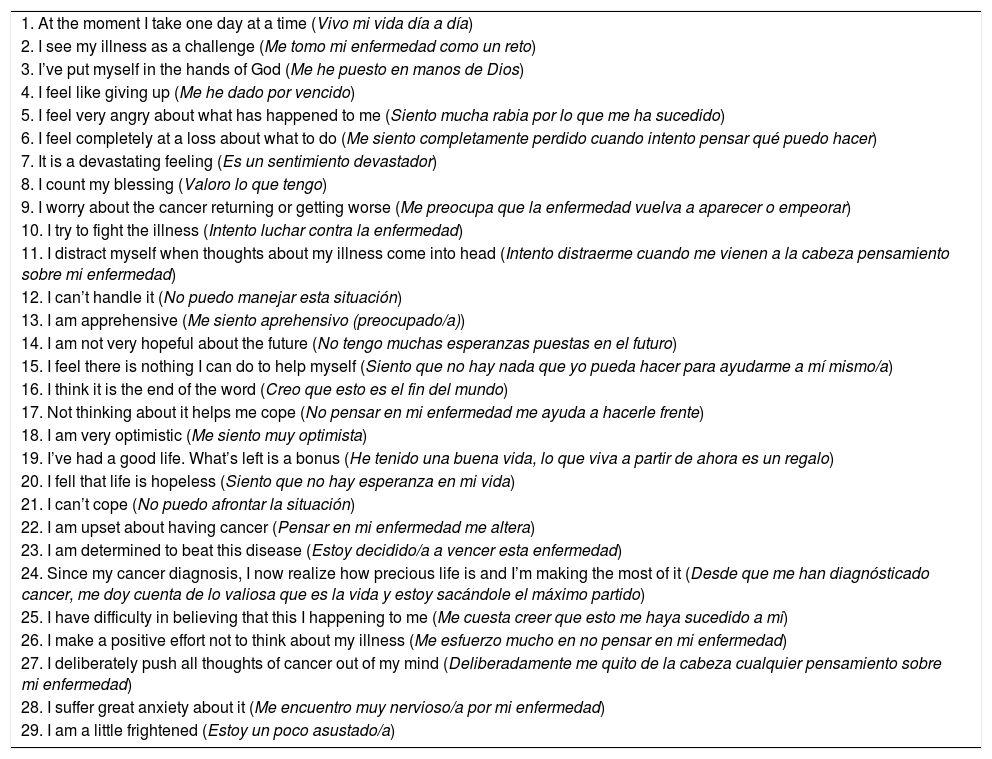
A number of statements are given below which describe people’s reactions to having cancer. Please circle the appropriate number to the right of each statement, indicating how far it applies to you at present. For example, if the statement definitely does not apply to you, then you should circle 1 in the first column.
| 1. At the moment I take one day at a time (Vivo mi vida día a día) |
| 2. I see my illness as a challenge (Me tomo mi enfermedad como un reto) |
| 3. I’ve put myself in the hands of God (Me he puesto en manos de Dios) |
| 4. I feel like giving up (Me he dado por vencido) |
| 5. I feel very angry about what has happened to me (Siento mucha rabia por lo que me ha sucedido) |
| 6. I feel completely at a loss about what to do (Me siento completamente perdido cuando intento pensar qué puedo hacer) |
| 7. It is a devastating feeling (Es un sentimiento devastador) |
| 8. I count my blessing (Valoro lo que tengo) |
| 9. I worry about the cancer returning or getting worse (Me preocupa que la enfermedad vuelva a aparecer o empeorar) |
| 10. I try to fight the illness (Intento luchar contra la enfermedad) |
| 11. I distract myself when thoughts about my illness come into head (Intento distraerme cuando me vienen a la cabeza pensamiento sobre mi enfermedad) |
| 12. I can’t handle it (No puedo manejar esta situación) |
| 13. I am apprehensive (Me siento aprehensivo (preocupado/a)) |
| 14. I am not very hopeful about the future (No tengo muchas esperanzas puestas en el futuro) |
| 15. I feel there is nothing I can do to help myself (Siento que no hay nada que yo pueda hacer para ayudarme a mí mismo/a) |
| 16. I think it is the end of the word (Creo que esto es el fin del mundo) |
| 17. Not thinking about it helps me cope (No pensar en mi enfermedad me ayuda a hacerle frente) |
| 18. I am very optimistic (Me siento muy optimista) |
| 19. I’ve had a good life. What’s left is a bonus (He tenido una buena vida, lo que viva a partir de ahora es un regalo) |
| 20. I fell that life is hopeless (Siento que no hay esperanza en mi vida) |
| 21. I can’t cope (No puedo afrontar la situación) |
| 22. I am upset about having cancer (Pensar en mi enfermedad me altera) |
| 23. I am determined to beat this disease (Estoy decidido/a a vencer esta enfermedad) |
| 24. Since my cancer diagnosis, I now realize how precious life is and I’m making the most of it (Desde que me han diagnósticado cancer, me doy cuenta de lo valiosa que es la vida y estoy sacándole el máximo partido) |
| 25. I have difficulty in believing that this I happening to me (Me cuesta creer que esto me haya sucedido a mi) |
| 26. I make a positive effort not to think about my illness (Me esfuerzo mucho en no pensar en mi enfermedad) |
| 27. I deliberately push all thoughts of cancer out of my mind (Deliberadamente me quito de la cabeza cualquier pensamiento sobre mi enfermedad) |
| 28. I suffer great anxiety about it (Me encuentro muy nervioso/a por mi enfermedad) |
| 29. I am a little frightened (Estoy un poco asustado/a) |
The format of a five-point Likert scale from 1 (Does not apply to me) to 4 (Totally applies to me).