Previous studies have shown that childhood abuse is associated with symptoms of depression. This study aims to examine the prevalence of childhood abuse or neglect and its correlation with depression among a sample of Chinese people who use methamphetamine.
MethodPeople who use methamphetamine (MA) (N = 1,173) were recruited from government-operated drug rehabilitation centres in Anhui province, China. Participants were assessed using the short form of Childhood Trauma Questionnaire and the Beck Depression Inventory-II for childhood abuse or neglect and depression symptoms.
ResultsA total of 44.6% of people who use MA reported moderate/severe childhood abuse or neglect, and 56.9% of this sample were diagnosed with depression. Emotional abuse, sexual abuse, emotional neglect and physical neglect were revealed to increase the risk of depression. Multivariable regression analyses showed that depression scores were significantly predicted by gender, duration of drug use, sexual abuse and emotional neglect (model R2 = .08, p < .001). The interaction between emotional neglect and duration of drug use on the depression was statistically significant.
ConclusionsThese analyses indicate that sexual abuse and emotional neglect increase the severity of depression in individuals who use MA in drug rehabilitation centres of China.
Estudios previos han demostrado que el abuso infantil está asociado a síntomas depresivos. El objetivo es investigar la prevalencia del abuso infantil entre consumidores de metanfetaminas en muestras chinas y su correlación con la depresión.
MétodoSe reclutan consumidores de metanfetamina (MA) del centro de rehabilitación de drogas del gobierno chino (N = 1.173). Los participantes fueron evaluados utilizando la forma corta del Childhood Trauma Questionnaire y el Inventario de Depresión de Beck-II para abuso infantil o negligencia y síntomas depresivos, respectivamente.
ResultadosEl 44,6% de los consumidores de MA reportaron abuso infantil moderado/grave, de los cuales el 56,9% fueron diagnosticados con depresión leve a grave. El abuso emocional, abuso sexual, abandono emocional y negligencia física fueron asociados al incremente del riesgo de depresión. El análisis de regresión multivariada indica que la depresión se predice de manera significativa según el sexo, la duración del consumo de drogas, el abuso sexual y el grado de negligencia emocional (R2 = 0,08; p < 0,001). El efecto de la negligencia emocional y del tiempo de consumo de drogas sobre la depresión fue significativo.
ConclusionesEl abuso sexual y el abandono emocional aumentan la gravedad de la depresión en pacientes de centros de rehabilitación de drogas en China.
The pernicious effects of childhood abuse on psychiatric health are well documented. Childhood abuse is associated with depressive symptoms, posttraumatic stress disorder (PTSD), and implicit emotion regulation deficits in studies performed on samples from communities (Afifi, Boman, Fleisher, & Sareen, 2009; Dias, Sales, Mooren, Mota-Cardoso, & Kleber, 2017; Powers, Etkin, Gyurak, Bradley, & Jovanovic, 2015). The association of childhood abuse and subsequent substance abuse has also been reported in many studies (Ai, Lee, Solis, & Yap, 2016; Enoch, 2011); childhood sexual and/or physical abuse of people who use methamphetamine (MA) was greater than those who did not (Meade et al., 2012). Childhood abuse was related to age of onset and severity of MA dependence (Messina et al., 2008). Childhood physical abuse could predict the age at first drug use (Svingen et al., 2016). Adverse experiences in childhood could increase the vulnerability of MA-associated psychosis (Ding, Lin, Zhou, Yan, & He, 2014).
An association between depression and childhood abuse or/and neglect has been found in previous studies. Individuals experienced childhood abuse were associated with twice the elevated risk of developing depressive episodes (Nanni, Uher, & Danese, 2012). Childhood sexual and physical abuse were related to high levels of depression in adults (Lindert et al., 2014). Emotional abuse and neglect, physical and sexual abuse were related to depressive symptoms in women samples (O’Mahen, Karl, Moberly, & Fedock, 2015). In addition, depression is considered to be associated with drug abuse. Twelve months and lifetime drug abuse were found to be associated with a major depressive disorder (Grant et al., 2016). One report also showed that 41.6% of adults with amphetamine abuse and dependence have lifetime depression disorder, according to national epidemiologic data (Conway, Compton, Stinson, & Grant, 2006), and MA use was significantly associated with the severity of depression (Glasner-Edwards et al., 2009).
Numerous studies had found correlations among childhood abuse, depression and drug abuse, but the conclusions of the studies differed. One of the reasons is that participants in the studies may be from different countries or regions. According to the Global Burden of Disease (GBD) 2010, 9.3 million (57.8% of the world) cases of amphetamine dependence were estimated to be the most common forms of drug dependence in Asian regions (Degenhardt, Whiteford, & Hall, 2014). China has experienced a rapid increase in methamphetamine use over the past decade. In terms of people who use MA in China, there has been limited empirical research on childhood abuse or neglect, depression and the relationship between the two. This study aims to (1) report the prevalence of childhood abuse or neglect and depression in individuals who use MA in China, (2) compare demographic characteristics of and MA use/substance use and depression in participants of no/low and moderate/severe childhood abuse, and (3) estimate the multiple factor effect, or interaction, among childhood abuse or neglect, MA use/substance use and demographic characteristics on the risk of experiencing depression.
MethodParticipants and procedureIndividuals who use MA were recruited from 7 government-operated drug rehabilitation centres in Anhui province, China. The eligibility screening criterion for MA as the main drug choice was having used before entering rehabilitation. Written informed consent was obtained. Field collective measurements (approximately 60 people per group) were conducted using a standardized structured questionnaire which included questions about socio-demographics, drug-use behaviours, childhood abuse or neglect, and depression. The participants completed the survey independently or were guided face-to-face by trained interviewers. The research design and methods were approved by the Institutional Review Board of Anhui University of Chinese Medicine. In this study, 1,256 individuals who use MA were recruited, and 1,173 individuals who use MA (aged 18-56) completed the survey; the valid completion rate was 93.4%.
InstrumentsDemographic information on age, gender, educational status, marital status, occupation and past diagnosis of psychiatric disorders or mental disorders were collected. Frequency of MA use was measured with the question: “During the 1 month (i.e., 30 days) prior to entering the drug rehabilitation centre, how many days did you use MA?” In addition to MA, the use of other illicit drugs, such as heroin, morphine, marijuana, ecstasy, ketamine, magu (a mixture of MA and caffeine), and any other addictive drugs named by participants was measured. Years (age) of first drug use and years of last drug use were recorded. Duration of drug use was calculated through first and last drug use. The history of tobacco and wine use were also recorded.
The childhood abuse or neglect of participants was assessed using the short form of the Childhood Trauma Questionnaire (CTQ-SF; Bernstein & Fink, 1998; Bernstein et al., 2003). Contains five subscales (Emotional abuse, Physical abuse, Sexual abuse, Emotional neglect, and Physical neglect) assessing the history of childhood trauma before the age of 16. ‘Moderate/severe’ cut-offs of the CTQ-SF were used to create classification: emotional abuse score ≥13, physical abuse score ≥10, sexual abuse score ≥8, emotional neglect score ≥15 and physical neglect score ≥10 (0 = no/low abuse or neglect; 1 = the presence of moderate/severe abuse or neglect for at least one of the five subscales of CTQ-SF). ‘Moderate/severe’ cut-offs were shown to be good predictors of depression, PTSD, and suicidality (Carlier, Hovens, Streevelaar, van Rood, & Van, 2016). The Chinese version of CTQ-SF was translated and validated by Zhao, Zhang, and Li (2004)). In the current sample, McDonald’s omega was acceptable for the total score (ω = .80) as well as the subscales: Emotional abuse (ω = .70), Physical abuse (ω = .82), Sexual abuse (ω = .78), Emotional neglect (ω = .85), and Physical neglect (ω = .70).
The depression of participants was assessed using the Beck Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 1996). It is a 21-item self-report questionnaire with acceptable reliability and validity in measuring depressive symptoms. The total score of BDI-II ranges from 0 to 63, with higher score showing more depressive symptoms. The cut-offs with different degrees of depression are: 0-13 showing no depression, 14-19 showing mild depression, 20-28 showing moderate depression, and 29-63 showing severe depression (Beck et al., 1996). The Beck Depression Inventory-II in its Chinese Version (BDI-II-C, ω = .87 in current study) has good criterion validity, and the aforementioned cut-offs could be used for detecting Chinese adolescent depression (Yang & Xiong, 2016). In our study, we created classifications of depression through a cut-off of 14; that is, there was no depression when BDI-II scores were less than 14 points, and there was depression when BDI-II scores were greater than or equal to 14 points.
AnalysesData were analysed using SPSS version 23.0. The prevalence rates and gender differences of childhood abuse or neglect and depression were calculated and compared. Chi-squared tests (χ2) and t tests were used to evaluate the statistical significance of the differences in demographic characteristics, substance use variables and depression symptoms (BDI-II score≥14: depression; BDI-II score<14: no depression) between the classifications of CTQ-SF scores with ‘moderate/severe’ cut-offs. A Chi-square test and crude odds ratios estimated the relationships between depression and childhood abuse or neglect. Four multiple regressions were employed to predict depression using socio-demographic characteristics, substance use variables, childhood abuse or neglect. Educational status and marital status with more than two levels were dummy-coded. To not rule out potentially important correlates, significance variables were screened using a more liberal p-value (p < .10) (e.g., Vogel, Ramo, & Rubinstein, 2018), and then the screened significance variables in the first three multiple regressions together predicted depression in fourth step (p < .05). Last, we created a classification of duration of drug use (<10 vs. ≥10 years) and explored the interactions to determine whether childhood abuse or neglect moderated the association between either gender or duration of drug use and depression in separate interactions.
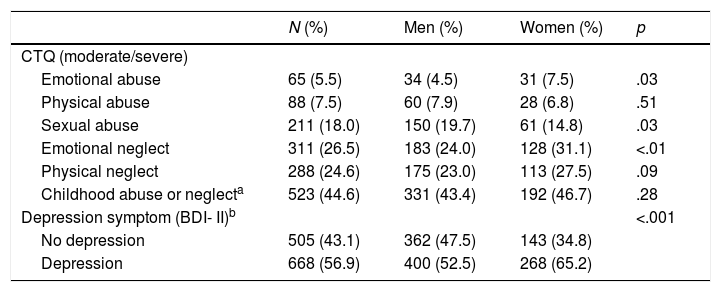
ResultsGender distribution of childhood abuse or neglect and depressionIn the current study, 1,173 (762, 65% men and 411, 35% women) participants completed all CTQ-SF and BDI-II assessments and other questions. The prevalence of childhood abuse or neglect and depression was high (see Table 1), with 44.6% (n = 523) of this sample reporting moderate/severe childhood abuse or neglect (the presence of moderate/severe abuse or neglect for at least one of the five subscales of CTQ-SF) and 56.9% (n = 668) were diagnosed with mild to severe depression according to criteria of BDI-II scores ≥14 points. We performed a Chi-Square test to examine gender differences in childhood abuse or neglect and depression. The findings revealed that moderate/severe emotional abuse and neglect of women was much greater than that of men (p < .05, p < .01), but sexual abuse was the opposite (p < .05). Moderate/severe physical abuse or neglect of the men who use MA was no different from that of the women who use MA (p > .05), and total childhood abuse or neglect was no difference between men and women (p > .05). In addition, there was a difference between men and women who use MA in depression symptoms (p < .001).
Gender distribution of moderate/severe childhood abuse or neglect and depression of participants (N = 1,173, 762 men and 411 women).
| N (%) | Men (%) | Women (%) | p | |
|---|---|---|---|---|
| CTQ (moderate/severe) | ||||
| Emotional abuse | 65 (5.5) | 34 (4.5) | 31 (7.5) | .03 |
| Physical abuse | 88 (7.5) | 60 (7.9) | 28 (6.8) | .51 |
| Sexual abuse | 211 (18.0) | 150 (19.7) | 61 (14.8) | .03 |
| Emotional neglect | 311 (26.5) | 183 (24.0) | 128 (31.1) | <.01 |
| Physical neglect | 288 (24.6) | 175 (23.0) | 113 (27.5) | .09 |
| Childhood abuse or neglecta | 523 (44.6) | 331 (43.4) | 192 (46.7) | .28 |
| Depression symptom (BDI- II)b | <.001 | |||
| No depression | 505 (43.1) | 362 (47.5) | 143 (34.8) | |
| Depression | 668 (56.9) | 400 (52.5) | 268 (65.2) |
Note. Count data using Chi-square test.
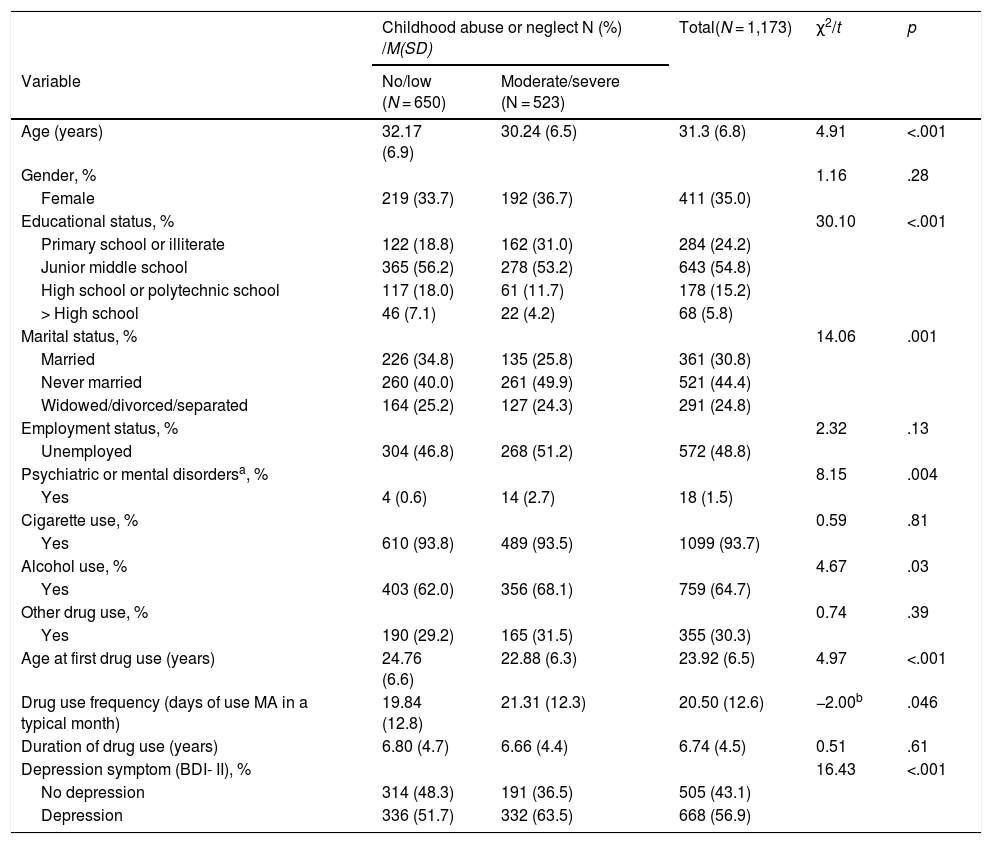
Table 2 shows socio-demographic, substance use and depression symptom characteristics and the statistically significant differences between individuals who use MA with no/low and moderate/severe childhood abuse or neglect. The final sample (N = 1,173) ranged in age from 18 to 56 years (M = 31.3, SD = 6.8) and women who use MA comprised 35% (n = 411). Education status was mainly junior middle school or below (79.0%). The participants were unmarried or widowed, divorced, separated (69.2%) or currently unemployed (48.8%); 1.5% had a past diagnosis of psychiatric disorders or mental disorders, and 30.3% reported a history of other drug use in addition to MA. The average age at first drug use was 23.9 years and the average duration of drug use was 6.74 years. Cigarette use (93.7%) and alcohol use (64.7%) history were high in participants.
Socio-demographic substance use and depression symptom distribution of participants with different childhood abuse or neglect.
| Childhood abuse or neglect N (%) /M(SD) | Total(N = 1,173) | χ2/t | p | ||
|---|---|---|---|---|---|
| Variable | No/low (N = 650) | Moderate/severe (N = 523) | |||
| Age (years) | 32.17 (6.9) | 30.24 (6.5) | 31.3 (6.8) | 4.91 | <.001 |
| Gender, % | 1.16 | .28 | |||
| Female | 219 (33.7) | 192 (36.7) | 411 (35.0) | ||
| Educational status, % | 30.10 | <.001 | |||
| Primary school or illiterate | 122 (18.8) | 162 (31.0) | 284 (24.2) | ||
| Junior middle school | 365 (56.2) | 278 (53.2) | 643 (54.8) | ||
| High school or polytechnic school | 117 (18.0) | 61 (11.7) | 178 (15.2) | ||
| > High school | 46 (7.1) | 22 (4.2) | 68 (5.8) | ||
| Marital status, % | 14.06 | .001 | |||
| Married | 226 (34.8) | 135 (25.8) | 361 (30.8) | ||
| Never married | 260 (40.0) | 261 (49.9) | 521 (44.4) | ||
| Widowed/divorced/separated | 164 (25.2) | 127 (24.3) | 291 (24.8) | ||
| Employment status, % | 2.32 | .13 | |||
| Unemployed | 304 (46.8) | 268 (51.2) | 572 (48.8) | ||
| Psychiatric or mental disordersa, % | 8.15 | .004 | |||
| Yes | 4 (0.6) | 14 (2.7) | 18 (1.5) | ||
| Cigarette use, % | 0.59 | .81 | |||
| Yes | 610 (93.8) | 489 (93.5) | 1099 (93.7) | ||
| Alcohol use, % | 4.67 | .03 | |||
| Yes | 403 (62.0) | 356 (68.1) | 759 (64.7) | ||
| Other drug use, % | 0.74 | .39 | |||
| Yes | 190 (29.2) | 165 (31.5) | 355 (30.3) | ||
| Age at first drug use (years) | 24.76 (6.6) | 22.88 (6.3) | 23.92 (6.5) | 4.97 | <.001 |
| Drug use frequency (days of use MA in a typical month) | 19.84 (12.8) | 21.31 (12.3) | 20.50 (12.6) | −2.00b | .046 |
| Duration of drug use (years) | 6.80 (4.7) | 6.66 (4.4) | 6.74 (4.5) | 0.51 | .61 |
| Depression symptom (BDI- II), % | 16.43 | <.001 | |||
| No depression | 314 (48.3) | 191 (36.5) | 505 (43.1) | ||
| Depression | 336 (51.7) | 332 (63.5) | 668 (56.9) | ||
Note. Count data using Chi-square test and measurement data using t-test.
Individuals who use MA with no/low and moderate/severe childhood abuse or neglect showed statistically significant differences in age, education status, marital status, past diagnosis of psychiatric disorders or mental disorders, alcohol use, age at first drug use, drug use frequency and depression symptom. Specifically, mean age and age at first drug use was younger and drug use frequency was higher in the moderate/severe group. In addition, the participants with moderate/severe childhood abuse or neglect reported more depression.
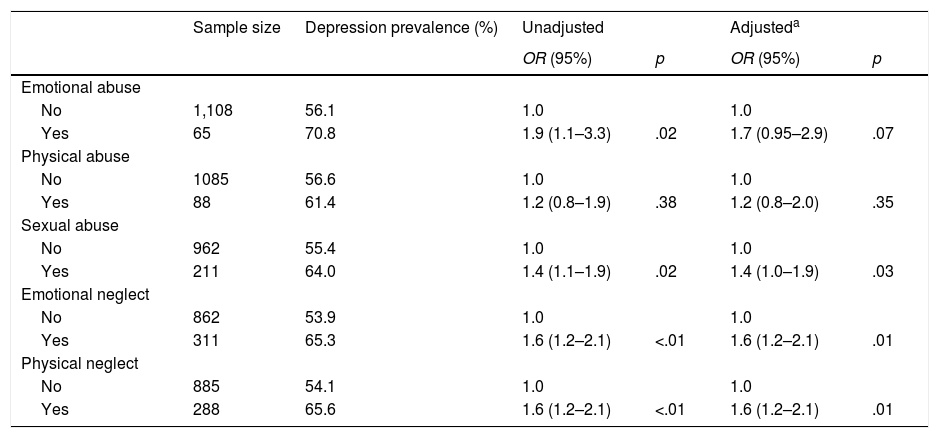
Associations between childhood abuse or neglect and depressionTable 3 shows the Chi-square test and the crude and adjusted odds ratios (ORs) for the relationships among each of five categories of childhood abuse or neglect and depression. Except for physical and emotional abuse, analyses revealed that three categories of childhood abuse or neglect were significantly associated with increased risk of depression.
Depression prevalence and odds ratios for associations between childhood abuse or neglect and depression (N = 1,173).
| Sample size | Depression prevalence (%) | Unadjusted | Adjusteda | |||
|---|---|---|---|---|---|---|
| OR (95%) | p | OR (95%) | p | |||
| Emotional abuse | ||||||
| No | 1,108 | 56.1 | 1.0 | 1.0 | ||
| Yes | 65 | 70.8 | 1.9 (1.1–3.3) | .02 | 1.7 (0.95–2.9) | .07 |
| Physical abuse | ||||||
| No | 1085 | 56.6 | 1.0 | 1.0 | ||
| Yes | 88 | 61.4 | 1.2 (0.8–1.9) | .38 | 1.2 (0.8–2.0) | .35 |
| Sexual abuse | ||||||
| No | 962 | 55.4 | 1.0 | 1.0 | ||
| Yes | 211 | 64.0 | 1.4 (1.1–1.9) | .02 | 1.4 (1.0–1.9) | .03 |
| Emotional neglect | ||||||
| No | 862 | 53.9 | 1.0 | 1.0 | ||
| Yes | 311 | 65.3 | 1.6 (1.2–2.1) | <.01 | 1.6 (1.2–2.1) | .01 |
| Physical neglect | ||||||
| No | 885 | 54.1 | 1.0 | 1.0 | ||
| Yes | 288 | 65.6 | 1.6 (1.2–2.1) | <.01 | 1.6 (1.2–2.1) | .01 |
Note. No: refers to no/low abuse or neglect; Yes: refers to moderate/severe abuse or neglect.
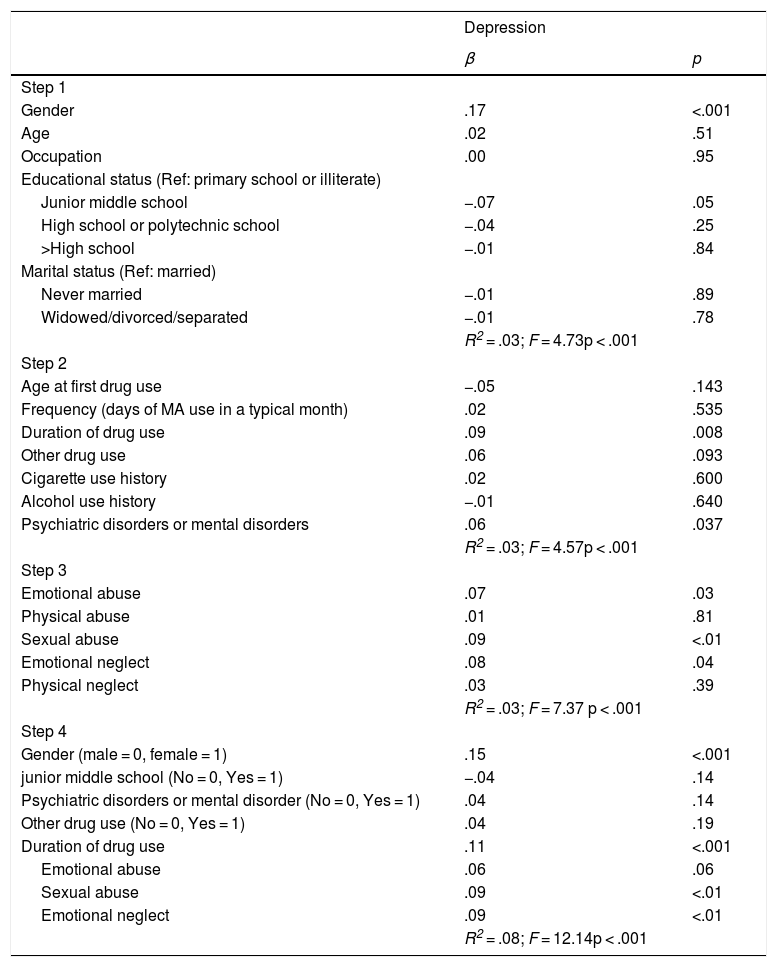
The results of multivariable regression analyses of depression scores by childhood abuse or neglect, socio-demographic and substance use variables are respectively presented in Table 4. In Step 1, we entered socio-demographic data (gender, age, occupation, educational status, marital status, past diagnosis of psychiatric disorders or mental disorders) and variables of gender, primary school or illiterate and past diagnosis of psychiatric disorders or mental disorders were screened to statistical significance variables (p < .10). In Step 2, substance use variables were entered and variables of duration of drug use and other drug use were screened to statistical significance variables (p < .10). In Step 3, variables of emotional abuse, sexual abuse and emotional neglect were screened to statistical significance variables (p < .10). Lastly, we entered screening significance variables together in three multiple regressions to predict depression scores (all variables evaluated at p < .05). The findings revealed that depression scores were significantly predicted by gender, duration of drug use, sexual abuse and emotional neglect (model R2 = .08, p < .001).
The multivariable regression analyses of depression scores by childhood abuse or neglect, socio-demographic and substance use (N = 1,173).
| Depression | ||
|---|---|---|
| β | p | |
| Step 1 | ||
| Gender | .17 | <.001 |
| Age | .02 | .51 |
| Occupation | .00 | .95 |
| Educational status (Ref: primary school or illiterate) | ||
| Junior middle school | −.07 | .05 |
| High school or polytechnic school | −.04 | .25 |
| >High school | −.01 | .84 |
| Marital status (Ref: married) | ||
| Never married | −.01 | .89 |
| Widowed/divorced/separated | −.01 | .78 |
| R2 = .03; F = 4.73p < .001 | ||
| Step 2 | ||
| Age at first drug use | −.05 | .143 |
| Frequency (days of MA use in a typical month) | .02 | .535 |
| Duration of drug use | .09 | .008 |
| Other drug use | .06 | .093 |
| Cigarette use history | .02 | .600 |
| Alcohol use history | −.01 | .640 |
| Psychiatric disorders or mental disorders | .06 | .037 |
| R2 = .03; F = 4.57p < .001 | ||
| Step 3 | ||
| Emotional abuse | .07 | .03 |
| Physical abuse | .01 | .81 |
| Sexual abuse | .09 | <.01 |
| Emotional neglect | .08 | .04 |
| Physical neglect | .03 | .39 |
| R2 = .03; F = 7.37 p < .001 | ||
| Step 4 | ||
| Gender (male = 0, female = 1) | .15 | <.001 |
| junior middle school (No = 0, Yes = 1) | −.04 | .14 |
| Psychiatric disorders or mental disorder (No = 0, Yes = 1) | .04 | .14 |
| Other drug use (No = 0, Yes = 1) | .04 | .19 |
| Duration of drug use | .11 | <.001 |
| Emotional abuse | .06 | .06 |
| Sexual abuse | .09 | <.01 |
| Emotional neglect | .09 | <.01 |
| R2 = .08; F = 12.14p < .001 |
In addition, based on the results of the multiple regression analyses, we further explored the interactions to determine whether childhood abuse or neglect moderated the association between either gender or duration of drug use and depression. The interaction between emotional neglect and duration of drug use on lifetime depression was statistically significant (p < .01), showing that individuals exposed to moderate/severe emotional neglect had significantly higher depression scores with longer duration of drug use. A simple slope analysis was used to analyse the moderating effect of emotional neglect. Using duration of drug use (<10 vs. ≥10 years) as a predictor and depression score as a dependent variable, linear regression analysis was carried out. The results showed that the standardized beta of duration of drug use was 0.09 (t = 2.53, p = .01) in the no/low emotional neglect group and was 0.25 (t = 4.61, p < .001) in the moderate/severe emotional neglect group (figure not shown). The interaction between sexual abuse and duration of drug use or gender on lifetime depression was not statistically significant, and the interaction between emotional neglect and gender on lifetime depression was also not statistically significant (figure not shown).
Discussion and ConclusionsWe investigated the prevalence of childhood abuse or neglect and depression in 1,173 individuals who use MA from 7 government-operated drug rehabilitation centres and examined the association of childhood abuse or neglect and depression. In our study, 44.6% of the participants reported moderate/severe childhood abuse or neglect. The result was similar to previous studies that showed 50.8% of individuals who use MA had undergone at least one adverse childhood experience (Ding et al., 2014). The prevalence of emotional abuse and neglect were higher among women (7.5% and 31.1% respectively) than men (4.5% and 24.0% respectively). Previous reports indicated that female alcohol abusers (Bailey, Baker, Mcelduff, & Kavanagh, 2016) and female inmates (Chen & Gueta, 2016) were more likely than males to experience emotional abuse or neglect. A study also found that female high school students who experienced emotional/sexual abuse had a higher prevalence of lifetime opioid use than male students in China (Lei et al., 2018). We found that male participants reported higher rates of sexual abuse (19.7%) in childhood compared with female participants (14.8%), which differs from a study based on Chinese adolescents (Chen, Dunne, & Han, 2004). Reasons for this contradictory result are unclear, and one plausible explanation may be differences in samples. One of the main findings of this study is that approximately 56.9% of the participants experienced mild to severe depression according to the criteria of BDI-II scores ≥14 points. That is, 52.5% of men and 65.2% of women in this sample experienced depression, and the prevalence of depression was higher among women. Several studies showed women who use MA had higher rates of depression than men who use MA (Glasner-Edwards et al., 2008; Hellem, Lundberg, & Renshaw, 2015). A recent two-year longitudinal study on Hong Kong Chinese students found that girls reported a significant increase in mean depression at a level that was higher than what was found for boys (Ho, Dai, Mak, & Liu, 2018).
In our study, individuals who use MA with moderate/severe childhood abuse or neglect were younger in age at first drug use and showed more days of drug use per month than individuals who reported no/low childhood abuse or neglect. Moreover, the two groups differed in educational status, marital status, past diagnosis of psychiatric disorders or mental disorders, alcohol use and depression. Our findings showed that emotional abuse and neglect, and sexual abuse could increase the risk of depression and predict depression scores in regression analyses of depression scores by childhood abuse or neglect. A recent study has shown that adolescents with a major depressive episode were inclined to report higher levels of emotional abuse and neglect (Gander, Sevecke, & Buchheim, 2018). Unlike prior studies (Lindert et al., 2014; Yildiz Inanici, Inanici, & Yoldemir, 2017), our study found that physical abuse was not significantly associated with increased risk of depression. Through multiple regression analysis, the present findings revealed that depression scores were significantly predicted by gender, duration of drug use, sexual abuse and emotional neglect. The duration of drug use as a factor could predict depression; this may be because MA chronic use can reduce brain concentrations of dopamine and serotonin, which leads to depression in individuals who use MA (Thomas, Angoa Perez, Francescutti-Verbeem, Shah, & Kuhn, 2010). Our findings also indicated that the interaction between duration of drug use and emotional neglect was statistically significant, with individuals exposed to moderate/severe emotional neglect having significantly higher depression scores in the presence of longer duration of drug use (≥10 years).
Our results suggest that the prevalence of emotional neglect (26.5%) ranked first among CTQ subscales in individuals who use MA, and thus emotional neglect and duration of drug use (≥10 years) as factors for depression should be paid attention by clinicians. According to viewpoint claiming that the effects of childhood trauma are treatable and preventable (Whitfield, Dube, Felitti, & Anda, 2005), individuals who use MA presenting depression symptoms should be asked about childhood abuse or neglect in order to treat depression effectively, especially those individuals with long years of drug use.
In this study, there are a few notable limitations. First, the self-reported questionnaire survey design is subject to recall bias. Second, the cross-sectional design does not assess morbidity of childhood abuse or neglect and depression, but only asks for lifetime prevalence. Third, the data were only from government-operated drug rehabilitation centres in Anhui province, and there is no control group to adjust the data, so the representation of the sample and the generalizability of the findings may be limited; moreover, it is also difficult to pinpoint whether the results of this study are specific to individuals who use MA or apply to the Chinese population in general. In addition, many of the analyses carried out may be under-powered. In future studies, larger, representative samples are needed to draw firmer conclusions.
Nonetheless, this study highlights the prevalence and correlates of both childhood abuse or neglect and depression in a sample of individuals who use MA in China. On the whole, the results suggest that the prevalence of depression and childhood abuse or neglect are high among individuals who use MA, and the risk factors of depression are screened for, such as gender, duration of drug use, sexual abuse and emotional neglect. Therefore, clinical psychologists, psychological counselors and psychiatrists observing individuals who use drug should assess childhood abuse or neglect in depressed individuals who use MA in order to treat depression effectively.