Cancellation of elective surgical cases leads to a waste of resources, financial burden, patient dissatisfaction, extended hospital stay, and unnecessary repetition of preoperative preparations.
AimThe objective of this study was to identify, analyze and manage the causes of cancellation of elective surgical cases in our institution.
MethodsThis quality improvement study compared preoperative cardiovascular event and case cancellation rates before and after implementing the practice of perioperative cardiovascular risk management. The study included the following phases: (1) Screening and identification of the most important reason for case cancellation; (2) Developing the strategy and internal protocol based on the international recommendations to minimize perioperative cardiovascular risk; (3) Implementing the internal protocol and monitoring preoperative cardiovascular events and case cancellation rate.
ResultsWe achieved a reduction in surgical case cancellation rate: 83 (3.7%) out of 2242 in 2018 and 28 (1.1%) out of 2538 cases in 2019 were cancelled after the patient had been delivered to the operating room area.
ConclusionScreening and identification of gaps in perioperative care as well as implementation of evidence-based recommendations can significantly improve the quality of patient care. In our case, implementing the internal protocol of cardiovascular risk management in perioperative period resulted in a reduction of preoperative hypertensive crisis, myocardial ischemia, heart rhythm disorder rates and in subsequently reduction in case cancellation rate.
La cancelación de casos quirúrgicos electivos conduce a un desperdicio de recursos, carga financiera, insatisfacción del paciente, estancia hospitalaria prolongada y repetición innecesaria de los preparativos preoperatorios.
ObjetivoEl objetivo de este estudio fue identificar, analizar y manejar las causas de cancelación de casos quirúrgicos electivos en nuestra institución.
MétodosEste estudio de mejora de la calidad comparó los eventos cardiovasculares preoperatorios y las tasas de cancelación de casos antes y después de implementar la práctica del manejo del riesgo cardiovascular perioperatorio. El estudio incluyó las siguientes fases: 1) Selección e identificación de la razón más importante para la cancelación del caso; 2) Desarrollar la estrategia y el protocolo interno basado en las recomendaciones internacionales para minimizar el riesgo cardiovascular perioperatorio, y 3) Implementación del protocolo interno y seguimiento de eventos cardiovasculares preoperatorios y tasa de cancelación de casos.
ResultadosLogramos una reducción en la tasa de cancelación de casos quirúrgicos: 83 (3,7%) de 2.242 casos en 2018 y 28 (1,1%) de 2.538 casos en 2019 se cancelaron después de que el paciente había sido entregado al área de quirófano.
ConclusiónLa detección y la identificación de las lagunas en la atención perioperatoria, así como la implementación de recomendaciones basadas en la evidencia, pueden mejorar significativamente la calidad de la atención al paciente. En nuestro caso, la implementación del protocolo interno de gestión del riesgo cardiovascular en el período perioperatorio resultó en una reducción de las tasas de crisis hipertensiva preoperatoria, isquemia miocárdica, alteraciones del ritmo cardíaco y, posteriormente, reducción de la tasa de cancelación de casos.
Cancellation of elective surgical cases leads to a waste of resources, financial burden, patient dissatisfaction, extended hospital stay, and unnecessary repetition of preoperative preparations.1 Causes of cancellation include patient-related factors (e.g. comorbid conditions), physician-related factors (e.g. surgeons or anesthesiologists are unavailable), inadequate preoperative evaluation, and emergency surgeries requiring rescheduling.2 The reasons for cancellation can be further classified as either avoidable or unavoidable.2
Upon preoperative assessment of high-risk patients that take multiple medications (such as beta-blockers, calcium channel blockers, angiotensin converting enzyme inhibitor, etc.) an important question for an anesthesiologist is to continue or discontinue these drugs during the perioperative period. This topic has been extensively studied previously and international guidelines have been elaborated to establish the safety of the eventual discontinuation of cardiovascular medication on the occurrence of preoperative conditions (hypertensive crisis, myocardial ischemia).3 Hospital quality improvement plays a central role in the clinical care. Even minimal changes in process of care may significantly improve outcomes of care or put patients at unnecessary risk. Identification and modification of such gaps is critical for quality improvement. During the perioperative care quality monitoring at our hospital we identified that there was high elective surgical case cancellation rate due to a high incidence of preoperative hypertensive crisis, ischemic heart disease and heart rhythm disorders patients. The purpose of this study was to identify and analyze the causes of cancellation of elective surgical cases after the patients had been delivered to the operation room and to improve the process of perioperative decision-making in our institution.
Material and methodsAfter receiving ethical approval from the Institutional Review Board of University Medical Center, we conducted a before and after study to analyze the reasons for cancellations of elective surgical procedures. The study was conducted between January 15 and December 31, 2018 (1st cohort, “before”) followed by development and implementation of the internal protocol of preoperative management of cardiovascular conditions and analysis of the cancellation occurred during a period between January and December 2019 (2nd cohort, “after”).
National Research Oncology Center (NROC) is a tertiary referral academic medical center that has a bed capacity of 280 and an operating department of 10 operating rooms (OR) distributed among eleven specialties: thoraco-abdominal surgery, hepatobiliary surgery, orthopedic surgery, gynecology, urology, vascular surgery, cardiology, plastic surgery and otolaryngology.
Study participants, sampling procedures and data collection techniqueThe study included the following phases: (1) Screening and identification of the most important reason for case cancellation (January–December 2018); (2) Developing the strategy and internal protocol based on the international recommendations to minimize perioperative cardiovascular risks (December 2018)3; (3) Implementing the internal protocol and monitoring preoperative cardiovascular events and case cancellation rate (January–December 2019).
In the analysis of cancelled cases, we included the patients in accordance with the following eligibility criteria: patients 18 years of age and older who were scheduled for an elective surgery in 2018 and then 2019. Cases were defined as patients whose surgical intervention was cancelled after the patient had been delivered to the operating room. The data were obtained from the electronic Hospital Information System of the NROC. We retrieved and identified cancelled cases (2018 and 2019) and categorized them by primary reason for cancellation.
We developed an internal protocol of perioperative patient management that mostly included anesthesiology-related recommendations from: “2014 ACC/AHA Guideline on Perioperative Cardiovascular Evaluation and Management of Patients Undergoing Noncardiac Surgery A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines”.3
The main changes that were added in the protocol:
- 1)
Preoperative serial blood pressure, pulse and rhythm assessment and monitoring;
- 2)
Continuation (unless contraindicated) of beta-blockers, calcium channel antagonists and statins. In 2018 the above-listed drugs were discontinued a couple of days before surgery and in 2019 these drugs were continued;
- 3)
Timely preoperative consulting cardiologists and other specialists if needed.
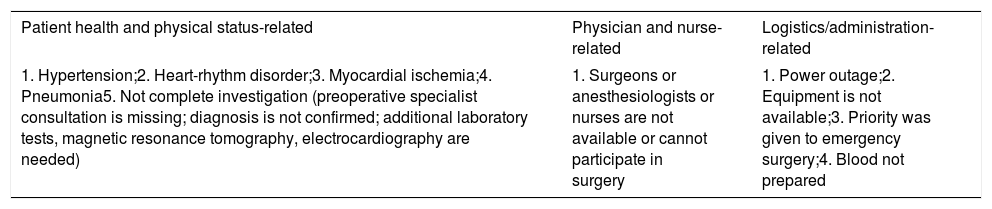
We collected the data on the following variables: the number of elective surgeries, the number of cancelled elective surgeries, and the reasons for cancellation (avoidable or unavoidable). We further categorized the causes as patient-related, physician/nurse-related (e.g. surgeons, anesthesiologists, nurses were not available) and logistics/administration-related (e.g. power outage, equipment is not available, surgical emergency). Patient-related reasons were further sub-classified into medical (e.g. hypertension-related, heart-rhythm disorder, myocardial ischemia, pneumonia and non-complete investigation) and non-medical (e.g. patient failed to show up, patient refusal) (Table 1). Potentially avoidable cancellations – those that could have been avoided by preliminary actions (a preoperative hypertensive crisis that could have been successfully prevented by appropriate preoperative medication, communication failure, no available operation rooms, list error, equipment problem), potentially non-avoidable cancellations – a patient condition that unlikely could be managed by preoperative medication, cancelled by the patient, emergency priority. We also reviewed the preoperative anesthesia assessments charts, strategies and drug prescriptions for preoperative management of patient with comorbidities.
Categorization of reasons of cancellation.
| Patient health and physical status-related | Physician and nurse-related | Logistics/administration-related |
|---|---|---|
| 1. Hypertension;2. Heart-rhythm disorder;3. Myocardial ischemia;4. Pneumonia5. Not complete investigation (preoperative specialist consultation is missing; diagnosis is not confirmed; additional laboratory tests, magnetic resonance tomography, electrocardiography are needed) | 1. Surgeons or anesthesiologists or nurses are not available or cannot participate in surgery | 1. Power outage;2. Equipment is not available;3. Priority was given to emergency surgery;4. Blood not prepared |
The criteria for cancellation of a scheduled case (if a patient had been already examined by an anesthesiologist preoperatively) was based on the assessment that the risk of the current anesthesia or surgery outweighs the risk of cancelling the surgery. Generally, these situations include cardiovascular conditions (acute myocardial infarction, acute heart failure or acute decompensation of chronic heart failure), acute pulmonary failure or acute decompensation of chronic pulmonary failure), acute infections, as well as not having a complete pre-anesthetic assessment. All patients, whose surgeries were cancelled, were hospitalized at least 1 day before surgery. The preoperative assessment was conducted by an anesthesiologist a day before the surgery or earlier in selected cases if it was necessary. The anesthesiologist could require the cardiology assessment if necessary.
In order to cancel a case, the cancellation criteria should have been met, and collegial consensus (anesthesiologist, chief of anesthesia department, an operating surgeon and chief of the surgical department) should have been reached.
If an anesthesiologist requested a consultation by cardiologist, pulmonologist, neurologist in the operation room and decision on cancellation was made collegially (an anesthesiologist, a surgeon and a cardiologist). For the purposes of this work, and if we identified two reasons for cancellation (for example hypertensive crises and absence of cardiologist consultation), we categorized this case accordingly to the most important reason (hypertensive crisis).
Since the main reasons for case cancellation included cardiovascular conditions, a process was put in place directed towards an evidence-based improving preoperative management of these conditions (arterial hypertension, ischemic heart disease and heart rhythm disorders) in the preoperative period.
Data analysisThe data were entered, checked, cleared, and analyzed by using SPSS version (20.0). Descriptive and basic analytical statistics were used.
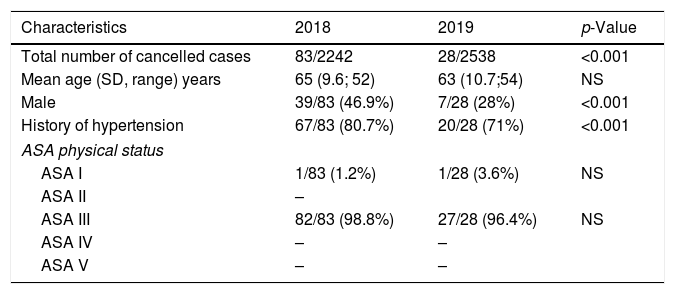
ResultsA total of 2242 elective surgical procedures were scheduled in 2018 and 2538 in 2019. Gender was balanced in our cohort (Table 2). The mean age was 65 and 63, respectively. Most of patients included in the study, were hospitalized to receive treatment for advanced malignancies (lung, stomach, pancreas, liver cancers) and end stage renal failure. The most common surgeries performed in these patients included pneumonectomy, lobectomy, gastrectomy, liver resection, pancreaticoduodenal resection, and renal transplantation. The types of surgeries performed in 2018 and 2019 and patients’ physical status were more or less homogeneous.
Baseline characteristics and demographics.
| Characteristics | 2018 | 2019 | p-Value |
|---|---|---|---|
| Total number of cancelled cases | 83/2242 | 28/2538 | <0.001 |
| Mean age (SD, range) years | 65 (9.6; 52) | 63 (10.7;54) | NS |
| Male | 39/83 (46.9%) | 7/28 (28%) | <0.001 |
| History of hypertension | 67/83 (80.7%) | 20/28 (71%) | <0.001 |
| ASA physical status | |||
| ASA I | 1/83 (1.2%) | 1/28 (3.6%) | NS |
| ASA II | – | ||
| ASA III | 82/83 (98.8%) | 27/28 (96.4%) | NS |
| ASA IV | – | – | |
| ASA V | – | – | |
Total number of scheduled cases: in 2018 – 2242, in 2019 – 2538.
Abbreviations: SD, standard deviation; ASA, American Society of Anesthesiologists; NS, not significant.
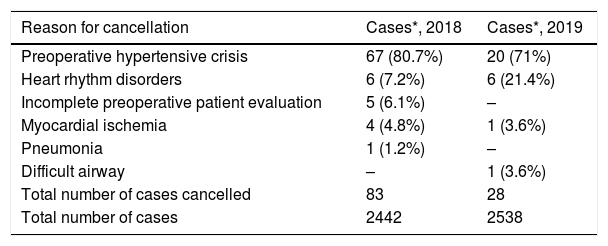
Our results show that we achieved a significant reduction in surgical case cancellation rate: 83 (3.7%) out of 2242 in 2018 and 28 (1.1%) out of 2538 cases in 2019 were cancelled after the patient had been delivered to the operating room area (Table 3). Among them, 1 (1.2%)/83 in 2018, and 1 (3.6%)/28 in 2019 had American Society of Anesthesiologists class of 1; 82/83 (98.8%) in 2018 and 27/28 (96.4%) in 2019 had a class of 3. All cancellations were due to patient-related medical reason and all cases were cancelled before anesthesia was induced (Table 3). After implementing the internal protocol of cardiovascular risk management in perioperative period there was a substantial reduction in preoperative hypertensive crisis, myocardial ischemia, heart rhythm disorder rate and consequently case cancellation rate (Table 3).
Reasons for cancellation.
| Reason for cancellation | Cases*, 2018 | Cases*, 2019 |
|---|---|---|
| Preoperative hypertensive crisis | 67 (80.7%) | 20 (71%) |
| Heart rhythm disorders | 6 (7.2%) | 6 (21.4%) |
| Incomplete preoperative patient evaluation | 5 (6.1%) | – |
| Myocardial ischemia | 4 (4.8%) | 1 (3.6%) |
| Pneumonia | 1 (1.2%) | – |
| Difficult airway | – | 1 (3.6%) |
| Total number of cases cancelled | 83 | 28 |
| Total number of cases | 2442 | 2538 |
Chi squared equals 45.213 (p<0.005).
The most common reason for the cancellation was preoperative hypertensive crisis: 67/83 (80.7%) in 2018 and 20/28 (71%) in 2019; followed by heart rhythm disorders: 6/83 (7.2%) in 2018 and 6/28 (21.4%) in 2019 (Table 3). Incomplete preoperative patient evaluation in 2018 constituted 5/83(6.1%) and included incomplete cardiovascular clearance (ECG not done, the absence of cardiologist consult), pulmonary clearance (spirometry not done, the absence of pulmonologist consult), neurological clearance (MRI not done, the absence of neurologist consult); in 2019 there were no incomplete preoperative patient evaluation. All patients, whose surgeries were cancelled because of hypertensive crisis (n=67/2242 in 2018 and n=20/2538 in 2019) had hypertension in their history, and the reason of the preoperative hypertensive crisis was either poorly controlled hypertension or/and discontinuation of preoperative antihypertensive medication (primarily beta-blockers). All cancelled cases were rescheduled to a later date after completion of preoperative evaluation and medical therapy (antihypertensive, antianginal, antiarrhythmic, antibacterial).
The review of preoperative anesthesia consultations showed that in 2018 prior to the implementation of the program, there was inconsistency in preoperative anesthesia assessment and drug prescriptions for preoperative patient management (including management of arterial hypertension, heart rhythm and conduction disorders, ischemic heart disease). Beta-blockers and calcium channel blockers were cancelled prior to surgery in 2018 and continued during the entire perioperative period in 2019.
DiscussionThe analysis showed that cardiovascular events were the most common reasons for cancellation of the elective surgery and majority of cancellations could have been avoided by more thorough a proper preoperative assessment, adjustment of medication and prescription of targeted premedication in selected patients.
A recent meta-analysis showed that the prevalence of case cancellation was very high in low and middle-income countries and the majority of cancellations could be avoided by preoperative patient evaluation and preparation.4
Cancellation of elective surgeries is a global problem with an incidence ranging from 1 to over 23%.5,6 Kaddoum et al. showed that 55% of surgeries were cancelled because of workup-related factors, 7% due to patient-related factors, 22% due to admission-related factors and 12% – due to surgeon/facility-related factors.7
We found that the patient-related factor of the hypertensive crisis was the most common reason for the cancellation of surgery in our hospital. Arterial hypertension is present in up to 30% of patients scheduled for non-cardiac surgery.8 A history of poorly controlled hypertension is associated with an increased risk of perioperative mortality in non-cardiac surgery and an increased risk of perioperative complications such as stroke, myocardial ischemia, and acute heart failure.9 It has also been shown that about 25% of the patients undergoing non-cardiac surgery and 80% undergoing cardiac surgery have perioperative hypertension and the history of hypertension can increase the perioperative cardiovascular complications by 35%.10–12 It was recommended to cancel elective surgery if the systolic blood pressure was higher than 180mmHg or if the diastolic blood pressure was higher than 110mmHg.12
The preoperative diastolic blood pressure higher than 110mmHg was associated with increased complications such as cerebrovascular events, myocardial ischemia and infarction, heart rhythm disorders, and renal failure.13 There is no sufficient evidence to suggest that preoperative arterial pressure monitoring should alter decisions to cancel surgery or not.14 The use of preoperative arterial pressure appears promising to guide intraoperative decisions.14 The majority of our case cancellations due to a patient's health condition were intended to avoid perioperative complications such as stroke, acute myocardial infarction, heart failure, and fatal dysrhythmias. The challenge facing the anesthetist who is confronted with a hypertensive patient prior to surgery is whether to proceed with the surgery and stabilize the patient's condition in the preoperative period or to simply cancel the case. There may be institutional and logistical reasons pressures to do the former and the anesthesiologist can readily reduce the blood pressure, but its rapid reduction can result in cerebral ischemia (levels of autoregulation remain abnormal) and increase the risk for perioperative ischemic stroke. Recent work on the increase in mortality, cardiac injury, and renal injury with intraoperative hypotension often defined as mean arterial pressure<65mmHg maybe relevant here as it is unclear what defines “hypotension” in chronic hypertensive.
Disorders of heart rhythm were the second most common cause of surgery cancellation in our hospital. The incidence of atrial fibrillation in patients undergoing non-cardiac thoracic or abdominal surgeries has been estimated to be from 8% to 13%.15 Beta blockers can reduce the incidence of atrial fibrillation.16
It is difficult to eliminate all possible causes of perioperative dysrhythmia even if appropriate antiarrhythmic drugs are prescribed preoperatively. Several patient factors including age, history of coronary artery disease, hypertension, obesity, enlarge atria increase the risk of perioperative arrhythmias.17,18
The third most common cause of case cancellation in our study was myocardial ischemia. Although it is critically important to diagnose perioperative myocardial ischemia in a timely fashion, it is quite difficult to do so in the anesthetized or sedated patient.
We also found that patients of American Society of Anesthesiologists class III in both cohorts (2018 and 2019) were at highest risk for case cancellation due to cardiovascular conditions such as hypertensive crisis, dysrhythmia and myocardial ischemia (Table 2).
We did not find even a single case that was cancelled due to lack of operating room time, or absence of the patient or surgeon. This is a notable difference from the findings in other studies.19 Likely, this has much to do with the differences in health care systems. Notably, the surgical volume at our medical center is much less than in many other hospitals. Thus while our results may not be generalizable, it is a worthwhile exercise for every institution to examine their own reasons for cancellations and implement local context quality improvement interventions. Our findings reveal that there is a need in our institution to improve preoperative patient assessment prior to OR arrival, to improve preoperative diagnosis of poorly controlled hypertension, and for better adjustment of perioperative antihypertensive therapy. It may be difficult to prepare the patient for surgery (for example select the right drug and dose of antianginal or antiarrhythmic drug to fully control these diseases) if preoperative consultation takes place only a few hours before an operation, therefore, our patients may benefit from consultation at the preoperative anesthesia clinics several days before the surgery.
The limitations of this study include being a single-centered, the short period of follow up and the small sample size. It is also affected by its non-experimental design, but we do not consider that this work may be affected by threats to internal validity linked with problems of patient history, heterogeneity, maturation, testing, instrumentation, regression to the mean, differential selection or attrition. Another limitation is that in complex interventions like this, and given that the internal protocol implemented (started in 2019) contains several changes, it is difficult to conclude what exactly led to a reduction in preoperative cardiovascular events. The data available for the before-after analysis is also a limitation to mention. Nevertheless, before-after designs are typical for small local quality improvement initiatives, although they may overestimate the effectiveness of the intervention.20
Finally, the value of this quality improvement process is that it helped us understand the main reasons for case cancellations and plan changes that resulted in a significant reduction in preoperative cardiovascular events. Future changes, such as the implementation of preoperative anesthesia clinics, where anesthesiologists conduct preliminarily preoperative patient assessments, might further contribute to a reduction in cancellation rates while improving blood pressure and heart rhythm control, reduce risk of perioperative myocardial ischemia and other conditions.
In conclusion, screening and identification of gaps in perioperative care as well as implementation of evidence-based recommendations can significantly improve the quality of patient care. In our case, implementing the internal protocol of cardiovascular risk management in perioperative period resulted in a reduction of preoperative hypertensive crisis, myocardial ischemia, heart rhythm disorder rate and subsequently reduction in case cancellation rate.
Author contributionsDV contributed to the study design. DV, AS, YU contributed to data acquisition. DV contributed to drafting the manuscript. DV, ASS and BB contributed to writing and critical revision of the manuscript. ASS contributed to the statistical analysis. All authors read and approved the final version.
Ethics approval and consent to participateThe study was approved by the Local Ethics Committee of the University Medical Center (UMC, Nur-Sultan, Kazakhstan).
Conflict of interestThe authors report no proprietary or commercial interest in any product mentioned or concept discussed in this article.