Surgical patients are at risk of hospital-acquired venous thromboembolisms (VTEs), and preventative measures such as thromboembolism deterrent stockings (TEDs) and low molecular weight heparin (LMWH) are proven to be beneficial. The National Quality Requirement in the NHS Standard Contract 2017/19 in England mandates that 95% of inpatients undergo VTE risk assessments. As hospitals transition to Electronic Patient Records (EPR), it is important to observe the impact on vital safety indicators such as VTE risk. The aim of this study is to observe the effect of implementing EPR in a tertiary centre on adherence to national guidelines, including VTE assessment rates and prophylaxis administration in surgical patients.
Materials and methodsUsing consecutive sampling, all acute surgical admissions at the hospital from 26/02/2018 to 18/03/2018 (n=154) pre-EPR and 31/10/2018 to 25/11/2018 (n=151) post-EPR were observed for VTE risk assessment, 24-h re-assessment, prophylaxis prescriptions, administration, and patient compliance. Data was compared using a two-tailed Z-test.
ResultsPre-EPR, 96% of patients had completed VTE assessments, which increased after EPR implementation to 97% (p=0.39). LWMH prescription rates decreased from 82% to 77% following EPR (p=0.14). Moreover, TED prescriptions decreased from 84% to 64% post-EPR (p<0.01). Administration rates of prophylaxis generally improved post-EPR. The 24-h re-assessment rate decreased from 62% to 54% of patients (p=0.08).
ConclusionThe study demonstrated that EPR is non-inferior to paper records. Transitioning to an EPR system did not interfere with the completion of VTE risk assessments, hence did not negatively impact the ability to achieve national targets.
Los pacientes quirúrgicos tienen un riesgo especial a padecer tromboembolismos venosos (TEV) y las medidas preventivas han demostrado ser beneficiosas. El Requisito Nacional en el Contrato del Servicio Nacional de Salud (NHS) 2017/19 asignó como mandato que el 95% de los pacientes tienen valoraciones de riesgo de TEV. Debido a la transición a los registros electrónicos de pacientes (EPR), es importante observar su impacto en estas evaluaciones. El objetivo de este estudio es observar el efecto de la implementación del EPR en un hospital terciario con respecto a las valoraciones de TEV y a la administración de profilaxis en pacientes quirúrgicos.
Materiales y métodosTodas las admisiones quirúrgicas agudas del hospital fueron observadas desde el 26 de febrero del 2018 al 18 de marzo del 2018 (n = 154) antes de la implementación del EPR y desde el 31 de octubre del 2018 al 25 de noviembre del 2018 (n = 151) después del EPR. El riesgo de TEV, la reevaluación de 24 horas, la prescripción de profilaxis, la administración y el cumplimiento de los pacientes fueron recolectados con el muestreo consecutivo. Comparamos estos datos con una prueba Z.
ResultadosAntes del EPR, el 96% de los pacientes tuvieron evaluaciones de TEV completas, esto aumentó después del EPR al 97% (p = 0,39). Las prescripciones de la heparina de bajo peso molecular (HBPM) disminuyeron del 82 al 77%, posterior al EPR (p = 0,14). Además, las prescripciones de calcetines de compresión de disuasión tromboembólica (TED) disminuyeron del 84 al 64% (p < 0,01) y las tasas de administración de profilaxis mejoraron. La reevaluación de 24 horas disminuyó del 62 al 54% (p = 0,08).
ConclusionesEste estudio mostró que el EPR no es inferior que los registros de papel. La transición a este no interfirió con las evaluaciones y se siguieron cumpliendo los requisitos nacionales.
A venous thromboembolism (VTE) is an acute, vascular, and major preventable cause of morbidity and mortality. VTE's present as deep venous thrombosis (DVT) in the deep veins of the lower leg, or as pulmonary embolisms (PE) in the lungs. The interplay of factors including venous stasis, vessel injury, and hypercoagulability lead to VTE formation. If untreated, the mortality of PEs can reach 25%.1 50–60% of VTEs are hospital-acquired, which occur within 90 days of a hospital admission. Hospital inpatients, particularly trauma and surgical patients, are at significant risk of vascular events, wherein a main factor is decreased mobility. This has led to extensive public health measures to limit the incidence of hospital acquired VTEs.2
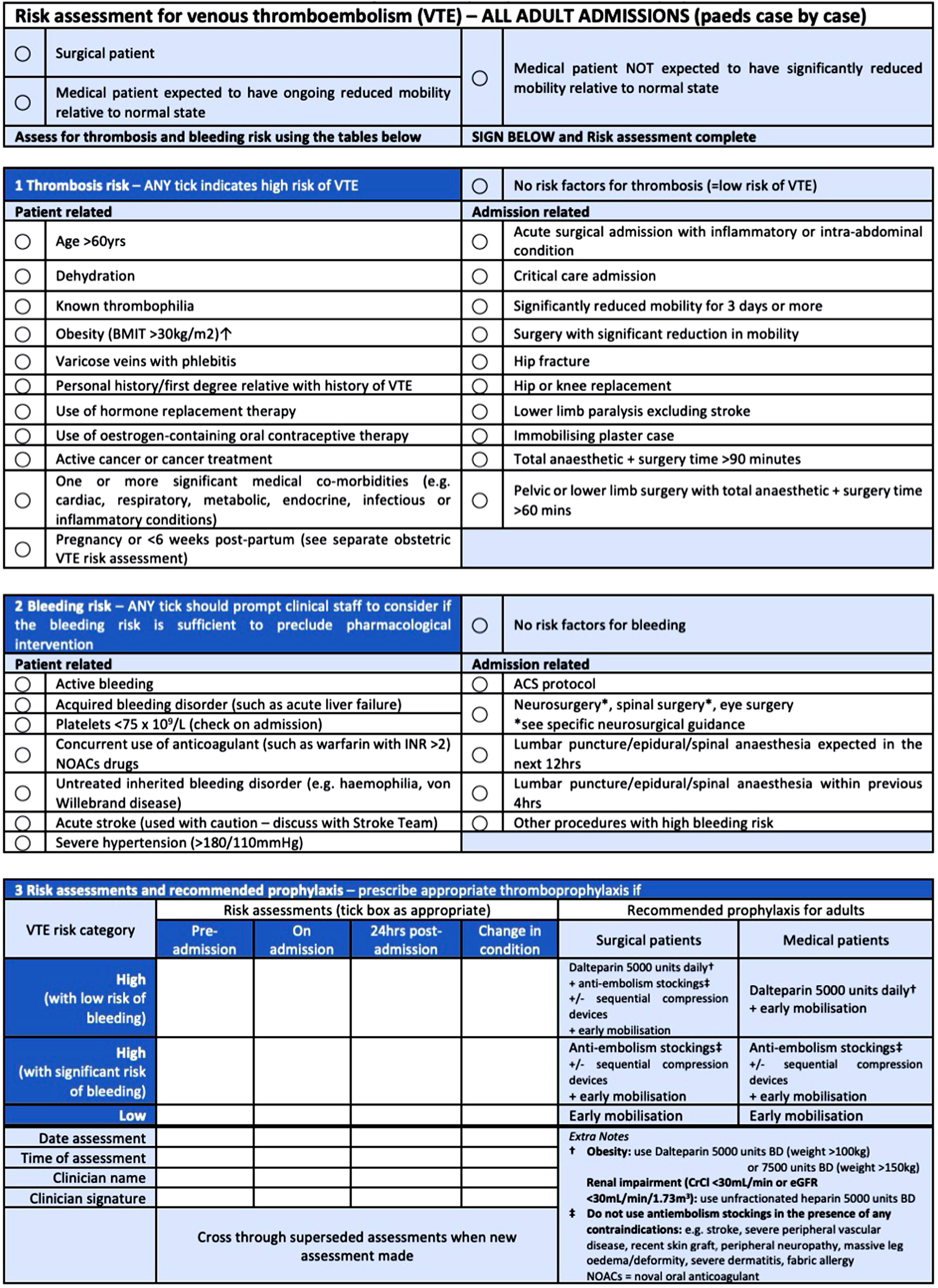
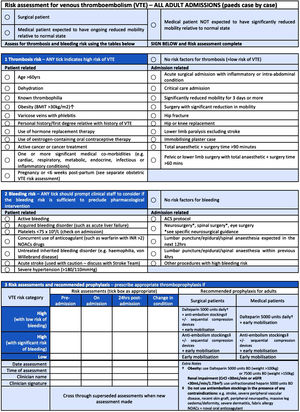
As such, the National Institute for Health and Care Excellence (NICE) guidance states that all hospital patients must have their VTE risk assessed. The guidance standardises risk assessment, management, and prevention of VTEs. Although no particular tool is mandated, all hospitals must use a tool that is published by a “UK body, professional network or peer-reviewed journal”.3 The Department of Health's VTE risk assessment is commonly used. It assesses mobility, thrombosis, and bleeding risk to advise on thromboprophylaxis (Fig. 1). Furthermore, the guidance states that assessments should be completed soon after hospital admission and before the first consultant review. The risk should be re-assessed if the clinical condition changes or before subsequent consultant reviews, and prophylaxis adjusted accordingly. VTE prophylaxis measures should be guided by patient risk and contraindications.
In patients with lowered mobility, mechanical prophylaxis such as thromboembolism deterrent (TED) stockings may be indicated. These devices increase venous blood-flow and decrease stasis to prevent thrombus formation.4 Some patients require pharmacological interventions, most commonly low molecular weight heparin (LMWH), which should be initiated within 14h of admission. The burden of VTEs can be prevented using the simple, cost-effective thromboprophylaxis interventions. To provide incentive for National Health Service (NHS) Trusts to follow guidance, the National Quality requirement in NHS Standard Contract 2019/2020 state that at least 95% of inpatients need to undergo VTE risk assessment, and if trusts fail to meet this target, they may be subject to a fine.5
Traditionally, NHS hospital trusts have used paper-based patient records for VTE assessments. This process was deemed obsolete due to its susceptibility to human error and low productivity.6 Therefore, on the 7th January 2019, NHS England published the ‘NHS Long TermPlan’ stating the national priorities for healthcare over the next 10-years.7 All trusts are required to switch from paper-based records to digital records by 2023. As such, St George's Hospital (SGH) NHS trust started the gradual shift to Electronic Patient Records (EPR) in 2018, limiting the use of paper-based records to select departments. Therefore, the process for VTE assessment, prescriptions and documentation evolved to fit the new record keeping system.
Prior to the implementation of EPR, a designated area in paper drug charts (Fig. 1) was used for VTE assessment and prescription. Patients were risk assessed and appropriate VTE prophylaxis was then prescribed. However, the implementation of EPR requires VTE assessments to be completed electronically. The computer system prompts clinicians to complete the forms, enter prescriptions and administer them. Similarly, 24-h VTE risk reassessments are completed electronically, with pop-up reminders for staff. These built-in electronic measures are expected to increase adherence to VTE assessments. As correct VTE assessment and prescription is vital to patient safety and avoiding fines, this research aims to determine the effect of EPR on adherence to national VTE assessment guidelines, including VTE assessment rates and prophylaxis administration in surgical patients in the early stages of switching to the electronic system at SGH NHS Trust. It is hypothesised that the assessment, prescription and implementation of LMWH and TED stockings would increase with the implementation of EPR, allowing the trust to meet a higher number of assessments.
Materials and methodsStudy design and participantsA cross-sectional study observing all general surgery patients at SGH from 26th February to 18th March (n=154) and 31st October to 25th November (n=151) 2018 was completed by manually searching patients’ notes for baseline information on adherence to national VTE prophylaxis guidelines. During the first data collection period (February to March), patient's hardcopy medical records were reviewed. This was analysed and compared to the National Quality Requirement in the NHS Standard Contract 2017/2019 of 95% patients undergoing VTE risk assessment. Seven months later (October to November) the EPR system was introduced, after which a further observation of prophylaxis adherence was conducted.
Thromboprophylaxis types assessed were subcutaneous LMWH and TED stockings. The recommended prophylaxis methods, their administration and monitoring are based off the Department of Health's Risk Assessment for VTEs, NICE guidelines,3 and SGH NHS Trust procedures. All patients admitted under the general surgery team, either as an emergency or elective admission were included in this study. Exclusion criteria encompassed patients under 18 years of age.
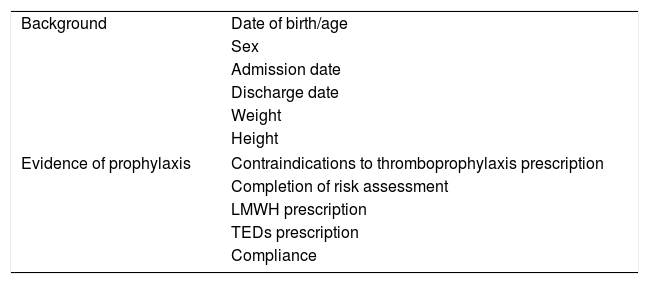
Data collectionSurgical take lists were reviewed by the authors under the local registrar's supervision every morning. Patients’ notes were accessed and analysed for (Table 1):
- •
Conduction of VTE prophylaxis risk assessment – on drug charts or informally on notes during admission and re-assessment 24-h later (Fig. 1);
- •
Accuracy of risk assessment – filling out assessment sheets, recording the date, time, and signature;
- •
If prophylaxis was prescribed correctly and if contraindications were recorded using risk stratification for thrombosis and bleeding risk, and co-morbidities (such as obesity, and renal impairment) according to NICE guidance. These factors determine whether a patient is high or low risk of VTE (Fig. 1);
- •
Patient compliance – assessed by data collectors checking if medication had been taken, TED stockings had been given and correctly worn.
According to SGH NHS Trust, such studies do not require ethical approval as they fall under the premise of ‘internal audits’. The study was conducted in accordance to The Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans. The privacy rights of human subjects were strictly observed.
Statistical analysisStatistical analysis was carried out using Statistical Package for the Social Sciences (SPSS) version 21.0. Descriptive statistics were used to compare demographic and clinical variables. Demographics were compared using the two-tailed Mann–Whitney U Test and Chi-squared test. Two data sets were compared, pre- and post-implementation of EPR, to observe its impact on adherence. A two proportion Z-test was used to compare the data of the two populations. These results were compared with a p-value, with a level of significance set at p<0.05 (Tables 2–5).
Demographics of study participants.
| Pre-implementation of EPR (n=154) | Post-implementation of EPR (n=151) | p-Value | |
|---|---|---|---|
| Age (mean±SD) | 52±20.48 | 52±20.59 | 0.83 |
| Sex | |||
| Female (n (%)) | 102 (66%) | 83 (55%) | |
| Male (n (%)) | 52 (34%) | 68 (45%) | 0.04 |
| Risk of VTEa | |||
| High (n (%)) | 75 (49%) | 62 (41%) | |
| Low (n (%)) | 79 (51%) | 89 (59%) | 0.18 |
| BMI (mean±SD) | 25.7b±4.80 | 26.9c±3.70 | 0.62 |
The study sample pre- and post-implementation of EPR were similar for age. Importantly, factors affecting the prescription of VTE prophylaxis i.e. risk of VTE and BMI were comparable. There was a difference in sex distribution pre- and post-implementation of EPR.
EPR: Electronic Patient Record; BMI: Body Mass Index (weight/height2); VTE: Venous Thromboembolism; n: number; SD: Standard Deviation.
Patients were categorised as high risk if there was at least one risk factor for VTE present as outlined in NICE guidelines [NG89] (Fig. 1).
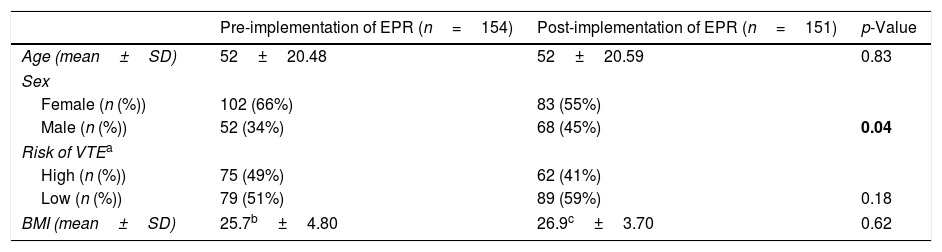
Initial VTE assessment and 24-h reassessment in pre- and post-EPR implementation populations.
| Pre-implementation of EPR (n (%)) | Post-implementation of EPR (n (%)) | % change | p-Value | |
|---|---|---|---|---|
| n=154 | n=151 | |||
| VTE assessment completed | ||||
| Correctly | 141 (95%) | 137 (94%) | −2.84% | 0.40 |
| Incorrectly | 7 (5%) | 9 (6%) | −28.57% | 0.29 |
| Total | 148 (96%) | 146 (97%) | −1.35% | 0.39 |
| VTE assessment not completed | 6 (4%) | 5 (3%) | −16.67% | 0.39 |
| 24-h reassessment | ||||
| Correctly | 88 (96%) | 75 (95%) | −14.77% | 0.08 |
| Incorrectly | 4 (4%) | 4 (5%) | 0.00% | 0.49 |
| Total | 92 (62%a) | 79 (54%a) | −14.13% | 0.08 |
| 24-h reassessment not completed | ||||
| No reason | 32 (57%) | 47 (70%) | 46.88% | 0.02 |
| Discharged | 24 (43%) | 20 (30%) | −16.67% | 0.27 |
| Total | 56 (38%a) | 67 (46%a) | 19.64% | 0.08 |
The total VTE assessments completed pre- and post-EPR implementation increased from 96% to 97% respectively, p=0.39; majority of which were completed correctly with 95% pre-EPR implementation and 94% post-EPR implementation, p=0.40.
62% of the total patients had a 24-h reassessment completed pre-EPR implementation when compared to 54% post-EPR implementation, p=0.08. Similar to the initial assessment, most 24-h reassessments were completed correctly with 96% pre-EPR implementation and 95% post-EPR implementation, p=0.08. Patients who had no reason for not having a 24-h reassessment completed increased significantly from 57% to 70% pre- and post-EPR implementation respectively, p=0.02.
EPR: Electronic Patient Record; VTE: Venous Thromboembolism; n: number.
p-Value<0.05 was considered significant.
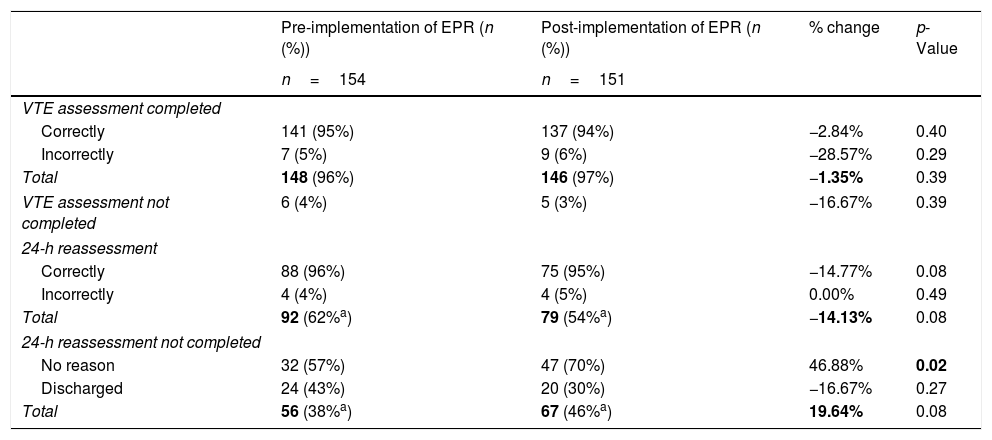
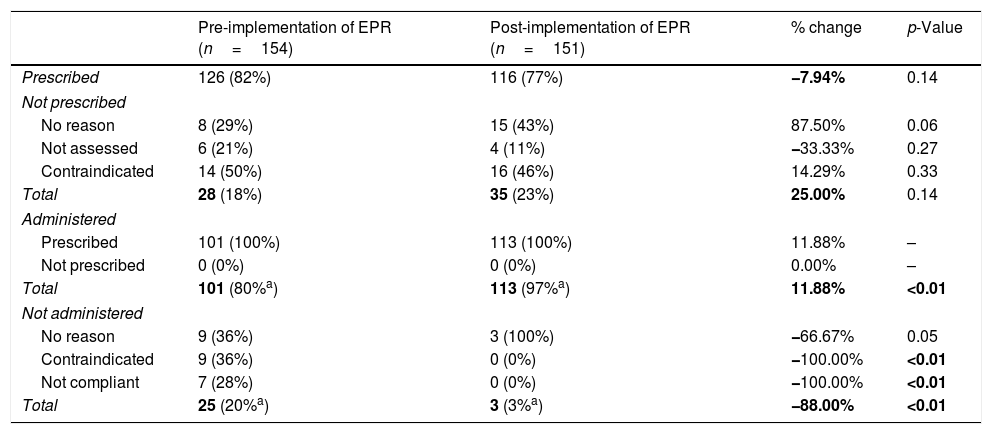
Prescription and administration of LMWH in pre- and post-EPR implementation populations.
| Pre-implementation of EPR (n=154) | Post-implementation of EPR (n=151) | % change | p-Value | |
|---|---|---|---|---|
| Prescribed | 126 (82%) | 116 (77%) | −7.94% | 0.14 |
| Not prescribed | ||||
| No reason | 8 (29%) | 15 (43%) | 87.50% | 0.06 |
| Not assessed | 6 (21%) | 4 (11%) | −33.33% | 0.27 |
| Contraindicated | 14 (50%) | 16 (46%) | 14.29% | 0.33 |
| Total | 28 (18%) | 35 (23%) | 25.00% | 0.14 |
| Administered | ||||
| Prescribed | 101 (100%) | 113 (100%) | 11.88% | – |
| Not prescribed | 0 (0%) | 0 (0%) | 0.00% | – |
| Total | 101 (80%a) | 113 (97%a) | 11.88% | <0.01 |
| Not administered | ||||
| No reason | 9 (36%) | 3 (100%) | −66.67% | 0.05 |
| Contraindicated | 9 (36%) | 0 (0%) | −100.00% | <0.01 |
| Not compliant | 7 (28%) | 0 (0%) | −100.00% | <0.01 |
| Total | 25 (20%a) | 3 (3%a) | −88.00% | <0.01 |
The total LMWH prescriptions decreased from 82% to 77% pre- and post-EPR implementation respectively, p=0.14. Of the patients not prescribed LMWH (18% pre-EPR and 23% post-EPR implementation, p=0.14), 50% compared to 46% were due to contraindications pre- and post-EPR implementation respectively, p=0.33. The remainder of patients with missing prescriptions were due to a lack of an assessment (p=0.27) or no documented reason (p=0.06).
Of those prescribed LMWH, 80% were given the prescription pre-EPR implementation compared to 97% post-EPR implementation, a significant increase with p<0.01. 100% of patients given LMWH were prescribed it pre- and post-EPR implementation. Of those not given the LMWH prescription (20% pre-EPR and 3% post-EPR implementation, p<0.01), 36% were due to contraindications pre-EPR compared to 0% post-EPR implementation, p<0.01. The remainder of those who were not administered were due to lack of compliance (p<0.01) or for no documented reason (p=0.05).
EPR: Electronic Patient Record; n: number.
p-Value<0.05 was considered significant.
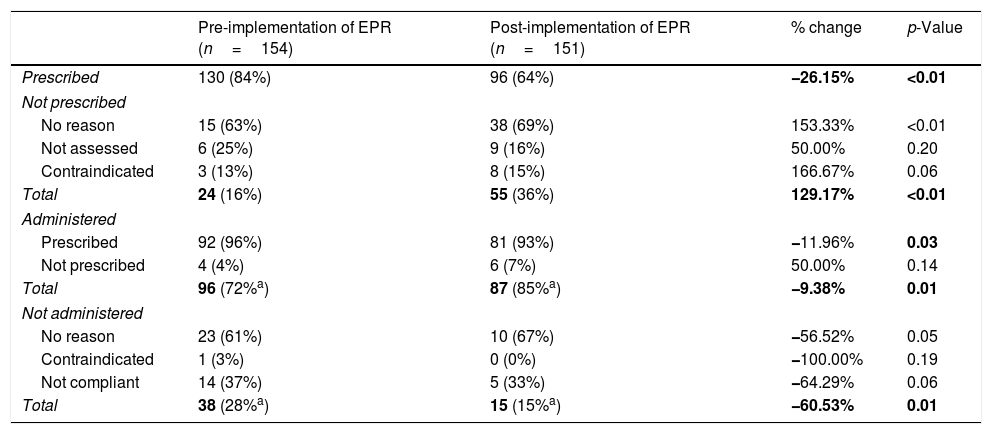
Prescription and administration of TED stockings in pre- and post-EPR implementation populations.
| Pre-implementation of EPR (n=154) | Post-implementation of EPR (n=151) | % change | p-Value | |
|---|---|---|---|---|
| Prescribed | 130 (84%) | 96 (64%) | −26.15% | <0.01 |
| Not prescribed | ||||
| No reason | 15 (63%) | 38 (69%) | 153.33% | <0.01 |
| Not assessed | 6 (25%) | 9 (16%) | 50.00% | 0.20 |
| Contraindicated | 3 (13%) | 8 (15%) | 166.67% | 0.06 |
| Total | 24 (16%) | 55 (36%) | 129.17% | <0.01 |
| Administered | ||||
| Prescribed | 92 (96%) | 81 (93%) | −11.96% | 0.03 |
| Not prescribed | 4 (4%) | 6 (7%) | 50.00% | 0.14 |
| Total | 96 (72%a) | 87 (85%a) | −9.38% | 0.01 |
| Not administered | ||||
| No reason | 23 (61%) | 10 (67%) | −56.52% | 0.05 |
| Contraindicated | 1 (3%) | 0 (0%) | −100.00% | 0.19 |
| Not compliant | 14 (37%) | 5 (33%) | −64.29% | 0.06 |
| Total | 38 (28%a) | 15 (15%a) | −60.53% | 0.01 |
The total TED stocking prescriptions decreased significantly from 84% to 64% pre- and post-EPR implementation respectively, p<0.01. Of the patients not prescribed TED stockings (16% pre-EPR and 36% post-EPR implementation, p<0.01), 13% compared to 15% were due to contraindications pre- and post-EPR implementation respectively, p=0.06. The remainder of patients with missing prescriptions were due to a lack of an assessment (p=0.20) or no documented reason (p<0.01).
Of those prescribed TED stockings, 72% were given the prescription pre-EPR implementation compared to 85% post-EPR implementation, a significant increase with p=0.01. Of the patients given TED stockings, 96% had a prescription for them pre-EPR implementation compared to 93% post-EPR implementation, p=0.03. Of those not given TED stockings (28% pre-EPR and 15% post-EPR implementation, p=0.01), 3% were due to contraindications pre-EPR implementation compared to 0% post-EPR implementation, p=0.19. The remainder of those who were not administered was due to a lack of compliance (p=0.06) or for no documented reason (p=0.05).
EPR: Electronic Patient Record; n: number.
p-Value<0.05 was considered significant.
This study aimed to explore the effects of converting to EPR from paper records on the adherence to NICE thromboprophylaxis guidelines in a tertiary centre hospital. As the NHS moves towards paperless technology,7 it is vital to ensure the quality of care and patient safety is not compromised.
Using paper records, the trust met the national target set out in the NHS Standard Contract 2019/2020 at a 96% completion rate of VTE assessments, which increased to 97% post-EPR implementation (p=0.39). This rise is not statistically significant, demonstrating that EPR is not inferior to paper records and therefore has not interfered in assessment completion. This VTE risk assessment completion rate compares similarly to a study conducted at SGH NHS Trust in 2014,8 which reported a completion rate of up to 98% using paper records, demonstrating the department has been consistently meeting assessment targets. The study also assessed whether risk assessment forms were completed correctly or not. The data shows no statistically significant difference between paper (5% completed incorrectly) and electronic records (6% completed incorrectly) (p=0.29), agreeing with the results of this study.
As per local guidelines, VTE risk is re-assessed at 24hours post-admission. The pre-EPR completion rate was 62%, falling to 54% post-EPR. This was unexpected as it was hypothesised that prompts and alerts on the EPR system would remind staff to complete 24-h re-assessments. However, 24-h re-assessment forms are not mandatory, allowing staff to dismiss alerts. Additionally, as data collection was conducted shortly after EPR implementation, staff may have had limited training and were unfamiliar with the system. A similar pattern was found in the SGH 2014 study,8 with around 63–77% of 24-h re-assessments being completed correctly using paper records. A recommendation to improve these risk assessment completion rates is to develop the IT system training for new staff, run a “refresher” training session for existing staff on using the EPR system with emphasis on the importance of completing the 24-h VTE risk re-assessment for maintaining patient safety.
Overall, LMWH prescriptions decreased from 82% to 77% with the transition to electronic records, although this change is not statistically significant (p=0.14). In both paper and electronic records, 9–12% of patients were not prescribed LMWH due to a VTE risk assessment not performed or no reason stated. Similar results of low prescription rates of LMWH were found in other trusts, for example in a prospective study in 2005 showing similar trends for thromboprophylaxis prescriptions in two NHS teaching hospitals.9
All patients who were given LMWH, before and after EPR implementation, had completed prescriptions. This suggests that encouraging early assessment is key for ensuring completed prescriptions and avoids delaying VTE assessments. On the other hand, some patients were not given LMWH despite having a prescription; 25 patients pre-EPR and 3 patients post-EPR. Lack of record keeping, and compliance issues were prominent pre-EPR but reduced post-EPR. A mixed methods study in 2015 explored the benefits and challenges of EPR implementation within the NHS, noting a major benefit of EPR: enabling faster flows of information and increased efficiency of completing tasks.10 A UK based study conducted across 28 hospitals reported relatively high LMWH prescription rates and VTE risk assessment rates.11 This study also described that additional measures to further improve prescription rates are unlikely to be cost-effective.
Clarke et al. also described financial restraints and lack of time for electronic trust induction, hindering staff use of EPR. There is a difference across baseline technology capabilities between trusts, making it difficult for hospitals to achieve the same end-goal. Each trust instead needs to have their technological capabilities assessed, as each trust will have different needs and resources.12 These figures warrant further investigation into identifying the reasons for low LMWH prescription and missed assessments as there is a clear discrepancy between hospital performance and nationwide regulations.
As for mechanical methods, before the implementation of EPR 84% of patients were prescribed TED stockings, which dropped to 64% with the use of EPR (p<0.01). The data shows a worrying pattern of poor record keeping in the use of TEDs with both paper and electronic records. This demonstrates that EPR systems have non-inferiority to paper records in terms of TED prescriptions. Nevertheless, TED stockings are a non-pharmacological treatment method, and therefore may not have been straightforward to prescribe using the EPR system. Cambridge University Hospital12 also experienced troubles with consistency of care after their EPR system, Epic, was implemented. The Care Quality Commission inspection only made significant improvements in their record keeping two years after the implementation of EPR. Therefore, it is possible that the TED prescription rates fell due to a ‘productivity dip’.13 Possibly, staff were unfamiliar with the system or there may have been technological glitches in the software. While TEDs were often prescribed, data shows that they were not always administered, or TED stockings were sometimes not prescribed but still given to patients. TEDs administration (defined as the patient found wearing the TED stockings correctly) fell from 96% to 93% (p=0.03) with the transition to EPR. However, administration remained variable regardless of prescription rates, indicating the cause of low TEDs administration lies elsewhere to that of EPR. Five patients lacked compliance in wearing TEDs (post-implementation of EPR), but more often there was no reason stated in the notes as to why (67% of cases). Six patients were wearing TED stockings given by staff even though a prescription had not been completed on the system. This may be due to staff being unfamiliar with the new software or poorly trained record keeping, as well as being able to bypass prompts to fill out the forms fully. According to Restrepo P et al.,14 it is difficult to monitor proper TEDs use because of lack of clear guidelines and strong evidence. The transition to EPR is an enormous undertaking for a hospital, however the results demonstrate that this electronic system is not inferior to paper records and this process does not hinder patient safety.
This study did not assess the impact on how correctly VTE risk assessments were done (e.g. whether prophylaxis was correctly prescribed or whether the correct size TEDs were administered), and did not record patient's previous risks for VTE, such as use of combined oral contraceptive pill, past history of DVTs, active cancer, etc., which would be useful in making judgements on the appropriateness of prescriptions. Data was also not recorded on patients’ presenting complaint, diagnosis, scheduled operation, or length of bed rest pre- or post-op, which all have an impact on VTE risk. Staff attitude is also a key parameter in the success of sustainable change, and therefore would be useful to include in this study.
The main limitation of the study is that patients were only selected from the general surgery list and from one tertiary centre. This limits the applicability of the results to other departments and to larger geographic areas. In the future a larger sample size should be considered, making it easier to achieve statistical power within the results. Moreover, there was a difference in sex pre- and post-implementation of EPR (p=0.04). This could not be controlled for as this was a cross-sectional study observing all admitted patients between two time points which may have skewed the results. Future studies could include a larger sample size to attempt to correct for this. It is challenging to maintain consistently high standards of care during large transitions such as implementing EPR, especially with frequently rotating staff (e.g. junior doctors), which may have influenced the results. A multifactorial framework is required to achieve technological goals including enhancing staff attitude, increasing EPR training and assessments in individual trusts.
ConclusionsIt is evident that implementing EPR has not interfered with the completion of assessments and therefore is not an inferior method to using paper-records. Based on the outcomes of this study, EPR is an acceptable alternative and should not negatively impact trusts in achieving their national targets and subsequently be penalised. Further investigation should be conducted to identify the cause of a declining 24-h re-assessment rate after EPR implementation. There are clear discrepancies in administration of both LWMH and TED stockings, despite the fact that current practices at the tertiary centre in this study did meet the national guidelines. This clearly indicates need for further improvement. It is necessary to ensure that there is appropriate training in place for EPR use, as there are varied technological capabilities across trusts. This is particularly important in VTE prophylaxis as thrombotic events are preventable causes of death for in-patients.
FundingThis research did not receive any grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestNone.