The healthcare industry is nowadays increasingly forced to adapt to new fast-paced changes, despite its conservatism. Indeed, the number of new technology entrepreneurs and technology value is increasing. In this study, we use modern literature and illustrative cases to identify patterns of technological value creation in the healthcare industry with the purpose to form an understanding of the challenges and opportunities for technology entrepreneurs. Hence, we propose a new challenges-opportunities framework for understanding technology entrepreneurship (i.e., technology innovation, technology proactivity, and technology risk-taking) as a foundation for value creation concerning the needs of patients, medical personnel and hospitals, and the whole industry. We also end the article by outlining practical implications at the micro-level (i.e., patient advocacy and technology-enabled engagement strategies), meso-level (i.e., digital health solutions and motivation for collaboration), and macro-level (i.e., trust building and infrastructure).
The healthcare industry has been recently researched through the prism of various social sciences such as economics, organization studies, marketing, and others. However, despite this academic turmoil, many fields of study still appear fragmented and under-developed. Indeed, despite the increase in the number of technology applications in healthcare (Lee, 2019; Anema, Preston, Platz, & Unnithan, 2020), academic literature at the intersection between technology entrepreneurship and healthcare still requires systematization and further theorization (Medina-Garrido, Martínez-Fierro & Ruiz-Navarro, 2007; Zhao, 2008; Wang, Pan & Ray, 2021). Drawing on existing definitions (for overviews, see Bailetti, 2012; Ratinho, Harms & Walsh, 2015), we define technology entrepreneurship in healthcare as the process of building, launching, and scaling businesses that develop new technologies, products and services to create value for patients and the other stakeholders (e.g., personnel, hospitals, insurance companies). This may include developing apps and software, launching medical device companies, as well as creating new business models that leverage technology to improve patient care and reduce costs. Therefore, several features are specific to technology entrepreneurship: First, potential customers of healthcare services, such as physicians or patients, may not even assume that standard medical procedures or business processes can be performed in a new, atypical way (Tortorella, Saurin, Fogliatto, Rosa, Tonetto & Magrabi, 2020). The value of a new technology approach must be empirically proven; references from other markets are of little value in healthcare. Second, cost reduction is not the only factor in changing the traditional approach to a more technological one. Technology entrepreneurship can produce new value by bringing advantages to disabled customers who previously could come to terms with the impossibility of a fulfilling life. Third, technology entrepreneurship directly influences the life quality of people by for instance decreasing incidence rates, helping invent previously inaccessible medicine, and improving rehabilitation processes.
The healthcare industry is undergoing significant changes associated with high demand from society, tightening legislation in the industry, and a greater supply of medical services. Although there is a need to provide high-quality services focusing on a particular patient (Mathur & Sutton, 2017; Tarkkala, Helén & Snell, 2019), medical personnel suffer from an increased and unpredictable workload due to the influx of patients (Chaudhry, Yarrow, Aldossari & Waterson, 2021). State regulatory and supervisory organizations require transparency in providing services, increasing accountability for medical actions. Companies offering medical products and solutions strive to bring novelties to the market as soon as possible in an increasingly competitive environment, while countries constantly increase funding for national health systems. However, many researchers and practitioners confirm that technology can be the next step in changing the traditional healthcare industry, which can effectively respond to current and future challenges (Tortorella et al., 2021; Lee & Yoon, 2021; Kulkova et al., 2023). By their deep understanding of the healthcare industry, the technology they are leveraging, and the regulatory environment they will operate in, technology entrepreneurs can respond faster to new challenges with increased scalability and flexibility in service delivery.
Modern healthcare also faces new challenges that are difficult to foresee. For example, the COVID-19 pandemic has posed additional challenges for society (Strang, 2021; Torkkeli, Ivanova-Gongne, Vuorio & Kulkov, 2021), while technology entrepreneurs have responded more successfully to new circumstances. The healthcare industry has seen the accelerated adoption of 5G communications (Alshammari et al., 2021), telemedicine (Nyame-Asiamah, 2020), and robotic services (Kaiser, Al Mamun, Mahmud & Tania, 2020), and changed established supply systems (Mollenkopf, Ozanne & Stolze, 2021) that open up new opportunities in the industry. New opportunities for patients and medical personnel include tracking the spread of the disease, conducting automatic screening, and receiving recommendations in case of illness (Khan, Siddique & Lee, 2020; Spece, 2021). Although COVID-19 has negatively affected many industries, tech entrepreneurs have filled many healthcare niches. We see a gap in the existing literature in a holistic understanding of exactly how technologies help overcome challenges and open up opportunities for entrepreneurs in the healthcare industry. Most of the research related to technology entrepreneurship in healthcare comes down to describing successful practices in individual cases, such as companies offering new services, hospitals integrating new solutions into their work, or countries succeeding in a particular area of healthcare (Magistretti, Dell'Era & Petruzzelli, 2019). Meeting the demand for high-quality and affordable healthcare is primarily driven by innovation. Moreover, technology entrepreneurs offer most of the proposed innovations in healthcare, conveying their value to the customer in a highly competitive environment (Guo & Li, 2018).
Our study's main aim is in developing a new theoretical framework based on analyzing the interaction of key market stakeholders (patients, medical personnel, and the industry in general) with the key characteristics of technology entrepreneurship (technology innovation, technology proactivity, and technology risk-taking) (Ratten, 2010; 2011). Therefore, we pose the following question: What healthcare challenges and opportunities exist for technology entrepreneurs to generate value for stakeholders? As an objective, we use a method combining literature review and illustrative cases from contemporary healthcare industry practices supporting our findings (Hardman, Sprung & Weingarten, 2019).
The remainder of this paper is organized as follows: the next section provides an overview of technology entrepreneurship in healthcare by leveraging three key dimensions of entrepreneurship, i.e., innovation, proactivity, and risk-taking. The following section illustrates the challenges and opportunities underlying value creation processes associated with the stakeholders identified at the micro-, meso-, and macro-levels. In the final part of our article, we develop a framework that combines the three levels with the three dimensions of technology entrepreneurship, discussing theoretical and practical implications, and avenues for future research.
Technology entrepreneurship in healthcareAccording to the works of Holt, Rutherford and Clohessy (2007) and Ratten (2010; 2011) entrepreneurship's key characteristics are innovation, proactivity, and risk-taking. In the following section, each characteristic will be discussed further with corresponding examples from the healthcare industry.
Technology innovationTechnology innovation is the process of designing, creating, and implementing new or improved technologies to solve problems or improve existing processes. In healthcare, technology innovations include all products and services aimed at improving medical services, reducing costs, and streamlining procedures (Hardeman & Kahn, 2020; Shen, Wang & Yang, 2020) for the prevention, diagnosis, treatment, and recovery of patients (Burns, 2012). Most of today's innovations in healthcare are, to some extent, related to the increased computing power of IT resources that can assist a human if necessary (Lu, 2016). Examples of technology innovation in healthcare include Electronic Health Records, e-prescribing, and telemedicine. Electronic Health Records has been upgraded over recent years to become more efficient, secure, and user-friendly (Kim, Rubinstein, Nead, Wojcieszynski, Gabriel & Warner 2019). It now allows for more comprehensive patient data to be stored for easier access, improved communication between healthcare providers, and better patient outcomes. Additionally, the system has been upgraded with advanced analytics to help providers better monitor, manage, and diagnose patient conditions (Juhn & Liu, 2020). By utilizing e-prescribing, doctors can quickly and easily send prescriptions to pharmacies electronically, saving time and eliminating the need for paper prescriptions (Aldughayfiq & Sampalli, 2021). This technology has improved over the years, with more advanced features such as the ability to check for drug interactions, access medical history, and generate refill reminders. Telemedicine has been used for decades, but it has been continuously improved to provide more efficient and secure methods of delivering healthcare services to patients (Loeb, Rao, Ficke, Morris, Riley III & Levin, 2020). Recent improvements have included the development of secure video conferencing platforms, the introduction of artificial intelligence to aid in diagnoses and treatments, and the ability to store and transmit medical data securely.
Modern academic literature raises numerous questions for researchers and practitioners regarding the application of technological innovations. First, there are concerns about the security and confidentiality of the data collected, stored, and processed (Hathaliya & Tanwar, 2020). Second, medical personnel harbors resistance to automating traditional medical procedures (Monllau, 2019). Third, the complexity of modern medical technology requires combining knowledge and skills from different areas (Yu, Beam & Kohane, 2018).
In turn, numerous small and medium companies and large corporations shape innovation in the healthcare technology sector. Companies seek to discover, take, or form a new niche through unique knowledge (Skica, Mroczek & Leśniowska-Gontarz, 2019). For example, computer modeling and Big Data methods make finding candidates for substance molecules for drug development (Mak & Pichika, 2019). Large companies greatly emphasize search-based forecasting and determine relationships between unstructured data. Modern solutions such as IBM Watson are involved in drug development, financial tracking, fraud detection, and recommendations for healthcare management (Magistretti et al., 2019). The formation of new markets and niches is inextricably linked with providing access to new data that was unavailable or unprocessed. Trust between market participants and society is vital in technological development and the applicability of results in practice (Ferranti, Langman, Tanaka, McCall & Ahmad, 2010; Hathaliya et al., 2020). Tencent is testing its AI-based disease screening solutions in over 100 clinics in China. Although continuous training and fine-tuning solutions can increase the accuracy of a diagnostic evaluation, the automated system has already processed tens of millions of images and helped millions of people. The state's increased interest in successful technological innovations has also attracted additional private investment in the healthcare market (He, Baxter, Xu, Xu, Zhou & Zhang, 2019).
Technological innovations have become part of medical personnel's daily routine from the start of training. These innovations are relevant in supporting their knowledge and skills throughout their careers. Students can study using virtual and augmented reality, surgeons can prepare for surgery and receive 3D data previously inaccessible, robots can perform operations with the remote support of the surgeon (Zemmar, Lozano & Nelson, 2020), artificial coaches can facilitate the learning of new skills (Kulkov, Berggren, Hellström & Wikström, 2021), etc. The COVID-19 pandemic impacted the training and education of professional medical personnel, and now, medical education organizations offer distance education methods. The significant advantages of these technological innovations in training include a convenient and individualized training schedule, controlled intensity, and the ability to communicate with a physical or digital mentor (He et al., 2019). However, one disadvantage is decreased communication between students and the reliability of assessment activities (Shelgikar, 2020).
Technology proactivityTechnology proactivity is a technology-based activity that identifies and resolves problems before they occur (García-Morales, Ruiz-Moreno & Llorens-Montes, 2007). In the healthcare industry, technology proactivity can support the use of technology to anticipate, prepare for, and respond to emerging healthcare needs. It involves collecting data on emerging health trends, identifying potential risks, and creating new strategies to address them. Examples of technology proactivity in healthcare include predictive analytics, early detection of disease, and healthcare automation. The goal of proactive technologies in healthcare is to preserve the population's health, identify personal medical deviations, and form forecasts at an individual or societal level (Liao & Tsai, 2019). Proactive medicine involves investment in the stages of prevention, diagnosis, and detection of disease when expensive health system resources are most often unrequired.
Technology-based proactive medicine targets change in human behavior to change unhealthy behavior and support behavior change. People without adequate support can significantly damage their bodies, be frequently hospitalized, and die (Hixon, 2015). Not all patients have the necessary desire and willpower to make vital changes. In such cases, technology solutions can help, as they base their recommendations on constant feedback and personalization, offering recommendations at the right time. Measured indicators such as heart rate, activity level, and so forth are instantly transmitted to the attending physician or automatically tracked by the technology solution. Such indicators can become the basis for predicting health changes.
Technology proactivity can also promote more sustainable healthcare strategies by supporting hospitals in developing new approaches to service delivery that stand the test of time, are financially comprehensive, and assist the environment (Kyriakarakos & Dounis, 2020). The introduction of successful practices of sustainable technologies in healthcare forms favorable outcomes for future generations. Social technology entrepreneurship affects the principles of working with market participants and internal and external resources and finds maximum resonance in healthcare due to its close association with solving medical challenges (Amini, Arasti & Bagheri, 2018).
Technology risk-takingTechnology risk-taking refers to entrepreneurial behavior resulting in possible profit by taking financial risks associated with technology development and application. According to the academic literature available, the following key healthcare technological risks have been identified. First is the potential for patient injury or death when using the device or technology. Companies are responsible for the functioning of equipment and software due to design, manufacturing features, and possible incorrect use by medical personnel or the patient. The equipment may be unable to transfer changes in the patient's condition, resulting in a status change and possible legal fees. Second, health-critical technological products should be delivered completely ready and debugged, minimizing the possibility of additional adjustment and calibration (Sittig & Singh, 2010). Such information is critical not only for the patient and physician but other industry stakeholders. For example, an insurance company may provide discounts if a patient uses technology equipment. In the case of an error, the company may suffer financial losses because of data manipulation. Third, cyberattacks can impact sensitive medical data (Owens, 2020). If the fraudsters are successful, the technology company may incur financial, reputational, and organizational risks: Thus, due to such illegal actions, user data can be sold to third parties, the equipment used can be reconfigured without notifying users, and so forth.
Risky activities are inherent in entrepreneurs. However, risk-taking in healthcare affects not only technology entrepreneurs but other stakeholders. Physicians take a risk by agreeing to test new equipment or services (Borycki, 2015). Patients accept risks if the potential value outweighs the potential damage to health or other solutions have not shown a significant result (Schneider, Ridgely, Meeker, Hunter, Khodyakov & Rudin, 2014). Hospitals can incur reputational and other risks if cannot do their job due to being unprepared. These individuals and companies take risks when interacting with technology entrepreneurs and introducing new solutions to everyday work circumstances. Behind all healthcare industry stakeholders are people with varying levels of risk tolerance. The willingness to take risks and responsibility for decisions in such a mature industry as healthcare imposes its characteristics on entrepreneurs and stakeholders who offer or consume new products. The trust between industry stakeholders is formed through experience, skills, position in the professional community, recommendations, and so forth (Ferranti et al., 2010).
From the perspective of technology entrepreneurs, there are business, innovation, and social risks in healthcare. Business risks are often associated with start-ups and small companies, where the likelihood of failure greatly outweighs the likelihood of success. Technologies have become the basis of pharma companies (Chan, Shan, Dahoun, Vogel & Yuan, 2019). Large companies seek to reduce these costs by partnering with small technology companies that are more active in taking such risks. Regulatory bodies impose added restrictions closely monitoring the development, testing, and production of medical products and services. In most cases, entry into the markets of new countries is associated with the need to re-register and adapt to local rules and practices (Festa, Safraou, Cuomo & Solima, 2018). Innovation risks are related to the unavailability of the innovation infrastructure, lack of demand for proposed solutions, and mistakes in innovation management (Galende, 2006). Such risks can be divided into internal ones, such as a problem with the team or invention, as well as external ones beyond the technology entrepreneur's control, such as changes in legislation or the creation of required infrastructure. In turn, social risk is associated with the human factor and is a constant and unavoidable component of technology entrepreneurship (Matty et al., 2021). A patient may refuse to use a new solution, not because of design or functional limitations but because of personal characteristics, including the desire for personal meetings with the physician (especially among the older generation), the need for social interaction, empathy from a professional in a white coat, and so on (Peterlin, Dimovski & Bogataj, 2021).
Technology value creation in healthcareIn the following section, we illustrate the challenges and opportunities underlying value creation processes at the micro- (i.e., patients), meso- (medical personnel and hospitals), and macro-levels (industry).
Challenges and opportunities at the micro-levelTechnology entrepreneurship is associated by definition to the process of building, launching, and scaling businesses that develop new technologies, products, and services to create value for patients (Bailetti, 2012; Ratinho et al., 2015). Large tech companies such as Google create health value by collecting parameters throughout lives, subsequently forecasting long-term trends in changes at the micro-level. However, technology companies have recently created value in this market, for example, Kinsa Health or CardioQVARK, which are not inferior to giants in their niche. Moreover, technology entrepreneurs can evaluate the resulting parameters based on different population groups and cross-country differences, that is, comparing micro-level indicators in different populations. Due to machine learning methods, predicting the development of the patient's disease or identifying a trend towards an increased risk of illness for a specific population group in three to five years becomes possible. The best technology-created value in healthcare is determined by interconnecting solutions horizontally at the city or regional level and vertically at the interregional level with the involvement of industry regulators.
Researchers and entrepreneurs consider technology a way to increase value through patients’ involvement in their diagnosis, treatment, and recovery. First, physicians may recommend patients use mobile apps and wearables (Milner et al., 2021). Thus, representatives of the meso-level of healthcare (including medical personnel and hospitals) influence the changes taking place at the micro-level. Many companies of varying sizes produce wearable medical devices with artificial intelligence (AI) support. For example, California-based Eko produces advanced heart monitors with AI software while the well-known Ava from Swissland works with fertility parameters. Studies show that such solutions change behavior at the micro-level and encourage patients to think more about their health status, modify their lifestyle, and reduce the risk of developing the disease (Marahrens et al., 2017). Second, IT solutions allow remote assessment of the patient's condition based on symptoms at the micro-level and recommend emergency care or a regular visit to the physician thereby bringing changes to the industry at the meso- and macro-level. Strados Labs’ solution allows monitoring respiratory patients’ status using wearable sensors and advanced software. Moreover, a physician could be found in the nearest location or online consultation with the most suitable specialist could be offered, such as through a Zocdoc platform. Third, treating chronic disease involves monitoring routine activities that must be followed. The Canadian-based company, CareClinic or Pathmate, a spin-off from ETH Zurich, offers this. Training and required reminders could be tracked using software and hardware customized solutions and assess treatment progress (Bahl, Singh, Javaid, Khan, Vaishya & Suman, 2020). Thus, changes occur at the micro- and meso-levels of the industry. Fourth, technology solutions for monitoring treatment are becoming more common: namely, finding medicine and information about it, sending reminders to take medication, and involving additional participants, such as relatives and others. These activities impact treatment costs and the burden on the whole healthcare system. Small Finnish company Peilli offers its virtual reality equipment and software to be used on an outpatient basis, with the help of relatives, to help patients recover from strokes or occupational injuries. This increases the number of sessions and changes the traditional physician-patient approach. Forming value based on technology solutions fits optimally into the coordinate system based on patient-centered care at the macro-level (Eklund et al., 2019). Technology entrepreneurship is the engine of social change. New technologies make changing patients’ and improving their quality of life possible. People with disabilities and elderly patients gain access to an active life. Technology solutions such as the SignBook or Accessible Jordan can describe the state of the environment, adding new capabilities for people with disabilities.
Challenges and opportunities at the meso-levelHealthcare places high demands on people who have trained for work for a long time and are continuously required to improve their skills. The demands placed on technology and infrastructure are also always increasing creating prerequisites that challenge medical personnel's current expertise and encourage hospitals’ adoption of new practices and processes. The technological solution SurgeryVision is integrated into Finnish students’ curriculum by offering the viewer MRI/CT images in stereoscopic 3D format for accelerated human anatomy education and abnormality detection. Swedish Alteruna combines virtual reality and AI to train surgeons in new surgical techniques. Combining physical and haptic virtual objects with the possibility of group training lends greater involvement and preparedness for future work. Robocath offers physicians the option to perform remote surgery without being physically near the patient. Such technology companies overcome key limitations associated with location, lack of qualified assistance in remote regions, and high costs which are the main limitations at the macro-level (Marescaux & Rubino, 2004).
Developed countries prioritize using new technologies in healthcare while developing countries can significantly improve the state of the industry. Developing countries can gain access to quality medicine by skipping the industry stages they previously experienced. This niche is especially highlighted by Byon8, a developer of AI and virtual reality technology solutions from Stockholm that targets developing countries. Telemedicine, remote communication, training, decision support, and other areas of value creation are in great demand from developing and developed countries at the macro-level.
Remote medicine (telemedicine) makes getting expert consultation faster than classical methods and increases hospitals’ capacity (Hjelm, 2005) which affects the standard procedures of the meso-level. COVID-19 has given a powerful impetus to telemedicine development. With telemedicine's help patients and medical personnel have reduced the likelihood and spread of infection (Portnoy, Waller & Elliott, 2020). Telemedicine's most popular offerings are dedicated streaming platforms such as Lumed or Amwell which offer a complete suite of hardware, software, and support to connect patients and healthcare professionals.
Another change at the meso-level is that the absence of a narrow-profile specialist could replace a general practitioner with the support of decision-supporting algorithms based on machine learning. Remedy Health offers decision-making support to non-healthcare workers in identifying hidden and chronic conditions. Nursing staff may be more focused on communicating with the patient, while data collection and condition tracking is shifting towards technology solutions accompanying the patient. Babylon offers an application for self-diagnosing diseases. This AI solution allows you to check symptoms and reduce medical errors. Remotely servicing equipment or reducing repair time with technology solutions improves operational efficiency and reduces equipment downtime, see cases of XMReality from Sweden and Delta Cygni Labs from Finland.
Challenges and opportunities at the macro-levelEvaluating Big Data, analyzing unstructured information, and identifying intangible trends open up new opportunities for the healthcare industry at the macro-level. It is increasingly becoming apparent to industry stakeholders that data is a new resource and value in the industry. Large companies such as Roche and Pfizer, with experience and a long history, digitize their activities’ results, forming a knowledge base for their needs and the entire industry at the macro-level. However, companies may not have a clear purpose for this knowledge and may offer it to the market. Small companies find such a resource as the ability to build a business with access to data, creating a shared value (Kulkov, 2021). How such information is processed builds a company's business model. Access to prepared and cleaned data is an essential resource for technology entrepreneurs generating value at all three levels. However, most business representatives are suspicious of information collected by other companies. Trust and reputation in the healthcare industry are the most crucial factors influencing technology value formation (Ferranti et al., 2010).
Value creation is an essential prerequisite for a technology entrepreneur's success. The value creation strategy for a technology solution in healthcare is selected individually. However, such a strategy must generally follow certain principles that reflect the industry logics. However, the more disruptive a new healthcare solution is, the greater the industrial barriers that technology companies must overcome. In the case of a niche formation, involving other participants in the acceptance procedure, such as insurance companies for payment and research laboratories for testing, is necessary.
The lack of proper infrastructure for integrating and using technologies is one key constraint on developing at the macro-level. Security and trust issues (Hathaliya et al., 2020), insufficient integration of solutions into work procedures (Knickerbocker et al., 2018), and product selection for integration are the main components. Stand-alone solutions have been integrated and tested to a significant extent to provide a meaningful reference for others. However, there is no single proven standard that should be adhered to when developing technologies for health needs. Other researchers also point to the specific risks inherent at the meso- and macro-levels. First is the need for long-term testing and obtaining the necessary certificates before market launch (Hamburg, 2010). The probability of failure or the formation of an unsuccessful solution, which will not surpass analogs and classical solutions in its parameters, is high. Second, technology solutions in the healthcare industry require significant investments and a vast network for marketing, testing, and integrating solutions. Investors may consider the healthcare market high-risk, albeit with a potentially substantial return. Third, the conservatism and distrust of market participants can contribute to new technology solutions. Medical personnel may fear losing patients and the patient's need for the healthcare system, patients may be concerned about incorrectly working equipment and express the desire to continue treatment in person with a physician instead of applications, and the hospital's administration jeopardizes its reputation if it agrees to participate in testing and implementing untested technology solutions (Durán & Jongsma, 2021).
Challenges and opportunities of healthcare technology entrepreneurship: implications and avenues for future researchThe article's key contribution is the study of various aspects of innovation and knowledge (Alshanty & Emeagwali, 2019; Camisón-Haba, Clemente-Almendros & Gonzalez-Cruz, 2019; Ferreira, Fernandes & Kraus, 2019; Piñeiro-Chousa, López-Cabarcos, Romero-Castro & Pérez-Pico, 2020; De Bernardi, Bertello, Forliano & Orlandi, 2022) applied to the healthcare industry. In particular, this article aims to examine various aspects of technology entrepreneurship and, more specifically, how technology entrepreneurship forms a value framework for understanding value creation processes in the healthcare industry. Based on this premise, the current state of technology entrepreneurship in healthcare has been analyzed and linked to a multi-level challenges-opportunities framework.
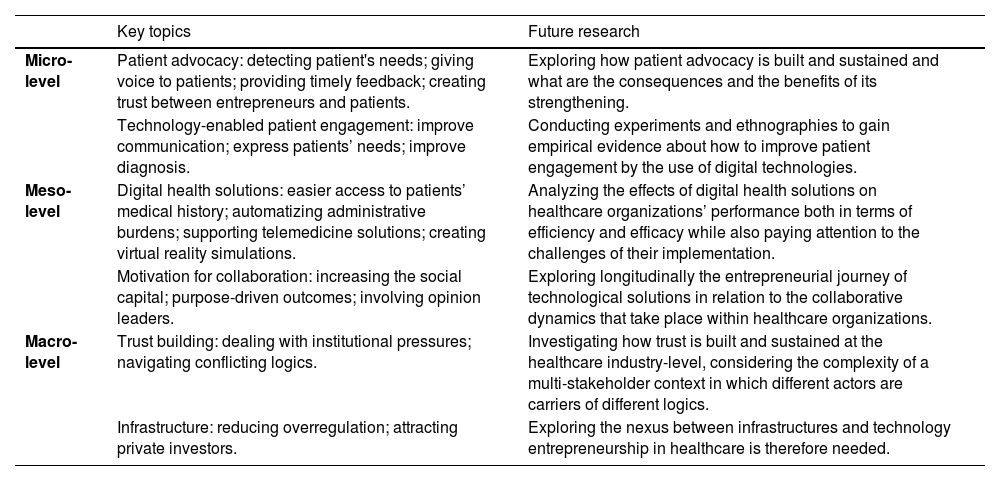
Table 1 introduces our framework, discussed in this paragraph in light of its theoretical and practical implications.
Challenges and opportunities of healthcare technology entrepreneurship
| Technology innovation | Technology proactivity | Technology risk-taking | ||||
|---|---|---|---|---|---|---|
| Challenges | Opportunities | Challenges | Opportunities | Challenges | Opportunities | |
| Micro level | Low awareness; Refusal of automatized medical services. | Co-creation of services in close interaction with patients. | Disrupt patients’ lives; Underestimation of patients’ needs. | Projecting long-term changes in health status; Promoting incremental rather than disruptive behavior changes; Preventive medicine. | Individual preferences influence risk perception. | Cooperating with industry professionals at the stage of development, testing and integration; Developing and standardizing protocols. |
| Meso level | Resisting new technology solutions; Increasing qualification requirements. | Trust based on evidence; Improved work efficiency, reduced workload; Development of professional skills throughout a career. | Reputational risk. | Counterbalance lack of medical personnel; Support decisions with large dataset; Reeduce the workload. | Machines replacing medicall personnel. | Co-creating value with risk-tolerant stakeholders; Optimizing decisions. |
| Macro level | Complexity of products. | Collective knowledge; Data is the new source for the industry. | Institutional voids in emerging markets. | Providing sustainable strategies for the industry development; Institutional work and the emergence of niche markets. | Unplanned access to medical data by third parties | Attracting risk averse investors. |
Technology innovation in healthcare refers to the process of designing and/or implementing new or improved technologies to address patients’ needs. Indeed, when developing an entirely new technology solution that was previously unavailable for the market, a technological entrepreneur can target not only the usual B2B market but B2C, addressing the patient directly. This new strategy provides renewed marketing channels, while its proven effectiveness will allow the technology entrepreneur to certify and use the classic promotional methods in the healthcare market. However, patients might not be aware, or even scared, by the disruptiveness of new technological solutions that promote new, unknown medical procedures and health practices. The medical staff sometimes likewise distrusts new technology opportunities partly due to a lack of experience and familiarity with new technological innovations. Short trial periods may reveal crucial for the medical personnel to realize the value and adapt to technological solutions such as digital work assistants. However, technology entrepreneurs should constantly demonstrate competence, as mistakes at this stage can demotivate health organizations from collaboration, depriving a future project from occurring. In turn, the incredible complexity of manufactured technological solutions, most of which are at the intersection of several fields of knowledge, requires advanced skills from collaborators (Yu et al., 2018).
At the industry-level, the accumulation of big medical data is becoming the foundation to co-create value and collective knowledge. Organizations of different sizes contribute in different ways to the generation of big data. Moreover, large companies shift the risks of developing solutions early on to small companies. Conversely, large companies form their digital knowledge bases, which are in demand with small technology companies (Kulkov, 2021).
Technology proactivity is associated with a significant lack of confidence in new solutions at the macro-level and the presence of institutional voids (Durán et al., 2021). Technology solutions providing decision support to specialists or affecting the patient's behavior are rapidly spreading (Shortliffe & Sepúlveda, 2018). Applications interacting with patients at the micro-level by collecting and processing data are booming. The data collected can also support the implementation of preventive medicine, which is essential to spur proactive entrepreneurial approaches and to encourage incremental rather than disruptive behavior changes in patients. Moreover, the aggregated data of many customers at the micro-level could become the basis for long-term trends in developing societies as well as for the emergence of niche markets (Kulkov, Tsvetkova & Ivanova-Gongne, 2021). The technology value created proactively will positively impact the availability of medical services in poorly developed regions, developing countries, and remote places, namely the development of the macro-level in a particular country. Technology entrepreneurs create value for health organizations by overcoming the challenges associated with a lack of medical personnel, excessive workload, and inefficient use of working time. Overall, the industry receives many opportunities for proactive value creation from technology entrepreneurs. We have identified sustainable strategies for companies, specialist support, and remote medicine as key positives in how technology entrepreneurs interact with healthcare (Janssen & Moors, 2013; Kyriakarakos et al., 2020). On the other hand, however, health organizations adopting massively emerging technologies may be exposed to reputational risks in case this massive adoption is perceived as it was de-humanizing medical services. AI, for instance, can assist specialists with the diagnosis of many diseases, predict genetic mutations and prognosticate disease outcomes (Secinaro, Calandra, Secinaro, Muthurangu, & Biancone, 2021). However, the same technology has also been criticized for reproducing biases.
Technology risk-taking is the last category we explore as concerns challenges and opportunities for value creation in the healthcare industry. Risk perception in healthcare depends on individual attitudes and dispositions. The desire to be subjected to new, experimental treatments, the preference for recovery at home or in the hospital and other elements depend on people's risk perception (Marahrens et al., 2017). This perception can be mitigated by cooperating with industry professionals at the stage of development, testing and integration and by developing standardized protocols. However, risk-taking is not only related to individual preferences but also to the social capital developed at the organizational- and the industry-level (Ferranti et al., 2010; Jalali & Kaiser, 2018; Hathaliya et al., 2020). Trust between stakeholders usually grows with the experience of cooperation (Hathaliya et al., 2020). Conversely, disruptive technology solutions may suffer from a lack of infrastructure and require significant changes in industry-specific procedures. Resource-poor companies may not find their customers due to the complexity of developing, testing, and certifying a new promising technology solution (Davila, Foster & Jia, 2010). Some countries have chosen the healthcare industry as a priority for development and are investing heavily in this area. Simultaneously, private investors are likelier to choose the healthcare industry in the presence of public pressures for investment (Henstock, 2019) as well as most risk-averse investors can invest in more uncertain technologies.
In the eternal dispute between technophobes and technophiles (Griffy-Brown, Earp & Rosas, 2018; Bresciani, Dabić & Bertello, 2022), technology detractors also argue that technological solutions will replace medical personnel while technophiles highlight that the replacement will take place between personnel with technological solutions and personnel without technological solutions. Among the risks associated with emerging healthcare technologies, there is also one related to cybersecurity. When a huge amount of data is online, protecting electronic information and assets from unauthorized access, use and disclosure becomes vital for the normal functioning of organizations and the protection of patients’ health (Kruse, Frederick, Jacobson & Monticone, 2017).
Based on research results, we also identified several practical implications that might also pave the way for future areas of study.
Micro-level: patient advocacy and technology-enabled engagement strategiesPatient advocacy plays an important role in technology entrepreneurship as it helps ensure that technological solutions are developed with the needs of the patient in mind. It gives patients a voice to express their needs and provides input into the development of products and services. Advocates can also provide feedback to entrepreneurs on the usability and effectiveness of their products and services, ensuring that they meet the needs of the patients they are designed to serve. Furthermore, patient advocacy can help to create more innovative solutions by connecting entrepreneurs to resources, such as patient data and research, that can help inform their designs. This input can also help to create trust between entrepreneurs and the patient community, which is essential for any successful technology business.
Technology-enabled patient engagement strategies can have a positive impact on patient outcomes by helping to improve communication between patients and their healthcare providers, increasing patient access to care, and providing resources and tools to empower patients to take control of their health. Through improved communication, patients are better able to discuss their health concerns with their healthcare providers, potentially leading to better diagnosis and treatment. Additionally, technology-enabled patient engagement strategies can increase access to care by making it easier for patients to schedule and receive care. Finally, technology-enabled patient engagement strategies can provide patients with the tools and resources they need to take an active role in their health and make informed decisions about their care.
Meso-level: digital health solutions and motivation for collaborationTechnology can be used to create digital health solutions that allow hospitals to streamline and optimize patient care. For example, hospitals can use technology to develop EMRs that enable doctors and nurses to easily access and share a patient's medical history and current health status. Additionally, technology can help hospitals better manage their resources and reduce costs by automating administrative tasks, such as scheduling appointments, billing, managing insurance claims, and tracking performance metrics. Furthermore, hospitals can use technology to create telemedicine solutions that allow patients to connect with their doctors remotely and receive medical advice and treatment online. Finally, technology can be used to create virtual reality simulations that enable doctors and nurses to practice medical procedures in a safe and controlled environment.
Motivation for collaboration on a hospital level is an important area for research. Certainly, financial rewards, the transfer of company shares, and participation in the board of directors are well-researched areas (for example, Carboni & Cross, 2020). However, intangible assets can be just as crucial. Moreover, most technology entrepreneurs lack the resources to develop their projects, and hiring costly experts can be difficult for a company. Diffusing limited resources reduces the likelihood of project success. Even having interested a physician in a technology project, an entrepreneur is not protected from decreasing interest in the project and possible incompetence, among other factors, during project development and integration. During our study, the factors identified regarding the interest in and retention of medical personnel in the project were the social capital of a technology entrepreneur and solving the global problems of the industry. Another attraction may be working with opinion leaders in the healthcare industry, despite the pros and cons of such cooperation (Campbell & Farrell, 2020).
Macro-level: trust building and infrastructureBuilding trust among market participants is another topic of active academic study (Ferranti et al., 2010; Hathaliya et al., 2020). However, it is worth paying more attention to practical steps and concrete recommendations for technology entrepreneurs when working with healthcare industry representatives. Building trust among stakeholders in healthcare differs from the usual framework offered in a B2B context. The main parameter can be the difference in organizational and professional culture and beliefs in general. Trust between two companies with similar interests is based on shared interests, beliefs, motivations, and so on. However, external factors such as institutions and regulations are more important in healthcare.
A competitive healthcare industry also needs a sound infrastructure that benefits not just individual stakeholders but society in general. Society uses significant resources for equipment, infrastructure, and training medical personnel in the hopes of a return. The industry is interested in more supply from technology entrepreneurs. A large amount of scientific research remains within research laboratories and does not reach the market. Private investors may view the healthcare market as a challenge due to long payback periods, difficult certification, and more. Due to complexity and overregulation, entrepreneurs from other industries do not consider healthcare. Future research that explores how better infrastructure supports technology entrepreneurship in healthcare is therefore needed. (Table 2)
Research agenda
| Key topics | Future research | |
|---|---|---|
| Micro-level | Patient advocacy: detecting patient's needs; giving voice to patients; providing timely feedback; creating trust between entrepreneurs and patients. | Exploring how patient advocacy is built and sustained and what are the consequences and the benefits of its strengthening. |
| Technology-enabled patient engagement: improve communication; express patients’ needs; improve diagnosis. | Conducting experiments and ethnographies to gain empirical evidence about how to improve patient engagement by the use of digital technologies. | |
| Meso-level | Digital health solutions: easier access to patients’ medical history; automatizing administrative burdens; supporting telemedicine solutions; creating virtual reality simulations. | Analyzing the effects of digital health solutions on healthcare organizations’ performance both in terms of efficiency and efficacy while also paying attention to the challenges of their implementation. |
| Motivation for collaboration: increasing the social capital; purpose-driven outcomes; involving opinion leaders. | Exploring longitudinally the entrepreneurial journey of technological solutions in relation to the collaborative dynamics that take place within healthcare organizations. | |
| Macro-level | Trust building: dealing with institutional pressures; navigating conflicting logics. | Investigating how trust is built and sustained at the healthcare industry-level, considering the complexity of a multi-stakeholder context in which different actors are carriers of different logics. |
| Infrastructure: reducing overregulation; attracting private investors. | Exploring the nexus between infrastructures and technology entrepreneurship in healthcare is therefore needed. |
This research was partially sponsored by the Jenny and Antti Wihuri Foundation, Finland. This research was partially sponsored by the research center XPRES (Excellence in Production Research) – a strategic research area in Sweden. The paper is an output of the project NFP313011BWN6 “The implementation framework and business model of the Internet of Things, Industry 4.0 and smart transport”.