Among patients with coronavirus disease 2019 (COVID-19), thrombogenicity is a common abnormality. Due to this, the prophylactic application of low molecular weight heparin (LMWH) has been recommended by several expert consensus,1 as one of its most serious complications is the well-known heparin-induced thrombocytopaenia (HIT).2
Additionally, as recent publications have reported the presence of spontaneous HIT in critical patients affected by COVID-19 and naive for heparin,3 and that therefore a higher percentage and/or intensity than expected could lead to the presentation of said disorder, the objective of this study has been to quantify said incidence of HIT among patients affected by moderate or severe COVID-19.
For this, we have retrospectively analysed a cohort of COVID-19 patients (diagnosed by the polymerase chain reaction test or PCR), under prophylactic treatment with LMWH (bemiparin 2,500−3,500 IU Anti-Xa). They were consecutively admitted to the Hospital Real de Nuestra Señora de Gracia, internal medicine department, between 1 st February and 16th March 2020, with a platelet count every 3−5 days and baseline between 100 and 500 × 103/ mm3.
The final study sample was 43 patients: 51% male, age 73.5 (± 16.9), body mass index 27.4 (±4.7), procalcitonin 0.4 (±1.5) ng/mL, leukocytes 8.3 (±4.5) 103/mm3, glomerular filtration (CDK-EPI) 70.2 (±21.3) mL/min, prothrombin time 12.7 (±1.2) s, Clauss fibrinogen 611 (±151), ferritin 814 (±495) ng/mL and D-dimer 3995 (±7092) ng/mL; of which 42% were being treated with hydroxychloroquine and 35% with hydroxychloroquine and lopinavir + ritonavir; 17 had associated risk factors: 35% DM2, 64.7% arterial hypertension and 17.6% renal failure.
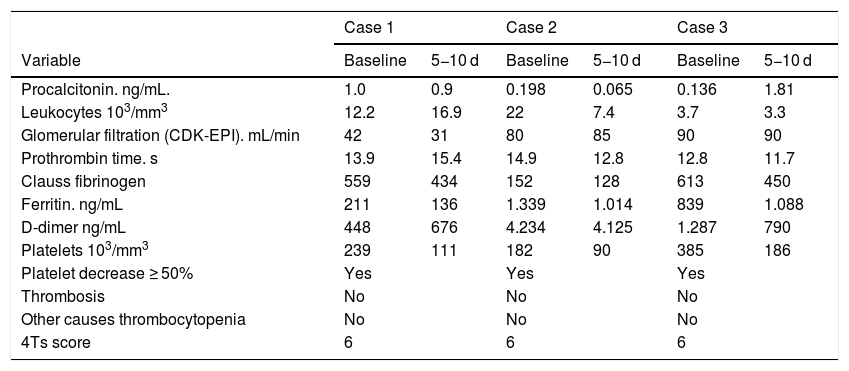
The results identified 3 patients (6.9% of the sample), all male and aged 45, 71 and 90 years, whose risk quantification of iatrogenic thrombocytopaenia obtained a value of 6, according to the 4 Ts scoring system.2 This meant they had a high probability of presenting HIT (Table 1). The incidence of HIT observed in our cohort (6.9%), although of moderate intensity (minimum platelet count reached > 100), seems to suggest, as described by Xuan et al.,3 that prior exposure to heparin is not absolutely necessary to induce HIT in COVID-19 patients, and that HIT can occur spontaneously as a result of SARS-CoV-2 infection.
Value of the biochemical and hematological variables studied, baseline and at 5-10 corresponding to the 3 cases of patients with suspected heparin-induced thrombocytopaenia.
| Case 1 | Case 2 | Case 3 | ||||
|---|---|---|---|---|---|---|
| Variable | Baseline | 5−10 d | Baseline | 5−10 d | Baseline | 5−10 d |
| Procalcitonin. ng/mL. | 1.0 | 0.9 | 0.198 | 0.065 | 0.136 | 1.81 |
| Leukocytes 103/mm3 | 12.2 | 16.9 | 22 | 7.4 | 3.7 | 3.3 |
| Glomerular filtration (CDK-EPI). mL/min | 42 | 31 | 80 | 85 | 90 | 90 |
| Prothrombin time. s | 13.9 | 15.4 | 14.9 | 12.8 | 12.8 | 11.7 |
| Clauss fibrinogen | 559 | 434 | 152 | 128 | 613 | 450 |
| Ferritin. ng/mL | 211 | 136 | 1.339 | 1.014 | 839 | 1.088 |
| D-dimer ng/mL | 448 | 676 | 4.234 | 4.125 | 1.287 | 790 |
| Platelets 103/mm3 | 239 | 111 | 182 | 90 | 385 | 186 |
| Platelet decrease ≥ 50% | Yes | Yes | Yes | |||
| Thrombosis | No | No | No | |||
| Other causes thrombocytopenia | No | No | No | |||
| 4Ts score | 6 | 6 | 6 | |||
Values are presented as mean (standard deviation).
d: days.
Our results show a high occurrence of HIT (6.9%) among COVID-19 patients under prophylactic treatment with LMWH. However, the platelet decline was moderate and transitory, with recovery occurring during convalescence, either because the viral infection was less severe or because lower heparin doses were used. Therefore, although several authors have reported a protective effect of anticoagulation with heparin in severe COVID-19 patients,4 the potential risk of HIT should be highlighted, especially when using high doses.
Regarding the limitations of this study, it should be noted that it is a retrospective design, and it focuses solely on the exploration of thrombocytopaenia. The influence of other therapies (for example, hydroxychloroquine) has not been evaluated and additionally, it is possible that there has been a ‘non-pharmacological change’ in the patients’ treatment, during the study period, in accordance with advancing knowledge of the COVID-19 pathophysiology. However, due to the lack of specific drugs against this infection, most of the patients received a similar treatment and, therefore, we believe that the results of the current study still have some clinical importance.
In conclusion, the incidence of HIT observed in patients with COVID-19, undergoing thromboprophylactic treatment with LMWH, is high (6.9%) although of moderate intensity. Therefore, in patients with a strong suspicion of HIT, heparin treatment should be suspended and/or continued with an alternative anticoagulant treatment, to avoid the high risk of HIT-induced thrombosis.
Please cite this article as: Lozano R, Franco ME. Incidencia de trombocitopenia inducida por heparina en pacientes con enfermedad por coronavirus 2019. Med Clin (Barc). 2020;155:409–410.