Functional and aesthetic outcome is an indication of successfully dental implant treatment. Single implant with chairside immediate provisional crown loading is preferred treatment for patient aesthetic demand and implant survival success.
ObjectiveThis case report is to show an alternative procedure to get good functional, aesthetic, less morbidity, and reducing treatment period with a chairside immediate provisional crown.
CaseA 54 years old women wanted to replace her missing upper left canine with a dental implant. She hoped that this procedure would not affect her appearance. A single implant with 4mm diameter and 10mm height was placed in the upper left canine area. A rigid abutment was installed, and a chairside provisional crown was built at a rigid cap immediately after surgery.
ConclusionA chairside immediate provisional crown after a single implantation procedure is a very good alternative to get an aesthetic, functional, morbidity, and shorter treatment.
A dental implant has been used in dental practice for more than three decades and well accepted as a therapy for edentulous patients.1,2 This high acceptance of dental implants has made greater expectations from both patients and clinicians in the success of this therapy. In many years, osseointegration of the fixture has been used as the main focus in many studies and research to raise the implant survival rate. Nowadays, with the development of implant surface treatment, osseointegration can be considered as a predictable biologic phenomenon. However, osseointegration of the implant does not ensure patient satisfaction, especially on the aesthetic area.3 so that why the functional and aesthetic outcome becomes an indication of successful dental implant treatment. Smith and Zarb extended these criteria by indicating a successful implant must have an adequate aesthetic appearance. The aesthetic outcome is determined by healthy and stable peri-implant tissue.3
According to many previous studies, many researchers believed that after implantation in the jaw for a future prosthesis, titanium implants should be left submerged to undergo a healing process before they are capable of functional loading. This healing process, which is called osseointegration, could be achieved entirely in a period from 3 to 6 months. The reason for the delayed loading was to avoid micro-movement on the implant, which could interfere with the healing process. If this situation occurs, connective tissue can grow at the interface between the implant surface and the bone.3 The result would be the failure of the implant due to not being able to resist the masticatory forces. The original two-stage procedure with delayed implant loading has been modified over the years with the introduction of early and immediate loading protocols, in the attempt to reduce treatment time and patient discomfort. With the increasing demand for a quicker and shorter treatment time, the concept of implant placement protocol in conjunction with immediate provisional has received great attention.2,4
This case report aimed to provide an alternative of immediate temporary crown that can be done in the chairside immediately after implant surgery.
Case presentationA fifty-four-year old-women came to Hasanuddin University Dental Hospital wanted to replace her missing upper left canine. She has been used a removable denture for over than five years and felt comfortable with it, but a year ago, she heard about dental implant treatment that has a better comfort than her denture. She comes to the hospital with high expectation to get a better outcome for her missing upper left canine replacement and wanted the treatment procedures did not affect her appearance.
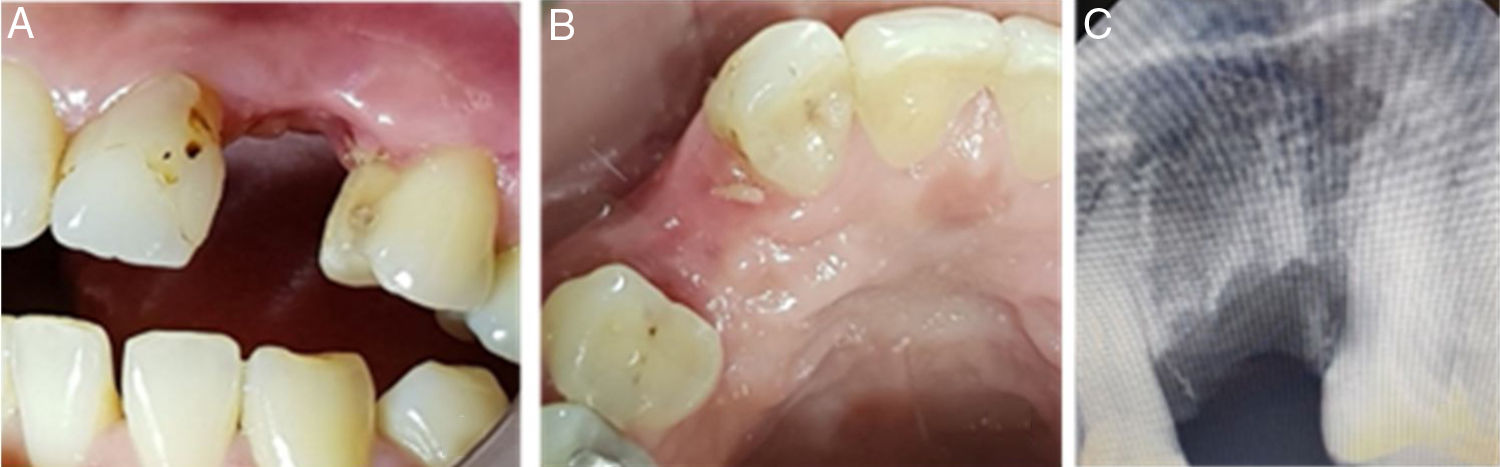
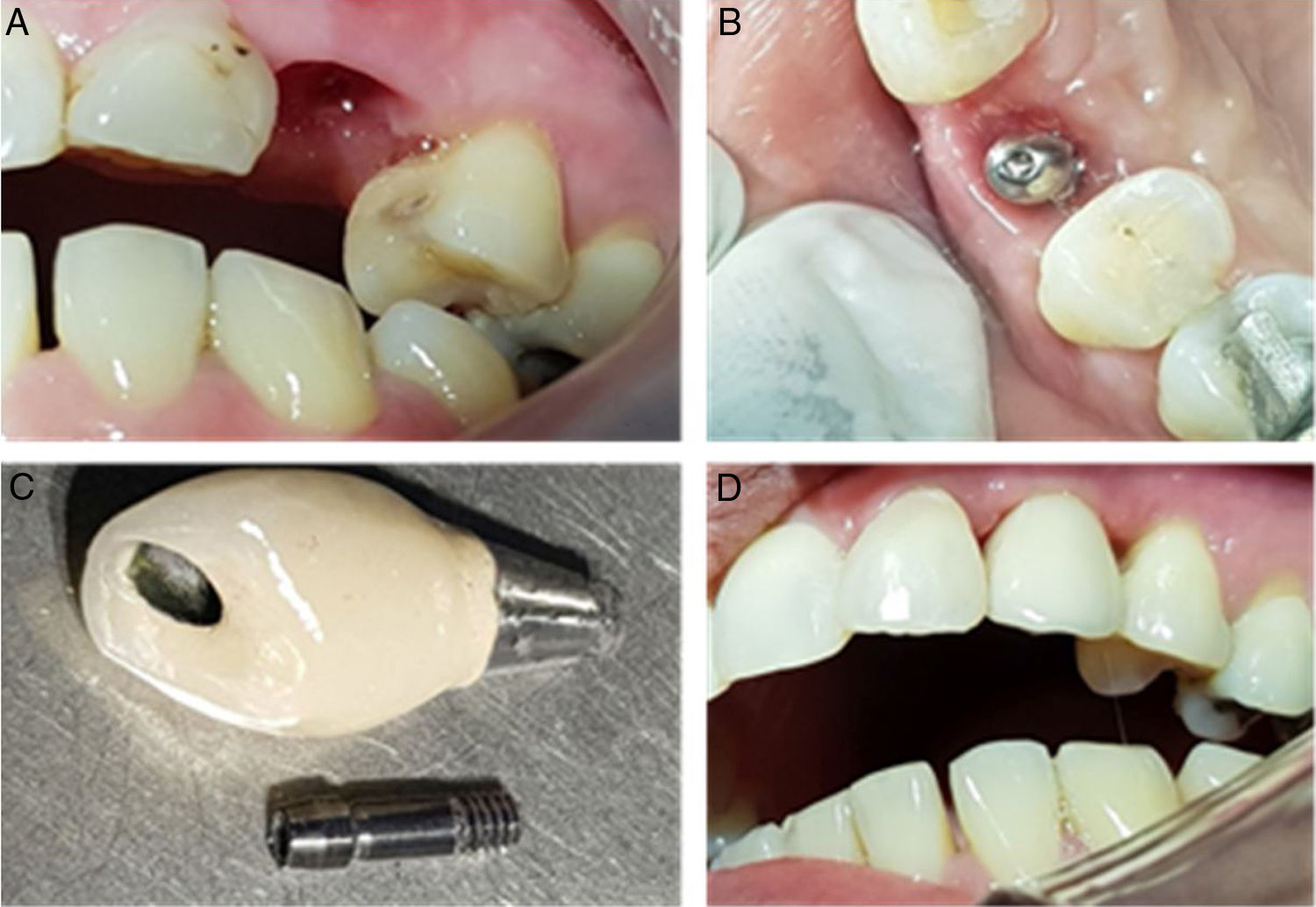
There were no systemic disease and allergic history. A dental examination showed edentulous ridge was found on #23 with 1m m gingival recession on #22 and #24. The inadequate and overhanging filling was on #22 (Fig. 1).
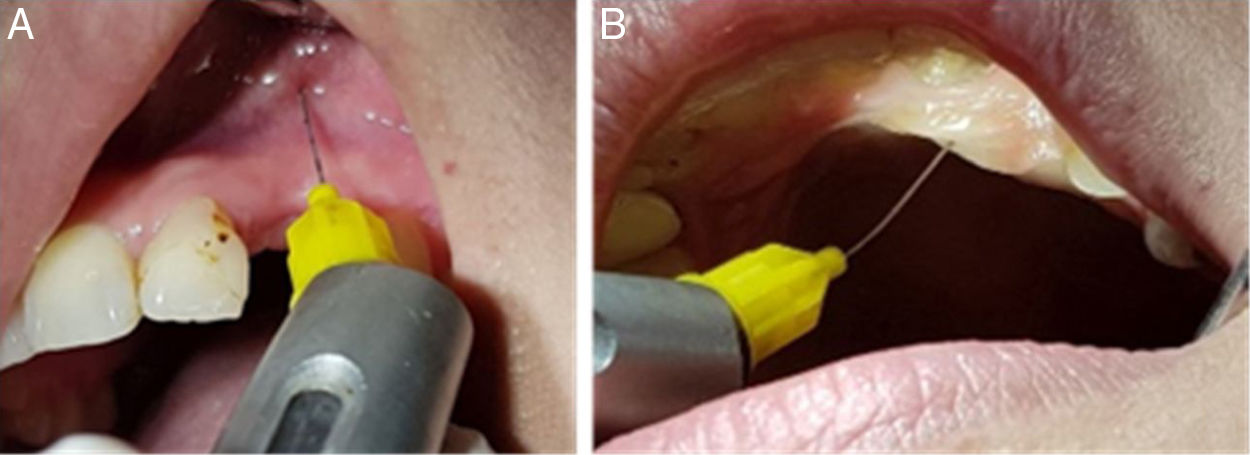
Periapical radiography examination showed a reduction of alveolar bone around 3mm on adjacent teeth (Fig. 2). 11mm mesial-distally available space was measured from the study model and 13mm vertical available space from the alveolar crest to the sinus base. On the labial-palatal aspect, 7.5mm bone thickness was measured with a bone mapping technique. Base on the patient condition, a proper discussion was done, and we decided to put a 4mm diameter with 10mm height single implant with immediate provisional crown procedures for her treatment with screw-retained type prosthetic.
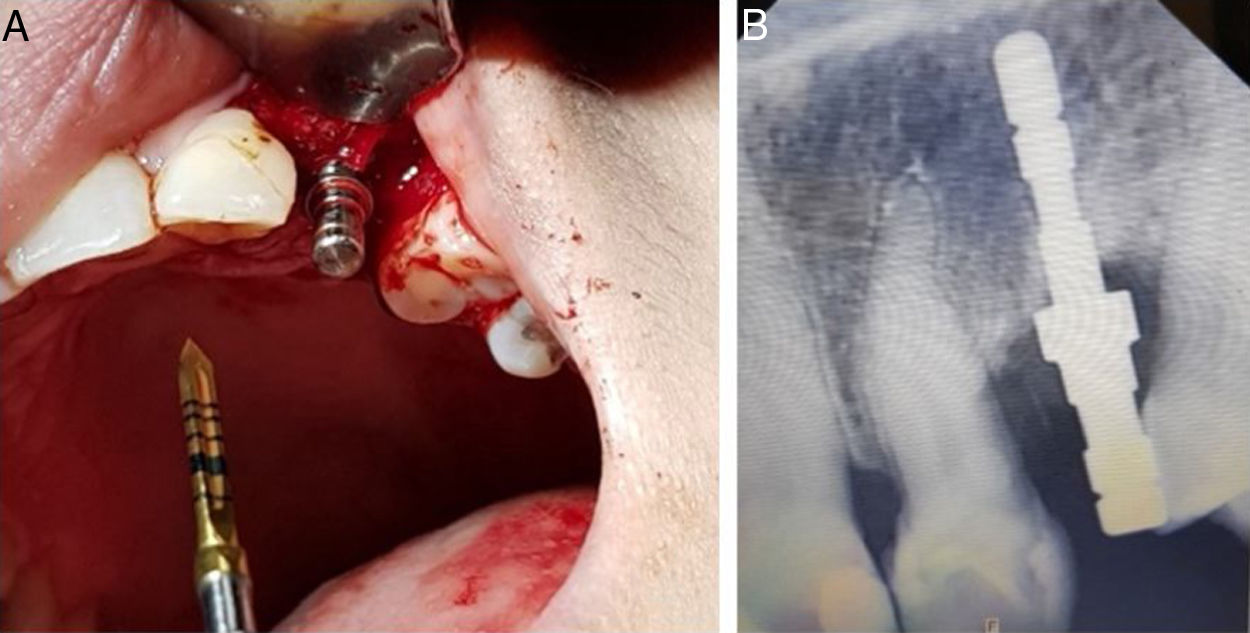
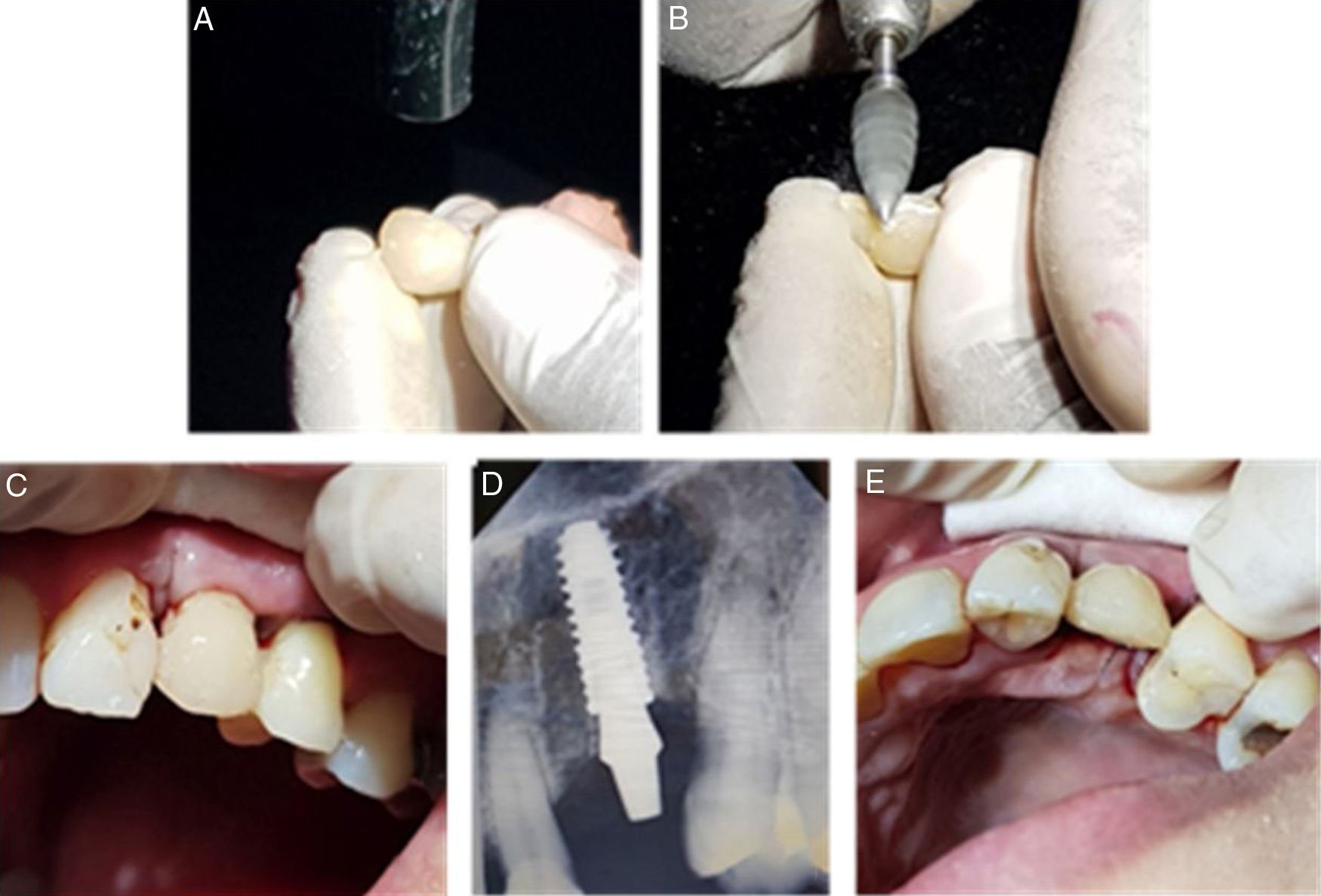
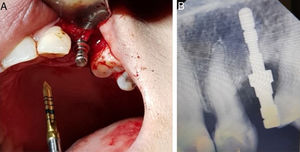
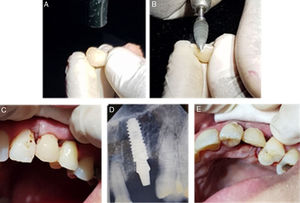
The surgery was done on the first visit. Middle crestal incision was made and full-thickness flap elevation was done to get access to the bone. Initial bur was drilled in the bone crest and the parallel pin was inserted to check the angulation (Fig. 3). The normal bone type was detected and the drilling stops at 4mm diameter drill with 10mm height (Fig. 4). A Tapered Implant with 4mm diameter and 10mm height was inserted in the drilling site with 1mm below the crestal bone. Primary stability was measured with a manual torque wrench and showed 45Ncm in the last torque. 1.5mm residual bone thickness has remained on the implant palatal aspect and 2mm thickness on the labial. A rigid abutment with 4mm diameter and 4mm height was placed and a provisional crown was built on the rigid cap. Composite resin was manually put on the rigid cap and formed to be left upper canine directly at the chairside. After gaining an ideal shape and polished well, the provisional crown was put on the rigid abutment and sutured were performed to close the flap. We used 5–0 blue nylon suture with 18mm reverse cutting needle to minimize the trauma. Free occlusal loading was ensured by eliminating the occlusal contact. Clindamycin 300mg, mefenamic acid 500mg, and chlorhexidine oral gargle were given after surgery.
(A) A chairside provisional crown on #23 with composite resin material. (B) Shaping and polishing #23 temporary crown. (C) Labial aspect the provisional crown after suturing procedures. (D) Periapical radiography, show the position of the implant and rigid abutment after provisional crown loading and suturing procedures (E).
The suture was removed ten days after surgery and very good healing showed on the wound area. Fixture level impression was done after 9.5 weeks and the gingiva emergence profile was very good with a small black triangle on the mesial and distal of the crown (Fig. 5). Two weeks later the screw-retained final restoration was placed. The patient was very satisfied with the treatment outcome, especially because she did not experience the edentulous period after the surgery.
DiscussionsRestoration a single tooth loss with an implant-supported crown has become a preferred rehabilitation treatment option.4 In the anterior maxilla, osseointegration alone is not sufficient; patient satisfaction is a key factor in the success of implant therapy. Provisional implant restorations are essential tools used by restorative dentists to optimize aesthetic outcomes for single-tooth implant restorations.3 It is become a choice because of the reduction of the treatment period, patient discomfort, and the patient get the aesthetic immediately after the implantation procedure. Time reduction was gain bay the single-step operation procedure by using immediate provisional crown without waiting for the healing process or osseointegration achievement. This healing process, which is called osseointegration, could be completely achieved in a period from 3 to 6 months.4
This one-stage surgery with provisionalization become a challenge for healing process, because of micromovement that can be happened during this period that can lead into osseointegration failure.4 Block et al., in a review of the literature, found reported implant success rates ranging from 91% to 97.8% when implants were loaded with a provisional restoration.4 A study showed an implant survival rate of 91.7% for immediately loaded implants at the two years of follow-up. Over the past 20 years, some studies and trials have reported similar results with trans-mucosal implants compared with submerged implants. As a result, it is not necessary to submerge the implants under the mucosa during the healing period, which eventually introduced the immediate loading protocol.
Adequate primary stability is the main prerequisite to apply an immediate provisional protocol. Secure mechanical retention of the implant into the host bone is necessary to prevent implant-bone micromovements, which could lead to a failure of the osseointegration process.5 Trisi et al., explained that between the implant and peri-implant bone, there should be a minimum gap, although without there being micromotions over the threshold, that could cause a deformation of the newly formed tissue able to destroy the new cells and vessels that have formed in the gap, determining the penetration of the osteoclasts that induce the bone resorption.4
There is no universal consensus about the minimum primary stability threshold to reach for a safe application of immediate provisional protocols; however, implant stability quotients (ISQ) >60–65 or peak insertion torques >35Ncm are mostly accepted as minimum values.3 Riskalah et al., insertion torque undoubtedly play an important role in the primary stability and successful osseointegration of implants, there seems to be no correlation between insertion torque and implant failure above 35Ncm threshold of insertion torque.4 The measurement of the moment of force (torque) necessary to insert an implant in its lodging place in the bone is a parameter for studying initial stability. The higher the implant insertion torque, the higher will be the initial stability reached.5
The bone density also become a consideration in immediate loading provisional restoration. Immediate provisional or fully loading restoration may be considered a valid therapeutic choice, even in low-density bone, as long as at least 45N/cm of insertion torque is reached.4
Implant design parameters such as implant surface, thread configuration, and body shape have a correlation relationship, that will define the initial stability of the implant. It is believed implant sites using a tapered design, and surface modification can increase the primary stability in the low-density bone. Furthermore, recent experimental preclinical work has shown the possibility of attaining primary stability of immediately loaded, tapered dental implants without compromising healing and rapid bone formation while minimizing the implant stability loss at compression sites. A tapered-screw implant design will provide adequate stability because it creates pressure on cortical bone in areas of reduced bone quality. Building on the success of traditional tapered implant therapy, newer tapered implant designs should aim to maximize the clinical outcome.5
The patient need of aesthetic, in this case, can be provided by the used of immediate provisional that build in the chairside. Functionally as aesthetic, this procedure also reduced the number of surgical visits, advantages of a bimodal approach involve less patient morbidity and enhanced maintenance of peri-implant soft tissue margin, and aesthetics. Due to the high aesthetic demands in the anterior maxilla as well as the patient's disaffection towards removable provisionals, immediate provisional restoration of single-tooth implants has gained popularity provided that satisfactory primary implant stability is reached.6 The immediate provisional restoration carried soft tissue support and subsequent optimization of peri-implant soft tissue aesthetics with regards to papilla preservation and stability of the gingival margin.5
The raised of the black triangle on the distal and mesial of the crown is because of the bone resorption that has been happening during 5 years post-extraction and the used of removable prosthesis. The 3mm resorption of the bone from the normal height position made the distance between bone crest with the proximal contact of the crown become 6mm long. Tarnow et al. (1992) investigated the effect of the distance from the contact point to the crest of bone on the presence of the interproximal dental papilla and found out that when the measurement from the contact point to the crest of bone was 5mm or less, the papilla was present almost 100% of the time.7
ConclusionLong term aesthetic outcome was primary patient demand on single dental implantation in aesthetic area. With the precise treatment consideration, immediate provisional loading on single implantation can get high survival rate. A chairside immediate provisional crown after a single implantation procedure is a very good alternative to get an aesthetic, functional, morbidity, and shorter treatment.
Conflict of interestThe authors declare no conflict of interest.
Peer-review under responsibility of the scientific committee of the International Conference on Women and Societal Perspective on Quality of Life (WOSQUAL-2019). Full-text and the content of it is under responsibility of authors of the article.