To improve the patient's quality of life without extracting periodontally compromised teeth.
CaseA 54 years old male patient came with chief complaint mandibular incisor mobile since one month ago. Intraoral examination revealed there were deep pockets and gingival recession on anterior teeth with degree 2 mobility. Radiograph examination showed that severed bone loss and increased periodontal ligament space. Periodontal flap surgery and then the teeth would be splinted permanently using metal frame partial denture because of patient's poor oral hygiene habit.
ConclusionSurgical approach was the gold standard to prepare periodontally compromised teeth before splint permanently using metal frame partial denture.
Chronic periodontitis is an inflammatory disease induced by bacterial biofilm in the gingival margin and characterized by gingival inflammation, loss of attachment and alveolar bone. The loss of attachment and alveolar bone can lead to increased tooth mobility if this condition left untreated. Occlusal trauma can also lead to increased tooth mobility. Increased tooth mobility affect function, esthetics, and patient's comfort.1,2
Treatment of chronic periodontitis can be done by non-surgical or surgical approach. Non-surgical therapy consists of oral hygiene instructions and scaling and root planing. Most of the cases showed decreased probing pockets depth, better attachment level. But this approach can only be successful in shallow to moderate pockets. If the pockets are deeper, it should be treated using a surgical approach. The main goal of periodontal surgery was to gain access to root surface for adequate debridement and to establish gingival contour that is optimal for the patient's self-performed plaque control.3,4
Periodontally compromised teeth usually have increased teeth mobility and will challenge the clinician. Therefore, splints are used to treat this condition. Splinting is a procedure by which a tooth resistance to an applied force is increased by joining it to adjacent teeth. Yogini et al. believe that splinting mobile teeth assists in regeneration of periodontal health, improve function, comfort, esthetics.2,5
Many splinting materials have been developed and it is important to classify them. A clinician has to able to classify them in order to make the best use of the splint materials. There are three types of splinting, temporary, semi-permanent, permanent splint. When periodontal compromised teeth treated with splinting, a patient may be having difficulty in performing oral hygiene and can accumulate more plaque.2
Removable denture appliance is one of the permanent splints. Removable denture appliance can restore esthetic, mastication, speech function of a patient. A removable denture can also be used as splinting for periodontally compromised teeth. This case report aimed to describe periodontal flap operative on periodontally compromised teeth and followed by metal frame denture.
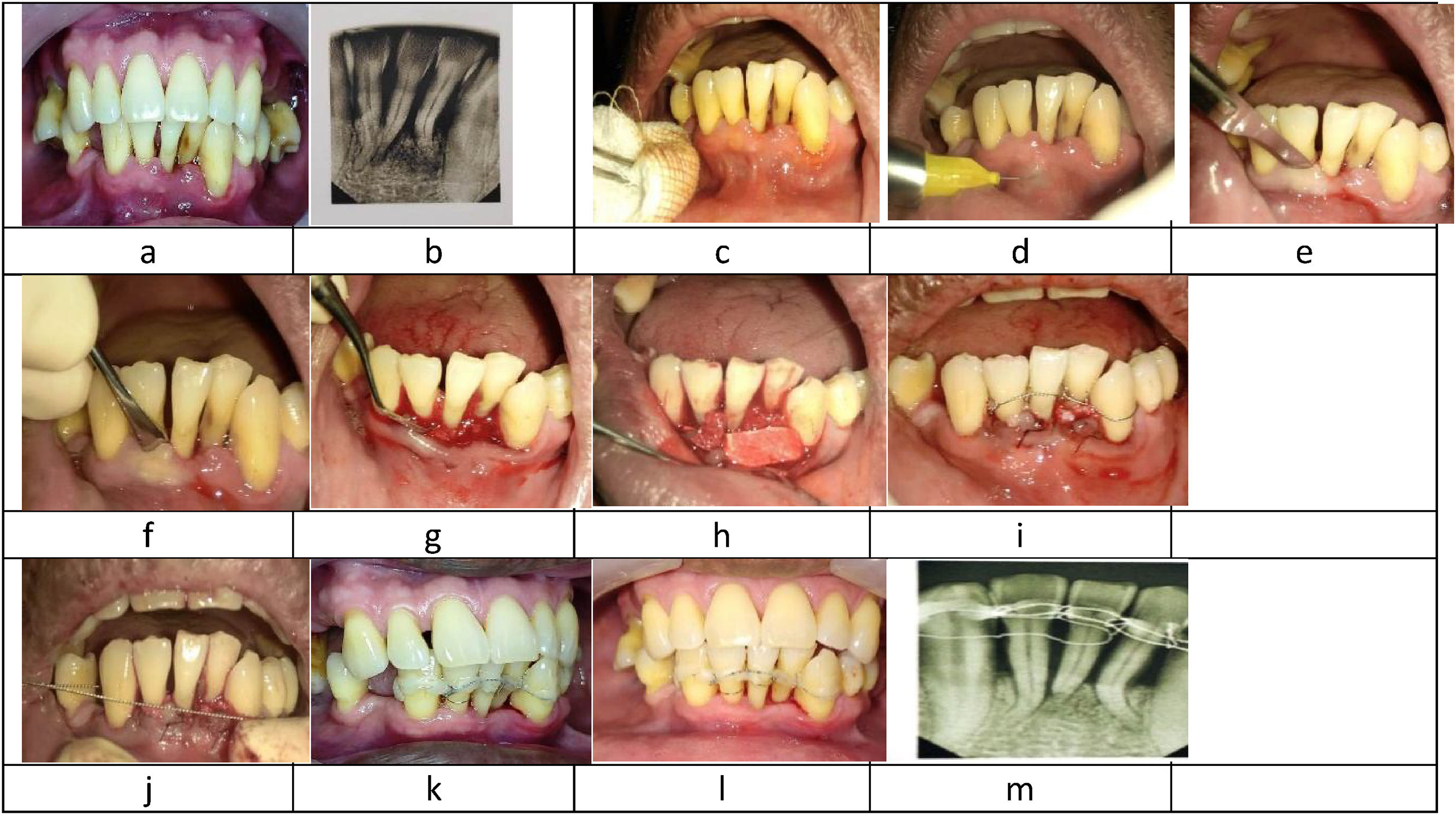
Case reportA 54 years old male patient was referred to Dental and Oral Hospital Hasanuddin University with chief complain mandibular incisor mobile since 1 month ago. Intraoral examination revealed that there were deep pockets and gingival recession on teeth 31, 32, and 41 with degree 2 mobility. A pulp sensitivity test was done on the teeth and showed a positive result. Radiograph examination showed that severed bone loss on teeth 31, 32, and 41 and increased periodontal ligament space.
The initial treatment to this case were scaling and root planing, followed by occlusal adjustment and splinting. After scaling and root planing were done and the teeth were polished using pumice at low speed, occlusion was checked using articulating paper. Selective grinding was done to the teeth having excessive occlusal trauma and the temporary splint was applied. Wire ligature splint was used in this initial treatment.
One week after the initial treatment. Periodontal flap surgery was done. The anterior teeth were disinfected using povidone-iodine and administered anesthesia. Then incision was done using blade no. 15. The flap was elevated using a periosteal elevator. A full-thickness flap was used in this case.
The granulation tissue and subgingival calculus were removed using curette Gracey nos. 1–2, 3–4 and ultrasonic scaler to achieve the smoother root. Bone graft and bio-adsorbable membrane were applied. The flap was sutured using 4–0 nylon. The wire ligature splint was changed to composite wire splint. At the end of the surgery, periodontal dressing was applied.
The patient was instructed to take amoxicillin and potassium clavulanate three times a day for 5 days, metronidazole three times a day for five days and mefenamic acid twice a day for 5 days. The patient was recalled after 1 week to remove periodontal dressing and the suture. The clinical examination was done, tissue healing was good but plaque and supra gingiva was found and removed using ultrasonic scaler.
After three months follow up, plaque and supragingival calculus were found, and radiograph examination showed no more progressive bone loss on 31, 32, and 41. The composite wire splint was removed and the patient was referred to prosthodontics departments for metal frame denture fabrication (Fig. 1).
(a–m) Operative view. (a, b) Clinical and radiograph of the patient's first visit; (c, d) disinfect and anesthesia of working area; (e, f) incision using blade no. 15 and full-thickness flap elevation; (g) mechanical debridement using curette Gracey; (h) bone graft and bio-adsorbable membrane were applied to the surgery area; (i) suturing was done; (j) composite wire splinting was applied after suturing; (k) clinical finding 1 week post-surgery; (l–m) Clinical and radiograph finding three months post-surgery).
The aim of periodontal therapy was to preserve natural teeth, to maintain and improve periodontal health, comfort, esthetics, and function. Mechanical debridement was the core of any periodontal therapy, and could be achieved by non-surgical and/or surgical therapy with instructions in self-administered oral care. Non-surgical therapy referred to supra gingiva and subgingival scaling and root planing. Non-surgical therapy aimed to control the bacteria that cause gingivitis and periodontitis.3
Surgical therapy facilitated mechanical debridement of the roots. Surgical therapy gave better access for removal of etiological factors, reduced probing depth, regenerated periodontal tissue. Mehraj et al.,3 in their study found that surgical therapy gave better result than non-surgical therapy, due to better access to the root debridement.
David et al.6 suggested that scaling and root planing did not attain treatment goals, and periodontal surgery should be considered as the next step. Treatment of mild-to-moderate chronic periodontitis had to focus on establishing excellent patient plaque control and did not have to treated surgically. On the other hand, surgical therapy offered benefits beyond scaling and root planing in treating severe periodontitis. A study by Heitz-Mayfield et al.7 suggested that chronic periodontitis with pocket depth more than 5mm, open flap debridement gain clinical attachment level significantly than scaling and root planing only. But before did the conservative periodontal surgery, the clinician must decide whether this procedure would give significant advantages beyond scaling and root planing or not.
The loss of attachment and alveolar bone could lead to increased tooth mobility. Tooth mobility was an important clinical finding in predicting the outcome of a treatment. Therefore, splinting was a recommended therapy to stabilized the tooth. The objectives of splinting were for redistribution of forces, to preserve arch integrity, restoration of functional stability, and psychological wellbeing of the patient and to stabilize mobile teeth during surgical procedure.1
Wiesgold classified splints into three categories, they were temporary, provisional and permanent splints. A temporary splint used on a short term, usually less than six months, this splint's function was to stabilize teeth during periodontal treatment, such as periodontal surgery. The provisional splint used for diagnostic purpose and last for few months and allow the clinician to see the teeth respond to the treatment. A permanent splint used indefinitely, it could be either fixed or removable.1,8,9
Sujeetha et al.5 suggested that splinting was a well-accepted holistic periodontal therapy which results in morale boost, improve patient comfort, and function. Gautam et al.10 in their study suggested that ligature wire that used in orthodontic treatments with 0.33mm of thickness was considered flexible and appropriate for flexible splints thus allowing psychological movements of the teeth.
The wire composite splint was found in 1982 by O’riordan et al.,11 who used etching technique and placed composite on the labial surface of the teeth, fixate them with a wire that was bent along the arch. This splint met most demands of teeth fixation. The advantages of this splint could be prevented and eliminated resorption area.
After the periodontal surgery and temporary splint were applied, the patients would be referred to prosthodontics department to had metal frame denture made for him. This denture would prevent the migration of teeth in vertically and horizontally, distributed occlusal force, and gave stabilization. Therefore, the remains teeth could function normally. Krisnandi et al.12 suggested that periodontal treatment before fabrication of metal frame denture was a need to improve the teeth ability to receive occlusal force.
In this case, after one week and three months followed up, we found a plaque and supragingival calculus. Perierira et al.13 suggested that splinting sometimes made oral hygiene became a little difficult, especially at interdental area and had to give extra effort to achieve good oral hygiene. Interdental tooth brushing was more effective rather than conventional tooth brushing in removing biofilm and reducing gingival inflammation. Therefore metal frame denture was recommended in this case, due to patient bad oral hygiene care.
Ranny et al.14 suggested that metal frame denture could be used as a permanent splint to achieve good stability and replace the missing teeth. This denture was a part of periodontal therapy and must be done as soon as possible when the periodontal tissue of the patient got better after the previous periodontal therapy. Krisnadi et al.12 suggested that periodontal therapy was a need before fabrication of metal frame denture to improve teeth ability to receive occlusal force and the metal frame denture function as a stabilizer and restored the efficiency of mastication.
ConclusionThe surgical approach was the gold standard to prepare periodontally compromised teeth before splint permanently using metal frame partial denture.
Conflict of interestThe authors declare no conflict of interest.
Peer-review under responsibility of the scientific committee of the International Conference on Women and Societal Perspective on Quality of Life (WOSQUAL-2019). Full-text and the content of it is under responsibility of authors of the article.