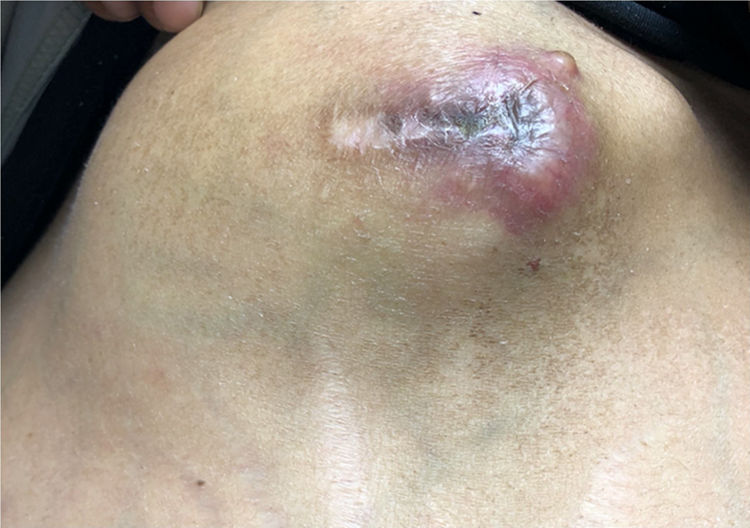
A 45-year-old female was sent for a second opinion to the Gastrointestinal Tumors Unit at our institution with a diagnosis of progressive, metastatic cholangiocarcinoma. Her present illness begun 10 months ago, when an extrahepatic cholangiocarcinoma was incidentally found during ERCP for residual choledocholithiasis after primary laparoscopic cholecystectomy. Additional imaging studies showed non-regional lymph node and port-site tract metastases. The patient received first-line combination chemotherapy with gemcitabine–cisplatin and later showed progressive disease in the abdominal wall after 8 cycles of treatment. She was then treated with capecitabine–oxaliplatin for 4-cycles after which a CT scan demonstrated abdominal wall progression. At her first visit to our institution, the physical exam showed a large, 15×20cm tumor in the right upper abdomen extending to the epigastrium, below the port-insertion site scar (Fig. 1). After a multidisciplinary team discussion, further systemic treatment with combination 5-FU and irinotecan chemotherapy was offered.
Given that some patients with biliary tract cancer are diagnosed incidentally after laparoscopic cholecystectomy, port-site dissemination from tumor seeding is a risk to consider. Although port-site metastases have been associated to diffuse peritoneal recurrence and a poor prognosis, the benefit of port-insertion site primary resection in terms of overall survival remains unknown.