Fitz-Hugh-Curtis syndrome (FHCS) is a perihepatitis that results from the intraperitoneal extension of pelvic inflammatory disease (PID) and classically occurs in reproductive-aged women with sexual activity. This syndrome usually presents with right upper quadrant (RUQ) abdominal pain together with lower abdominal pain and vaginal discharge. However, some patients may present with isolated RUQ abdominal pain mimicking other hepatobiliary pathologies and posing a diagnostic challenge to many physicians.
El síndrome de Fitz-Hugh-Curtis (SFHC) es una perihepatitis secundaria a la extensión intraperitoneal de una enfermedad inflamatoria pélvica (EPI), que habitualmente afecta a mujeres sexualmente activas. Generalmente se presenta con dolor abdominal en hipocondrio derecho (HD) junto con dolor en hipogastrio y aumento de flujo vaginal. No obstante, algunos pacientes pueden presentar dolor en HD de forma aislada, simulando otras enfermedades hepatobiliares, lo cual supone un verdadero reto diagnóstico para muchos especialistas.
Fitz-Hugh-Curtis syndrome (FHCS) is a rare complication of pelvic inflammatory disease and classically occurs in reproductive-aged women with sexual activity. Diagnosis of this syndrome can be challenging because of its similar presentation with many hepatobiliary pathologies. Patients often undergo extensive evaluations before a correct diagnosis is made.
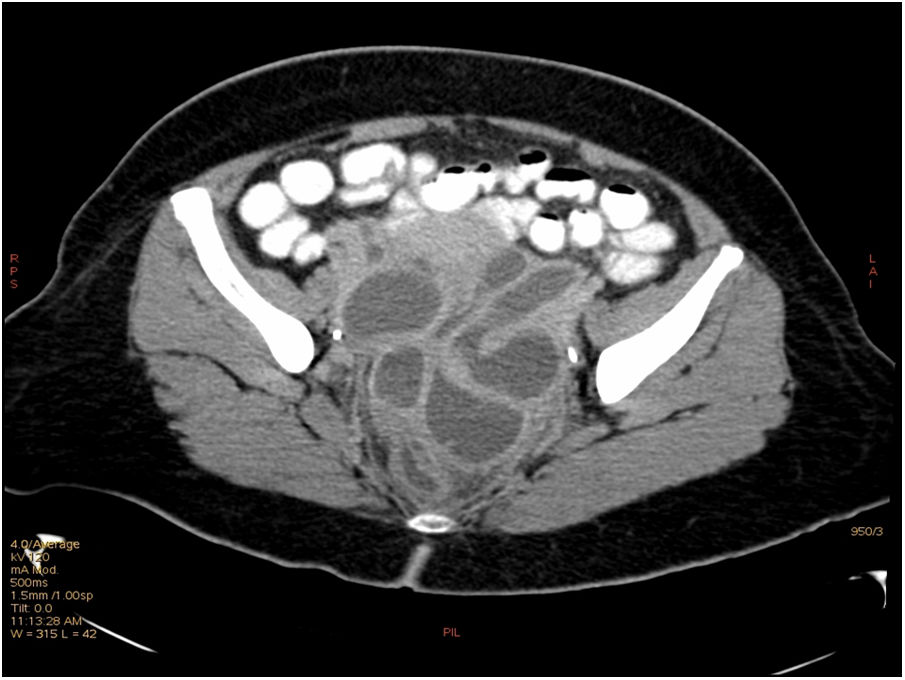
A 48-year old woman presented with fever, emesis and right upper quadrant abdominal pain. She denied other symptoms and sexual activity. Physical examination revealed RUQ abdominal tenderness. Laboratory tests showed 17000/mm3 white blood cell count (range 4000–10000/mm3), 6, 22ng/mL procalcitonine (normal <0.5ng/mL) and 1.64mg/dL bilirrubin (range 0–1.2mg/dL). Serum liver enzymes were also increased: GOT 89U/L (range 4–40U/L), GGT 89U/L (range 5–41U/L) and GGT 178U/L (range 10–71U/L). She had been cholecystectomized a few years ago, and therefore a cholangitis was suspected. Abdominal ultrasound demonstrated no hepatobiliary or intestinal abnormalities. Despite antibiotic treatment for 72h with ciprofloxacine and metronidazole, the patient kept febril and started with lower abdominal pain. She denied vaginal discharge and urinary tests were normal. New laboratory test revealed worsening of C-reactive-protein (17mg/dL, normal <0.5mg/dL) and liver enzymes which persisted despite changing treatment to piperaciline-tazobactam. The combination of a painful liver without evidence of hepatitis or biliary obstruction by abdominal ultrasound and lower abdominal pain raised the suspicion of Fitz-Hugh-Curtis syndrome. A computed tomography (CT) scan was finally performed 7 days after admission which showed hepatomegaly, piosalpinx and tubo-ovarial abscesses, all consistent with pelvic inflammatory disease (Fig. 1). The patient underwent laparoscopic surgery to remove tubo-ovarial abscesses, completed 3 weeks of piperaciline-tazobactam and was finally discharged.
FHCS is characterized by inflammation in perihepatic capsule with concomitant pelvic inflammation without involvement of hepatic parenchyma. The incidence of this syndrome ranges from 4% to 27% in women with pelvic inflammatory disease.1 The etiology is linked to sexually transmitted microorganisms being Chlamydia trachomatis and Neisseria gonorrhea the main etiologies of pelvic inflammatory disease and Fitz-Hugh-Curtis syndrome worldwide. However, 30–40% of cases are polymicrobial not related to sexual activity, like occurred in our patient. Tuberculosis and actinomycosis occur much less frequently.2
The pathophysiology of perihepatitis FHCS is unclear but direct infection of the liver capsule, hematologic or lymphatic spread and an exaggerated immune response have been suggested.1
Typical symptoms include right upper quadrant abdominal pain sometimes with pleuritic features and right shoulder radiation. Abdominal pain develops as a result of congestion of hepatic capsule, spotted hemorrhage, and fibrous exudates. Most patients also have symptoms of acute salpingitis such as lower abdominal pain, which may appear simultaneously or intermittently with the right upper quadrant abdomen pain. Cervical motion and adnexal tenderness may suggest underlying pelvic inflammatory disease.2,3
Diagnosis of this syndrome can be challenging because of its similar presentation with many hepatobiliary pathologies. Patients often undergo extensive evaluations before a correct diagnosis is made.4 A definitive diagnosis requires detection of “violin string” adhesions between the liver capsule and the anterior abdominal wall during intraoperative exploration. However, the use of noninvasive diagnostic procedures is desirable, considering that this syndrome is a benign condition that can be completely cured by oral antibiotics.1,3
Hepatic enzyme values are normal or slightly elevated and ultrasound findings are usually non-specific or even normal in several patients.1,4 Ultrasonography therefore plays a vital role in excluding other diagnosis rather than confirming Fitz-Hugh-Curtis syndrome.5 For suspected cases, culture tests in a cervical smear or peritoneal fluid should be performed using the special media for C. trichomatis.2
Increased enhancement along the hepatic surface on CT during arterial phase together with pelvic inflammatory disease findings may suggest the diagnosis. Recent studies demonstrated that dynamic abdominal CT scan can significantly improve depiction of perihepatic enhancement. This may reflect increased blood flow at the inflamed hepatic capsule, which is consistent with the laparoscopic findings of inflammation and exudate formations. Perihepatic capsular enhancement in the early phase may completely disappear after treatment.5
Treatment consists of antibiotics directed against N. gonorrhoeae and C. trachomatis.2 Mechanical lyses of adhesions can be performed surgically if conservative treatment fails. Treatment of all sexual contacts is desirable.1,3
Fitz-Hugh-Curtis syndrome should be considered as a cause of right upper quadrant abdominal pain in adults in whom imaging and liver laboratory findings remain elusive. Biphasic TC with arterial and portal phases may help ensure adequate medical treatment as well as avoid invasive procedures.
Financial supportNone.
Conflict of interestsAuthors reported no conflict of interests in relation to this article.