Considering the various effects of the corona epidemic on humans, the current study was conducted to investigate adults' nutritional patterns and the psychological status during the COVID-19 pandemic.
Methods and materialsThis cross-sectional analytical study was performed on adults in Iran during the COVID-19 epidemic. A total of 315 participants were examined by the convenience sampling method. To collect data from the standard 21 questionnaire (das) and Eating Attitudes Test - 26 items were used. The data were analysis by SPSS and independent t-test, correlation coefficient, and chi-square analysis of variance at a significance level of less than 0.05.
ResultsThe mean age of the participants was 31.93±10.02 years. Based on the findings, 31.1% had some degree of depression, 29.5% had some degree of anxiety, and 31.7% have been affected by varying degrees of stress. Also, 8.7% of the participants had eating disorders. A statistically significant relationship was observed between depression score, anxiety score, stress score as well as an overall score of mental disorders and eating disorders; in such a way that with the increase of each of these cases, the score of eating disorders also increases.
ConclusionFollowing the prevalence of the COVID-19 epidemic and its psychological effects, the level of stress and anxiety has increased. Awareness controlled the level of anxiety and stress and prevented its adverse effects on nutrition.
Teniendo en cuenta los diversos efectos de la epidemia de corona en los humanos, el estudio actual se realizó para investigar los patrones nutricionales y el estado psicológico de los adultos durante la pandemia de COVID-19.
MétodosEste estudio analítico transversal se realizó en adultos en Irán durante la epidemia de Covid-19. Un total de 315 participantes fueron examinados por el método de muestreo por conveniencia. Para recopilar datos del cuestionario estándar de veintiún (das) y la prueba de actitudes alimentarias, se utilizaron 26 ítems. Los datos fueron analizados por SPSS y prueba t independiente, coeficiente de correlación y análisis de varianza de chi-cuadrado a un nivel de significación de menos de 0,05.
ResultadosLa edad media de los participantes fue de 31,93 ± 10,02 años. De acuerdo con los hallazgos, el 31,1% presenta algún grado de depresión, el 29,5% presenta algún grado de ansiedad y el 31,7% se ha visto afectado por diversos grados de estrés. Asimismo, el 8,7% de los participantes presentaban trastornos alimentarios. Se observó una relación estadísticamente significativa entre la puntuación de depresión, la puntuación de ansiedad, la puntuación de estrés, así como una puntuación global de trastornos mentales y trastornos alimentarios; De tal forma que con el aumento de cada uno de estos casos, también aumenta la puntuación de los trastornos alimentarios.
ConclusiónA raíz de la prevalencia de la epidemia de Covid-19 y sus efectos psicológicos, el nivel de estrés y ansiedad ha aumentado. La conciencia controló el nivel de ansiedad y estrés y previno sus efectos adversos sobre la nutrición.
Eating disorders are one of the most common mental/psychosomatics disorders that cause many problems in physical health and mental function, also they impair the quality of life of the affected person and cause death.1 Eating disorders are characterized by behaviors such as reduced eating and overeating.2 The clinical manifestations of these disorders are anorexia nervosa and bulimia nervous, which can lead to malnutrition and mental disorders such as depression.3 Anorexia nervosa and bulimia nervosa are often highly correlated with chronic eating disorders.4 The incidence of overeating is higher than anorexia nervosa and it is about 90%–95% in women.5
Anorexia nervosa leads to excessive stimulation, weight loss, and psychological distress.6 The prevalence of various disorders in Western societies is 6% for anorexia nervosa and 1% for bulimia nervosa.7 Studies revealed that a type of eating disorder, which is seen as eating disorder, is associated with social, emotional, and psychological factors.8 Problems related to eating disorders due to illness or inappropriate behaviors and habits have caused new dangers and increased the incidence of various physical and mental diseases which has caused a vicious cycle in the health of society.9 The most common mental disorders are associated with eating disorders, anxiety, and depression. Anxiety is an unpleasant and vague feeling often in the form of anxiety, which is defined by a sense of doubt about an unknown factor.10 This unpleasant feeling can be accompanied by many physiological, emotional, and mental symptoms which manifest in the form of a strong emotional feeling.11 Because one of the main ways to control COVID-19 is public health measures, this disease was able to cause severe quarantine measures in the world in a short period.12
Quarantine can be applied voluntarily or mandatory at the individual- or community level. Voluntary and home quarantine is usually preferred13,14 and the duration of quarantine should be equal to the maximum incubation period (14–21 days). Social distancing is also a form of quarantine that is done to reduce interactions between people in a community, and on a large scale can delay the peak of the epidemic to allow the healthcare system to be more resilient to large numbers of patients.13
This strict policy of quarantine will cause psychological, social, and economic effects and will lead to social isolation, financial losses, discrimination, and so on. Also, limited human awareness of this disease and the news and rumors related to this disease cause and increase anxiety and fear, boredom, despair, etc.12 Therefore, not only paying attention to patients' health measures to deal with the disease but also psychological care is necessary to reduce stress and psychological pressure.15
Government policies to break the chain of the COVID-19 pandemic has left many people without mobility and physical activity as before and spend most of their time at home. All of these issues create a challenging environment for people with anorexia nervosa and bulimia nervosa.16 Due to the prevalence of the COVID-19 disease worldwide, including in Iran, and the increase in anxiety and worry of people, the prevalence of eating disorders may increase. So, investigate adults' nutritional patterns and the psychological status during the COVID-19 pandemic.
Methods and materialsThis descriptive–analytical cross-sectional study was performed on adults living in Iran. The statistical population included adults aged 25–70 years living in different provinces of Iran.
Sampling is done with a simple sampling method. The sample size was 315 participants, with a 95% confidence level and an accuracy of 0.03. The inclusion criteria were participation in the study voluntarily, and answering all questions of the questionnaire. Exclusion criteria were individuals under 25 years old and over 75 years old, questionnaires that have been completed with more than 2 IDs, the time to complete the questionnaire was less than 7 min.
After the approval of the plan by the Research Council and obtaining the ethics code of IR.MEDSAB.REC.1399.067 due to the epidemic conditions of the COVID-19 epidemic, we prepared a questionnaire online and the link of it for the groups was sent to different provinces (Questionnaire link with explanations about the questionnaire and voluntary cooperation). The data collection tool was the Psychological Disorders Questionnaire which was a standard 21 questionnaire for measuring depression, anxiety, and stress.
Each question in this questionnaire has 4 options: never, rarely, sometimes, and always, on the Likert scale. The lowest score (0 points) belongs to the “never” option and the highest score of 3 points) belongs to the “always” option. This questionnaire consists of 3 subsets, each of which consists of 7 questions, and the total score of each sub-set is separately for measuring depression, stress, and anxiety.
Its validity and reliability have been confirmed by Sahibi et al. in the article Validation of Scale for Population in Iran.17 The EAT-26 questionnaire was used to assess eating disorders, the translation, validity, and reliability of which were confirmed by Dejkam et al. based on EAT. Each Likert scale question is categorized and for each statement, the answer is “always”, 3 points, “most of the time” 2 points, and “often” 1 point. The remaining 3 options, including “sometimes”, “rarely”, and “never”, score 0. A score above 20 is considered a disorder.18
Questionnaires are completed by individuals, consequently, the questionnaires are checked for repeatability of ID and response time and age. Questionnaire data that met the entry requirements were entered into SPSS 16 software. Descriptive statistics (mean and standard deviation, frequency), independent t-test, correlation coefficient, and chi-square analysis of variance were used to analyze the data.
ResultsIn this study, 315 participants were studied. Their mean age of them was 31.93 with a standard deviation of 10.02 years. In terms of gender, 38% were male and 62% (194) were female. Considering marriage status, 46.2% were married, 52.2% were single, and 1.6% were divorced.
In addition, 1.3% were primary literacy, 24.4% had a diploma, 44.1% had a bachelor's degree, 16.7% had a master's degree, and 13.5% had a doctorate. Also, 36.8% were affected by the virus SARS-CoV-2 and 63.2% were unaffected. In terms of depression, 68.9% were healthy and 31.1% had a degree of depression. Regarding anxiety, 29.5% had a degree of anxiety and 31.7% had different degrees of stress. Also, 8.7% of participants had eating disorders.
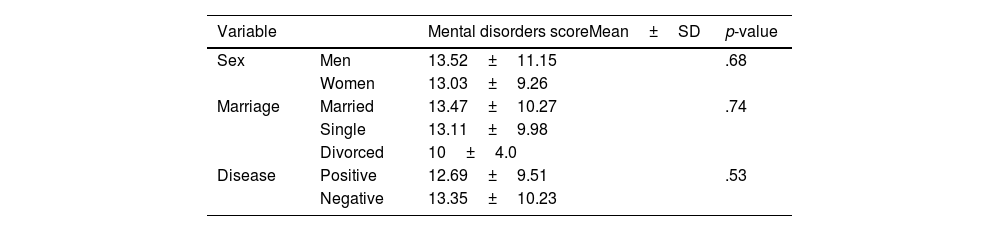
The mean score of the mental disorder questionnaire was not significantly different between the 2 genders (0.69), also there were not any significant differences in terms of marital status (p=.74), the mean score of mental disorders in group 2 was greater than 1, although this difference was not statistically significant (Table 1).
According to the findings, 8.7% of the subjects had eating disorders, the average score of eating disorders in men was 7.78±7.97 and in women, it was 9.08±9.08 which was not statistically significant (p=.21).
Based on the correlation coefficient, a statistically significant relationship was observed between depression score, anxiety score, stress score, and an overall score of mental disorders with an eating disorders; In such a way that with the increase of each of these cases, the score of eating disorder also increases (Table 2).
DiscussionEating disorders can affect the physical health and mental function of individuals, therefore, due to their importance and impact on quality of life, the present study was conducted to investigate the nutritional pattern with the psychological status of adults during the COVID-19 epidemic. The results showed that eating disorders have a direct relationship with anxiety, stress, and depression.
The findings by al-Musharaf et al. study revealed that during the COVID-19 epidemic, the tendency to eat emotionally was associated with more anxiety and depression, and the scores of anxiety, depression, and stress were highly correlated, and also were associated with worse sleep quality, shorter sleep duration, less physical activity, and more sitting time. Also in this study, emotional eating was more common among young women during the COVID-19 epidemic, so compared to men, women are more prone to abnormal eating patterns as well as mental health disorders. Therefore, women are more likely to get health problems related to eating disorders, which may be exacerbated by this epidemic.19
In the current study, mental disorders were observed more in women than men. In a study by Elsherbiny et al., they reported an increase in symptoms of anxiety, depression, and stress during the COVID-19 epidemic,20 and the findings showed that people with pre-existing mental disorders had more severity of symptoms and psychosocial stress in stressful conditions such as quarantine time during the COVID-19 epidemic.19,21 One of the main challenges for general mental health and mental disorders during the COVID-19 epidemic is the physical distance and in some cases self-isolation. Physical distance also increases the likelihood of experiencing isolation and loneliness. Loneliness and isolation are widely associated with risk factors for psychological problems as well as the development and maintenance of eating disorders.22 Valentin flaudias showed in his research that there is a strong relationship between problematic eating behaviors and stress-related to quarantine, so that the more stress related to the COVID-19 epidemic, the more problematic eating behaviors are, as well as the reduction of social interactions and disruption of daily activities during this period may increase negative effects such as stress, and on the other hand, these changes may cause a wide range of negative effects, such as boredom and frustration, which promotes problem-eating behaviors. On the other hand, time stress quarantine is most likely associated with overeating, which is consequently associated with higher levels of anxiety and depression.21
During the COVID-19 epidemic, the symptoms of eating disorders are exacerbated due to several symptoms, including the availability of certain foods, as well as the increased stress, anxiety, and depressive symptoms that result from social distancing measures.23 In agreement with these findings, Castellini et al. reported that eating disorders increased during the quarantine period of the COVID-19 epidemic, and among the patients with previous overeating, their overeating intensified.
On the other hand, they found that during quarantine during this period, the recurrence of pathological eating behaviors disrupt the recovery process of patients with eating disorders.24 Furthermore, due to the potential decrease in exercise, increase in overeating, and restrictive behaviors during this period, there are psychological and adverse health consequences for the general population. Therefore, it is very important to provide more psychological support to people with eating disorders during this period.23 The results of another study showed that eating disorders were more likely to worsen during quarantine and that patients who noticed an exacerbation of the disorder were more likely to have future concerns such as access to medical care, maladaptive reactions, anxiety symptoms, and depression confronted adverse situations and family conflicts.25 Quarantine, on the other hand, is consistently associated with negative mental health outcomes, and being restricted in this way may reinforce irregular eating behaviors, including overeating.26
Brown et al. reported that during the COVID-19 epidemic, eating disorder symptoms could be improved by focusing on self-efficacy and risk management. However, many previous studies have suggested that COVID-19 may accelerate or intensify eating disorders.26 Screening high-risk individuals and risk factors as well as providing purposeful intervention and counseling on environmental stressors caused by the COVID-19 epidemic and quarantine may help reduce problem-eating behaviors, especially in vulnerable individuals.21
ConclusionThe prevalence of the COVID-19 pandemic has had psychological effects and it has increased stress and anxiety. Among these, one of the most important aspects affected by these mental disorders is eating disorders. Considering that eating disorders were observed with increasing mental disorders (depression, anxiety, stress); therefore, it seems necessary to increase people's awareness of anxiety and stress control methods during the corona epidemic. With the necessary training through mass media to prevent its adverse effects on nutrition.
LimitationOne of the limitations of this research is the non-cooperation of research samples. Due to the epidemic conditions of the COVID-19 pandemic, it was not possible to complete the questionnaire face to face, so the samples were collected through virtual networks, which caused problems in delaying the response of the samples.
FundingThere is no funding for the present study.
Ethical considerationsThe study is approved by the ethics comitte of Sabzevar University of Medical Sciencewith the ethics code of IR.MEDSAB.REC.1399.067. written informed consent was obtained form participants.