Granulomatosis with polyangiitis is a systemic disorder that is characterized by necrotizing vasculitis of small and medium vessels.1 The respiratory system is most affected in limited forms of the disease, however, lower respiratory system, systemic vasculitis, and necrotizing glomerulonephritis are the characteristic components of the disease triad.2 Impact to the central nervous system is rare and may only occur with meningeal involvement.
A 67 year-old caucasian female patient resorted to the emergency services reporting severe headache, fainting sensation, and a feeling of blocked ear, all of which within a two week evolution period.
The patient has a relevant clinical history of granulomatosis with polyangiitis, diagnosed approximately 40 years ago, with impact restricted to the upper respiratory tract (nasal mucosa).
A computerized tomography reveals right otomastoiditis, and ischemic leukoencephalopathy, thrombosis of right lateral sinus.
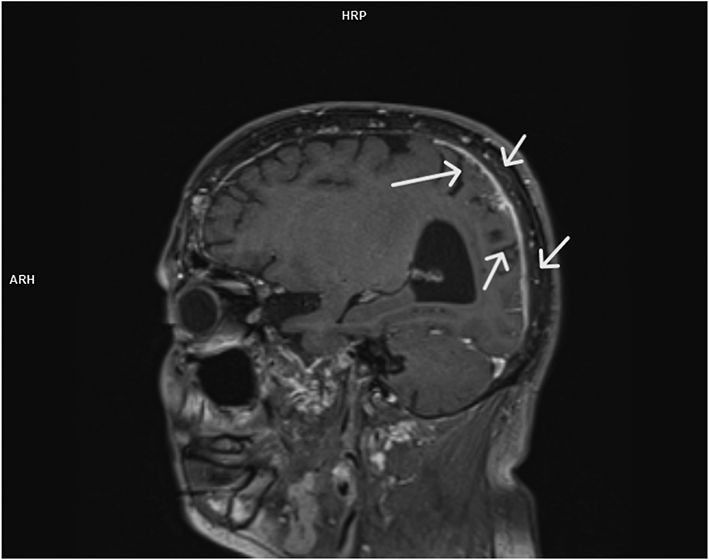
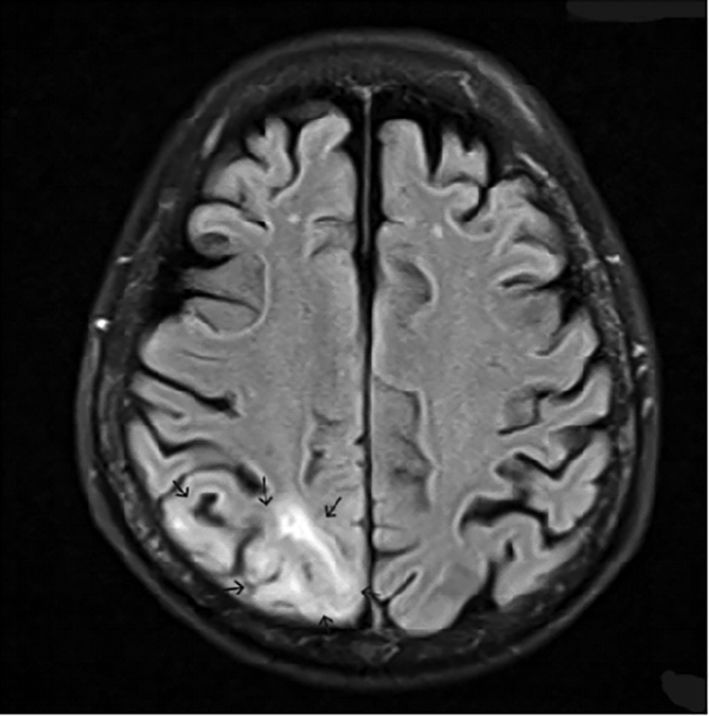
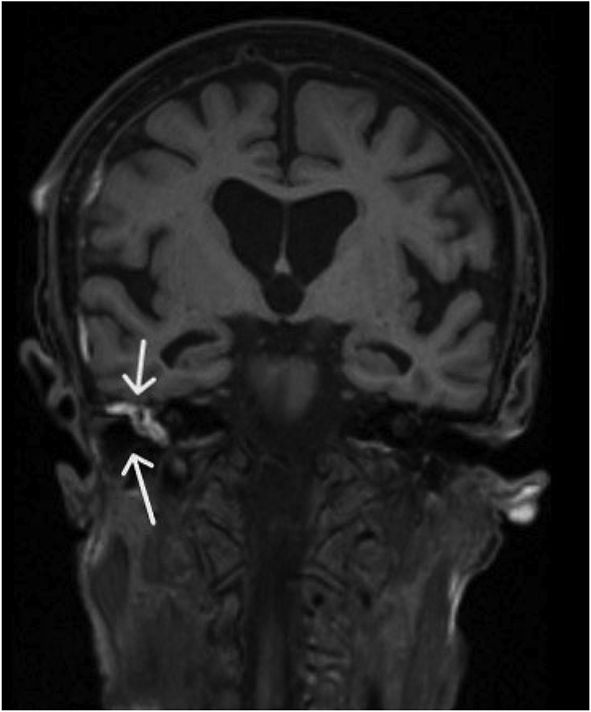
For added clarify and confirmation, a Magnetic resonance imaging (MRI) with gadolinium was executed. T1 showed involvement of the central nervous system by granulomatosis with polyangiitis.
Anomalous pachymeningeal dural enhancement and leptomeningeal involvement on occipital and parietal right lobes (Fig. 1 and 2, arrows), with homolateral occipito-parietal subcortical edematous component (Fig. 3, arrows) and right otopathy (Fig. 4, arrows).
The patient started treatment with corticosteroids 1mg/Kg/day for 4 weeks, along with rituximab, with significant improvements to the symptoms.