Male, 77 year-old, initially admitted on the emergency service after progressive dyspnea and productive cough with 5 day evolution. Diagnosed with global respiratory failure secondary to a COVID-19 bilateral pneumonia requiring hospitalization and non-invasive ventilation in the first 48h.
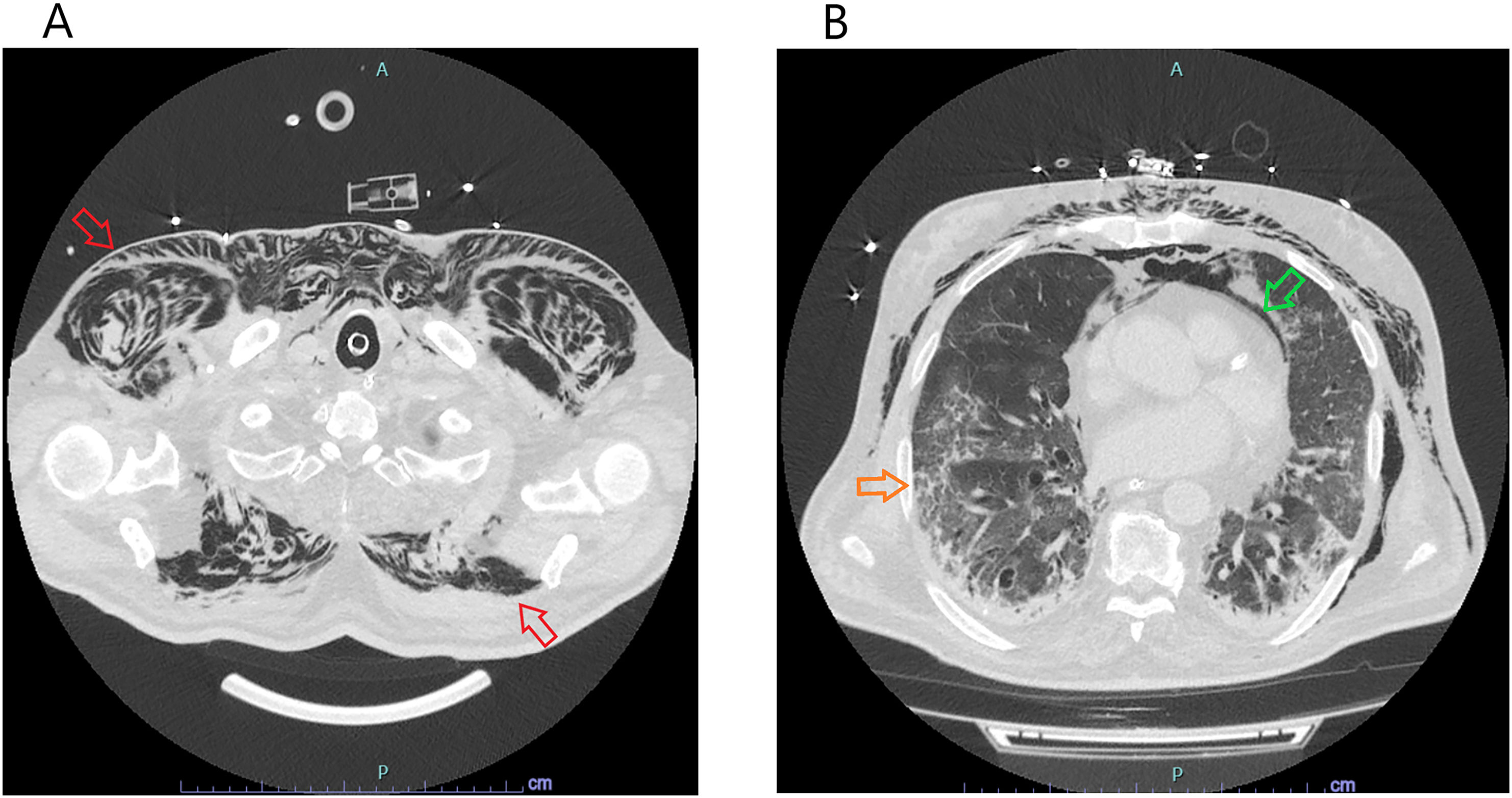
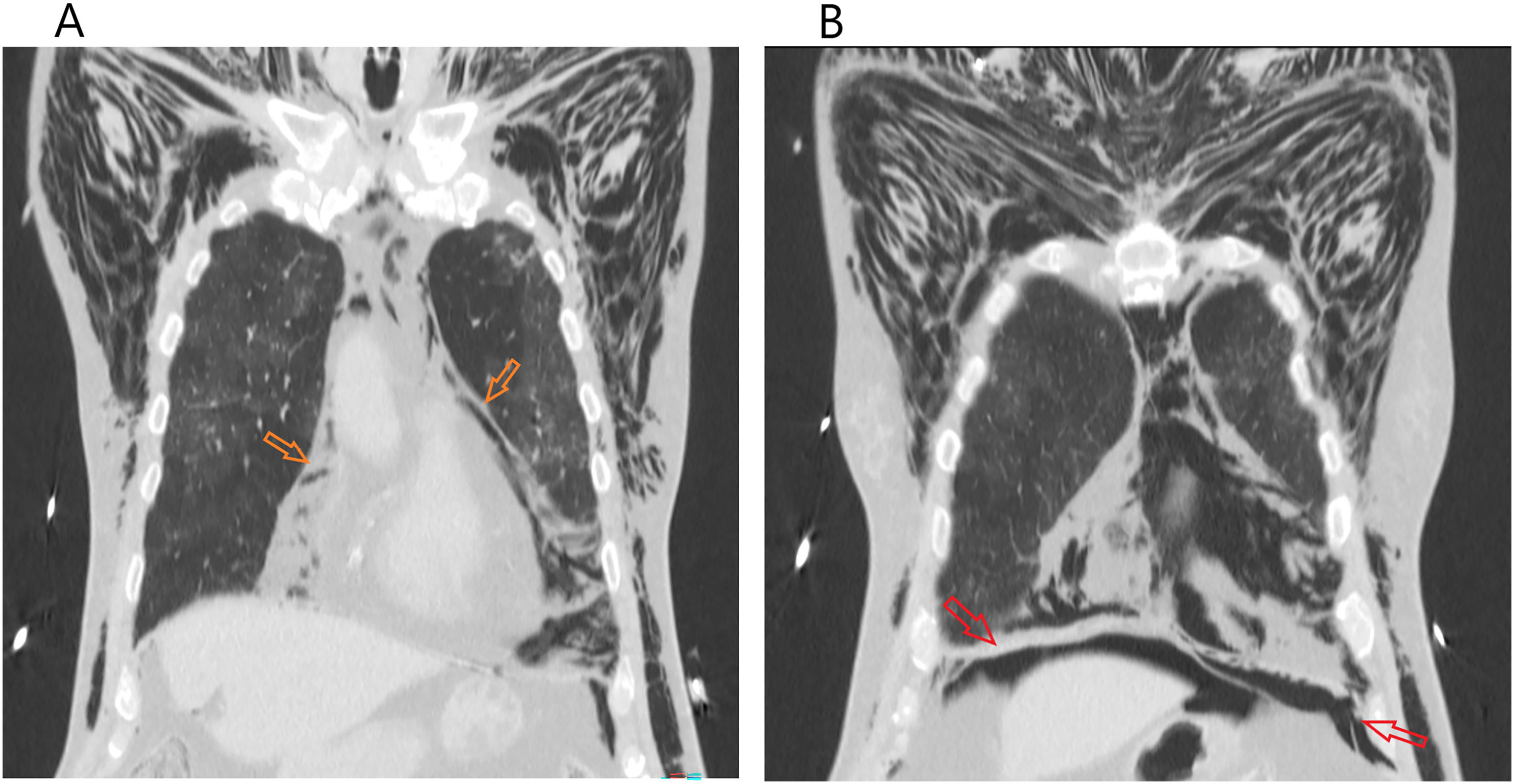
Worsening of severe respiratory failure with no significant response to medical therapy (antibiotic and corticosteroid) required escalation of care, transfer to intensive care unit and endotracheal intubation. Then, after 4 days, development of significant cervical subcutaneous emphysema (Fig. 1A) raised suspicion of potencial air trapping, with confirmation of sachular bronchiectasis, severe pneumomediastinum (Fig. 1B and Fig. 2A) and discrete pneumoperitoneum (Fig. 2B) in subsequent thoracic CT-scan. Notably present was also the characteristic COVID-19 pneumonia pattern – diffuse peripheric ground-glass opacity (Fig. 2B).
Thoracic CT scan (axial plane) revealing extensive subcutaneous cervical and thoracic emphysema (red arrows) with discernible muscular fibres dissection. Green arrow pointing to finding of predominant anterior pneumomediastinum. COVID pneumonia typical peripheral consolidation with ground-glass opacification (orange arrow).
Unfortunately, this patient didn’t survive this conglomeration of complications, denoting the difficulty between maintaining adequate ventilation while attempting to reduce airway pressure to permit some reduction of trapped extrapulmonary air.
Realization of invasive mechanic ventilation is associated with the risk of several complications, increasing with higher positive pressures required to maintain adequate ventilation of selected patients with severe ARDS or other entities. Of these, subcutaneous emphysema and pneumothorax are the more frequently observed, even more so than on the lower risk non-invasive therapy.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.