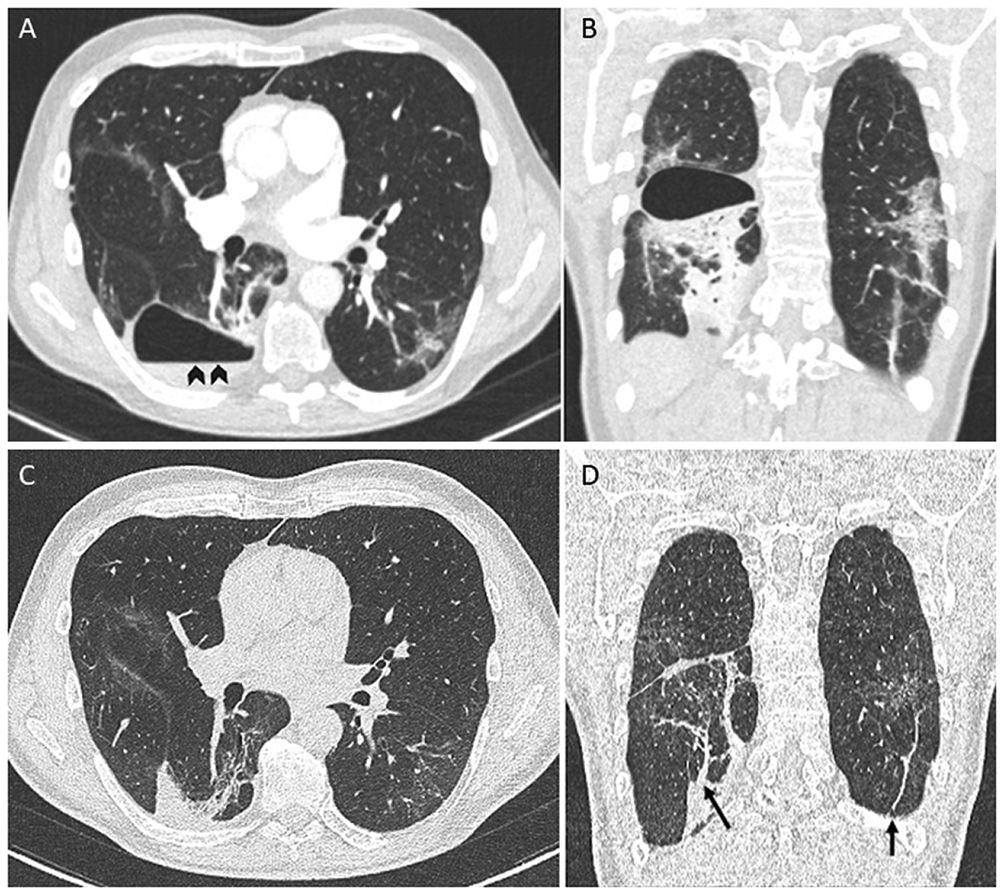
A 61-year-old man with no significant medical history presented to the emergency department with worsening dyspnea a week after close contact with someone who had COVID-19. He was unvaccinated. He was hypoxemic, and the chest radiograph showed bilateral opacities consistent with COVID-19 pneumonia and tested positive for RNA from SARS-CoV-2. Blood tests showed raised inflammatory markers. Computed tomography (CT) of the chest demonstrated bilateral ground-glass opacities. The patient was hospitalized and treated with high-flow nasal oxygen therapy, dexamethasone, and sarilumab. His clinical status improved, and he was discharged home after 1 week of hospitalization. Three weeks later, he presented again with worsening dyspnea, fever, and pleuritic chest pain. A CT pulmonary angiography ruled out pulmonary embolism (Fig. 1A, B) but demonstrated a thin-walled cystic lesion with an air–fluid level (Fig. 1A, arrowheads) that suggested an infected pneumatocele. The patient was managed conservatively with amoxicillin/clavulanic acid for 3 weeks. During the follow-up, the patient reported the disappearance of symptomatology. A subsequent CT performed 8 weeks after the diagnosis showed complete resolution of the pneumatocele (Fig. 1C, D) with persisting subpleural and parenchymal bands (Fig. 1D, arrows).
None.
Potential conflicts of interestJ.P. has been a consultant for Pfizer, MSD, Gilead, and Novartis. Other authors: No reported conflicts.
None