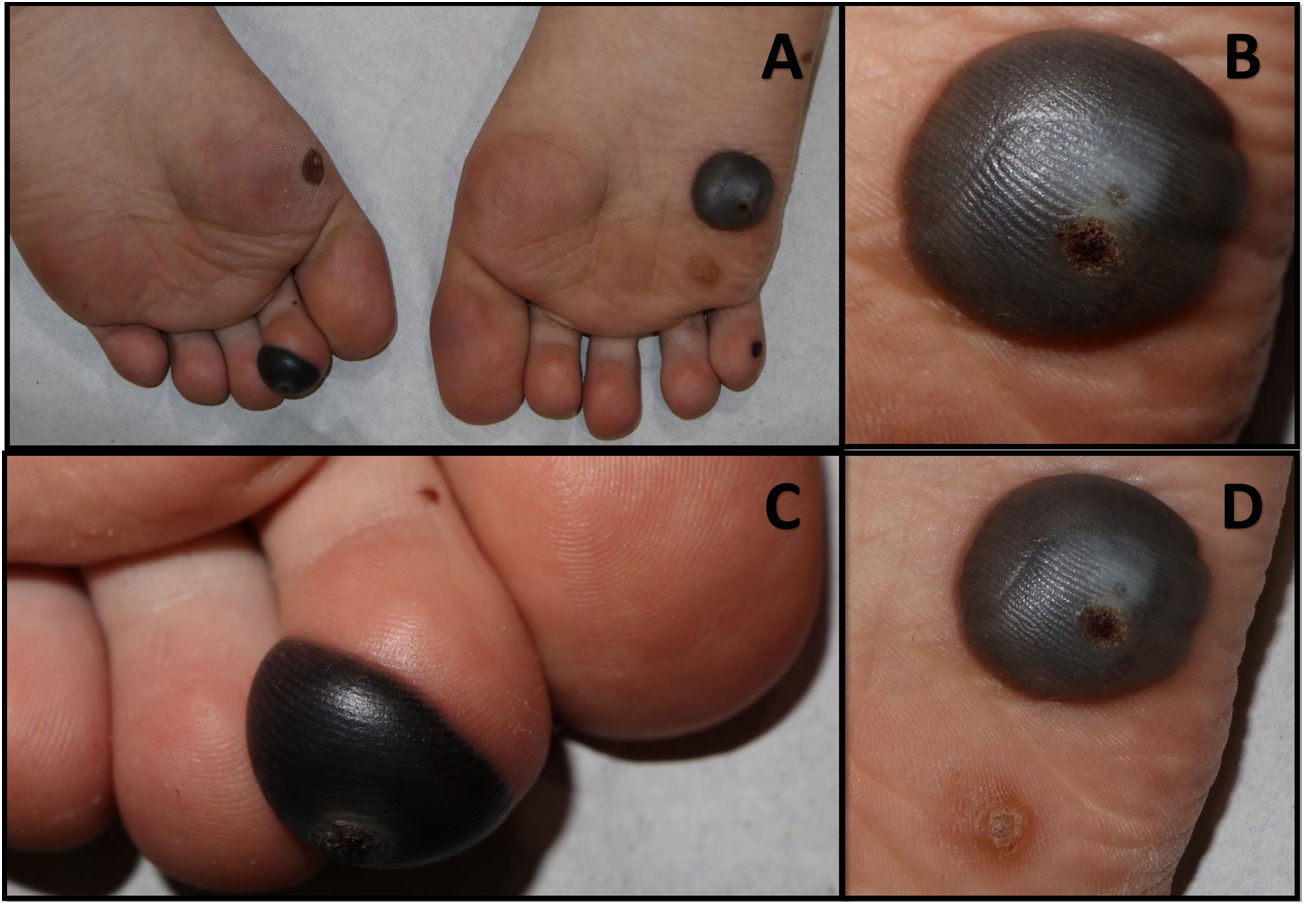
A previously healthy 15-year-old boy, presented with a 14-day history of painful lesions on his feet that limited his mobility. He denied prior trauma or any topical ointment application but he had been recently diagnosed of viral plantar warts. He denied any systemic symptoms and no relevant personal either familiar medical history was found. On physical examination, several hemorrhagic blisters were found on both plantar areas (Fig. 1A). They were tense bullae, without surrounding erythema, and all of them were centered by a hyperkeratotic lesion (Fig. 1B, C). Moreover, another hypertrophic papule was found in the plantar aspect of the right fourth toe, presenting black hemorrhagic dots (Fig. 1D). No other lesions were found on physical examinations. No stigma of any other dermatologic condition was present.
Clinical image: A. Hemorrhagic blisters located on both plantar areas. Two tense blisters B. Detail of tense bullae in right sole; note the hyperkeratotic lesion corresponding to the viral wart C. Detail of the lesion on the plantar aspect of the second left toe with a viral wart on top. D. Tense hemorrhagic bullae located on the upper part of one hyperkeratotic papule with black dots compatible with an untreated wart.
Our patient had been previously diagnosed of plantar warts and had been treated with cryotherapy. Drainage was performed and followed by pain relief. Verrucae plantaris (plantar warts) are common cutaneous lesions of the plantar aspects of the foot that are causes by human papillomavirus (HPV).1 The majority of cases occur in children and adolescents, but, other populations, such as immunocompromised patients are at increased risk for acquiring them.2 Numerous treatment options exist and each therapeutic method has been met with varying rates of success and adverse effects.3 Cryotherapy works by freezing the wart, causing cell damage and leading to a local inflammatory response that can be responsible for blistering. Owing to the generally benign course of plantar warts, treatment should be pursued if symptomatic or psychological distress, as most plantar warts resolves spontaneously within 2 years.1,3
Ethics approvalThis article has been approved by the Ethics Committee of Hospital General Universitario Gregorio Marañón (CEIm).
Consent for publicationPatient and his legal tutor gave permission to the publication of this article and its content. Informed consent was obtained.
Availability of data and materialPublished data have been reviewed and accepted by the patient and his legal tutor. Clinical history and images shown in this article has not been previously published and are original and related to the case presented.
FundingThe authors have not received any financial support or funding on this project.
Conflicts of interestThe authors have indicated no significant interest with commercial supporters.