Objective: Prove that conducting complementary studies at laboratories and imaging studies are unnecessary in first-time unprovoked seizures, since there is no change in the evolution and prognosis of the disease, as well as the study of our population, the incidence rate and the proportion of our patients that have been studied and given maintenance treatment, so it can be determined whether or not our population should follow the suggestions of the American Academy of Pediatrics and the Spanish Pediatric Association.
Methods: An observational study, including patients diagnosed with first-time unprovoked seizures. They were followed up on by the emergency department and information was collected from their clinical history and compared with the results of the different studies between patients that suffered just one seizure and the ones that had recurrent seizures.
Results: Thirty one patients were included, 14 males and 17 females. The average age was 5.5 years old. The 100% of patients were studied, and the groups were compared. The significant study was the electroencephalogram (EEG) with a p=0.02 (significance p<0.05), incidence of 41%.
Conclusions: The study and diagnosis of first-time unprovoked seizures is based on clinical manifestations. The EEG is important in the study and classification of unprovoked seizures. Our population has an incidence and recurrence rate similar to that in the bibliography, and for that reason, this study suggests that the diagnostic and therapeutic guidelines of the American Academy of Pediatrics and the Spanish Pediatric Association should be followed.
Introduction
About 5% of the patients who arrive at the emergency room are admitted with a seizure diagnosis.1 Management of these patients is determined by the first-contact pediatrician; they decide whether or not the patient gets exams/tests, is admitted and begins treatment.1 There is no standardized algorithm for the initial assessment of a patient who had a seizure for the first time, therefore a thorough case history and physical examination are required in order to determine additional lab and neuroimaging testing.2 Academic groups like the American and European Pediatrics Association suggest that neither additional testing or medical admittance are necessary for patients who had generalized unprovoked seizures.3
Currently we do not have studies describing our population; therefore we must follow the recommendations and guidelines given by these academic groups; for this reason we are conducting this research. Our main objective is to prove there is no need for additional lab and neuroimaging testing for patients who had generalized unprovoked seizures because it does not modify management, evolution or prognosis. Moreover, as specific objectives we will study the following: first-time generalized unprovoked seizure incidence at the “Dr. José Eleuterio González” University Hospital, percentage of patients who get additional procedures and/or additional studies, costs and length of hospital stays, the number of patients discharged with anti-seizure treatment and the most utilized anti-seizure in an acute event and subsequent to the event.
Methods
We designed an observational, descriptive, logitudinal, non-blind, prospective study.
We included in our population, patients of the “Dr. José Eleuterio González” University Hospital. We calculated the sample size using the finite population formula, with a result of 25 patients who had a first-time unprovoked seizure incidence in order to have significant results. This study was conducted over a period of 2 years; therefore we were able to include a total of 31 patients. We followed the patients during their medical visit and during their first follow- up appointment within the first month. The study and treatment was determined by the on-call doctor in the Pediatric Emergency Room at the University Hospital. We as researchers did not intervene in the decision making process. We obtained the information from their clinical files, gathering the following variables: age, gender, family history, perinatal history, use and type of anti-seizure in the acute event and subsequent to it and if they had studies performed, like a complete blood count (CBC), basic metabolic panel (BMP), lumbar puncture, electroencephalogram (EEg), computed tomography (CT) and magnetic resonance (MRI). The variables were compiled in a database created using Microsoft Excel®, later to be analyzed using statistical software SPSS® Statistics v. 20.0. Continuous variables will be expressed in median and standard deviation (SD) or ranges, on the other hand categorical variables will be described in percentages.
We included patients ranging from 6 months to 16 years old, with a first-time seizure diagnosis, generalized, unprovoked, about 5 minutes long, without focalization data after the event, with a normal neurological exam. We excluded patients with provoked seizures, history of previous seizures, patients with an epilepsy diagnosis, psychomotor development alterations, a previous brain injury, intoxication, gastrointestinal problems, vomiting and diarrhea, patients with dehydration data or central nervous system infection data and patients with an abnormal neurological exploration.
We divided the patients into 2 groups, patients who displayed recurrence in one group, and those who did not in the other group. We compared their lab and clinical tests’ results to verify that they were not anticipating immediate seizure evolution and/or complications. We defined immediate complications to the recurrence of seizures within the first month. We also divided the patients who received treatment from those who did not, in order to assess recurrence.
Results
Our sample size required a minimum of 25 patients; however, we managed to include 31 patients who met the inclusion criteria. We had 14 males and 17 females, with a median age of 5.5 years of age. Out of the 31 patients, there were 7 (22.6%) with a family history and 24 (77.4%) without, 3 (9.7%) had perinatal history and 28 (90.3%) did not.
We studied 31 patients as follows: We performed a lumbar puncture in 5 of them (0 abnormalities reported), 24 BMP (0 alterations), 26 CBC (2 altered results) and 24 neuroimaging scans (CT and MRI) with one altered result which was reported as a finding without being a cause of seizure. We performed an EEg in all 31 of the patients of which 14 were reported abnormal.
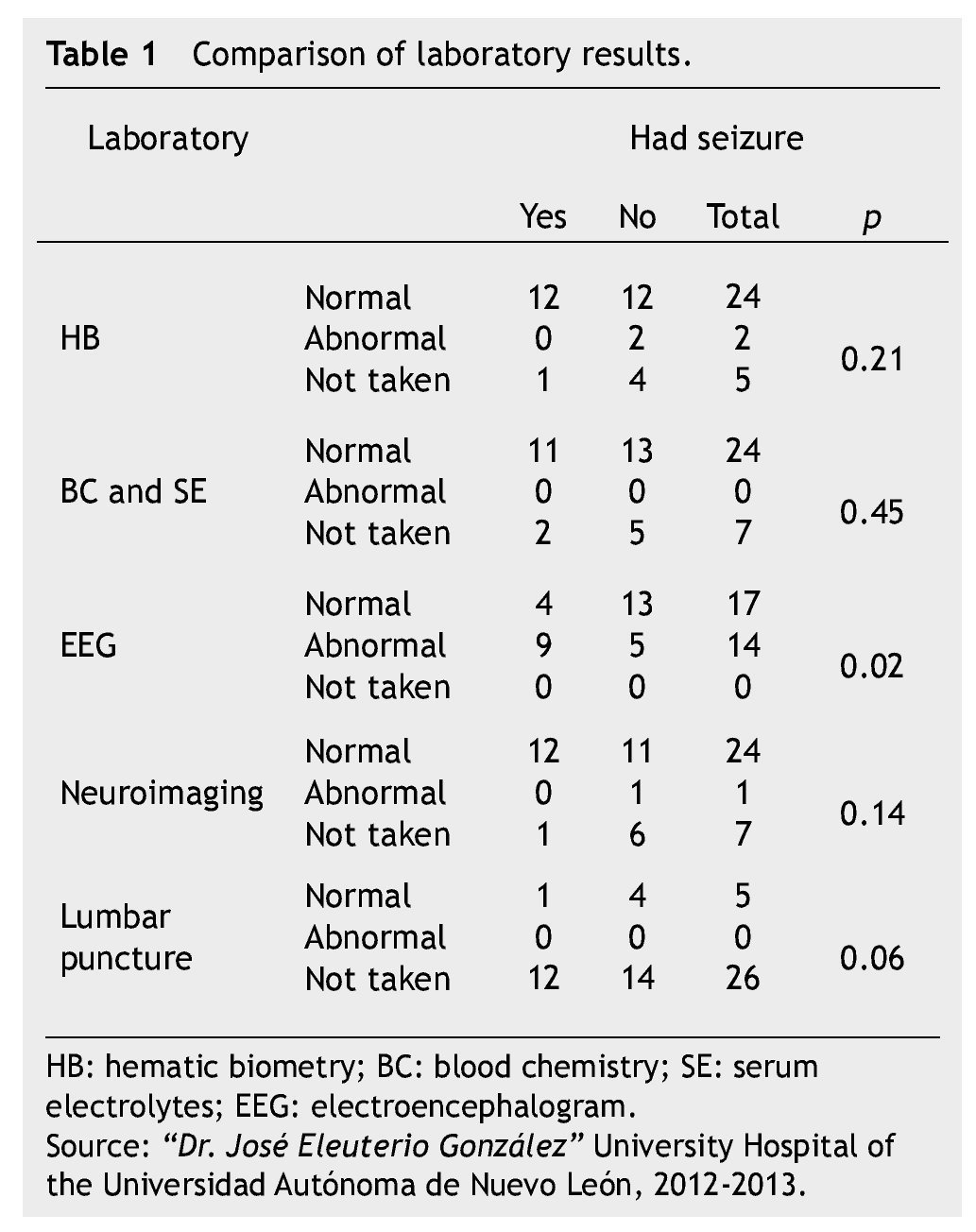
We compared the different test results from patients who experienced a recurrent episode to those patients who did not experience one, to verify if the results of the studies change or predict recurrences; of these the only one who showed significant results was p=0.02 the EEg (Table 1).
Out of the 31 patients who went to the emergency room, we began anticonvulsant treatment in 19 patients. Twelve patients were discharged conservatively, without anti-seizure treatment. Out of the 19 patients, 14 were given phenytoin, and 5 patients were given valproic acid.
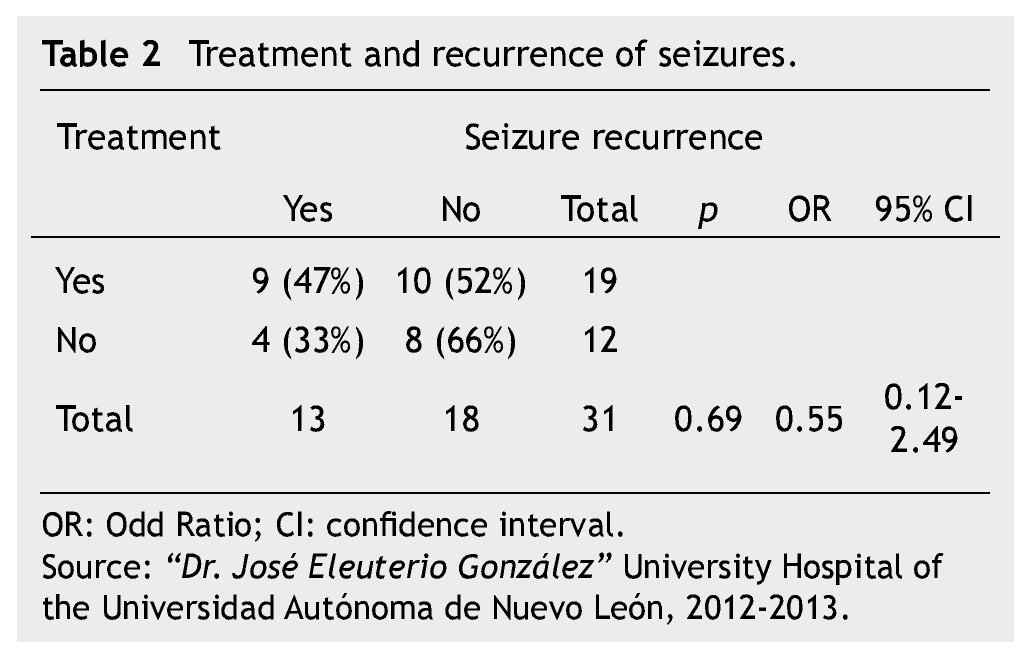
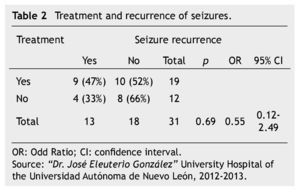
We compared seizure recurrence in patients discharged with treatment to those patients discharged without it, which showed a non-significant result with p=0.69, with an Odds Ratio (OR) of 0.55 and a confidence interval (CI) of 0.12-2.49, showing that the indication of chronic treatment is not a factor in protecting the patient against seizure recurrence (Table 2).
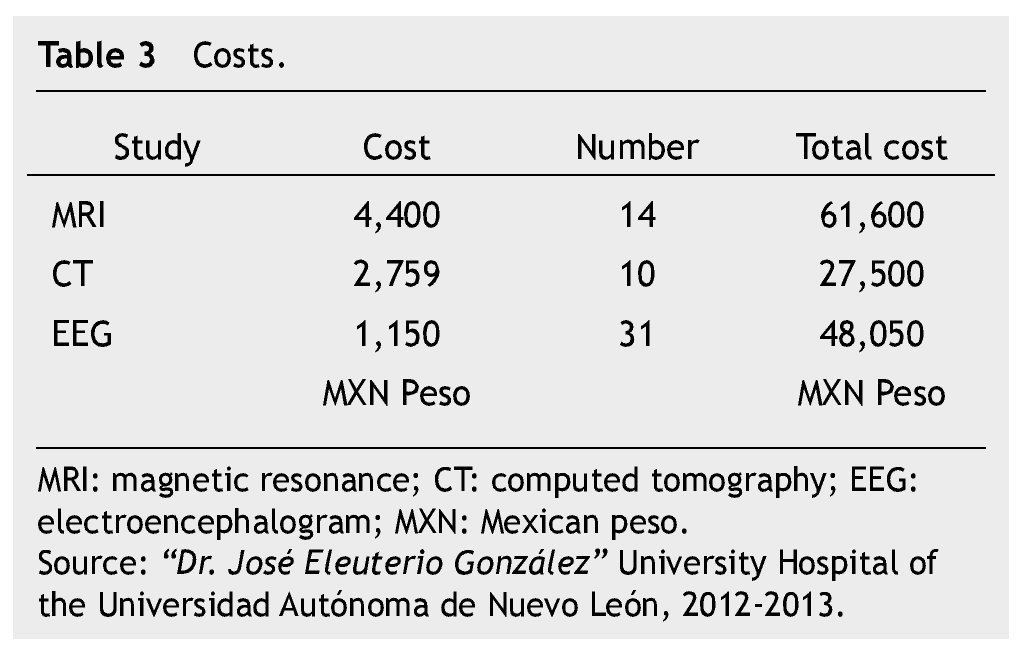
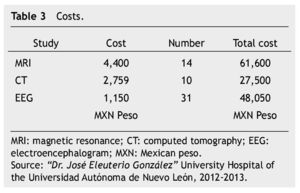
We researched inpatient costs and length, which resulted in a median of 1.5 days for the full study of seizures in patients who were admitted to the hospital. The costs are reported in Table 3.
Discussion
The results of the study were not very distant from those found in medical literature. With a similar reported incidence4 of 4 seizure episodes for every 1,000 habitants, which are said to be overstudied. This population was studied in full with at least one lab and/or clinical test, separating the EEg. Laboratory and neuroimaging tests were performed in 77% of the patients. None of them were reported with significant results for the diagnosis and prognosis of the disease, only the EEG had a significant p lower than 0.5, p=0.02.
Out of the 31 patients who had seizures, 45% showed an abnormal EEg, and from these patients with electroencephalographic alterations, 64% suffered a recurrence, compared to the rate reported in publications, which refers to a recurrence rate of 71%.4
The results regarding the recurrence of seizures treated with anti-seizure medication were similar to the data published. We prescribed treatment to 61% of the population. Of the patients who received treatment, 47% had a recurrence (29% of the entire population); this data can be compared to medical literature which mentions a probability of recurrence in a year of 19% to 26%. In this case the period of time is a variable, whereas in our study we just monitored the patients up to the first follow-up visit which is in a period of time no longer than 30 days.
This population showed a recurrence rate of 41% of the patients in the follow-up visit, compared with 3 other studies which recorded the recurrence rate at 2 years: 37%,5 54% (95% CI=46%-62%)6 and 57%, respectively.7
Conclusion
First-time seizure study and diagnosis is based on the clinical study. EEG plays a major role in the study and classification of unprovoked seizures. The use of medications and anti-seizure therapy after an unprovoked seizure is controversial; therefore each case should be personalized. The doctor should adequately study recurrence risk factors in order to start the patient on maintenance medication and compare the benefits with the medication’s adverse effects. Our population has similar incidence and recurrence rates to those reported in the references, thus this study suggests following the guidelines and recommendations made by the American and European Pediatrics Association concerning first-time unprovoked seizures.
Conflicts of interest
The authors have no conflicts of interest to declare.
Funding
No financial support was provided.
Received: February 2014;
Accepted: June 2014
* Corresponding author:
Pediatrics Department,
“Dr. José Eleuterio González” University Hospital.
Francisco I. Madero and Dr. Eduardo Aguirre Pequeño
Avenue, Mitras Centro, Z.P. 64460, Monterrey, N.L., Mexico.
Telephone: (81) 1041 1400.
E-mail address: mayela87@hotmail.com (M. A. Meza-Reséndiz).