Introduction: the incidence of primary bacteremia in patients on hemodialysis (HD) is reported to be from 2.5 to 5.5 cases per 1,000 catheter-day. The clinical impact is relevant and increases the cost of the HD Unit.
Methods: The present study is the first of 2 phases. It was conducted from January to December of 2012, and included all patients and nurses who were in the HD Unit. The prevalence of Gram-negative bacilli (GNB) and methicillin-resistant Staphylococcus aureus (MRSA) colonizing the nasal passages and the skin is described. Also, phenotypic association was sought by genus, species and sensitivities between colonizing bacterial strains and blood cultures with GNB and MRSA.
Results: the study included 70 patients and 10 nurses. The prevalence of nasal colonization in patients by GNB was 9% and 6% in the pericatheter, and no nursing GNB colonization was discovered. The prevalence of MRSA nasal colonization was 19% and 6% in the pericatheter for patients and in the nurses the nasal colonization was 50% and 10% in the hands.
We identified 29 cases of primary bacteremia. The primary bacteremia rate is 1.5 per 1,000 catheter-day or 0.4 episodes per patient per year.
Conclusion: We demonstrated a high prevalence of MRSA colonization in patients and nurses in the HD Unit. No relationship was found between primary bacteremia by GNB and patients and nurses’ bacteria colonization by the phenotypic comparison.
Introduction
The incidence of primary bacteremia in hemodialysis (HD) patients is reported to be between 2.0% and 4.5% per 1,000 catheter-day, or one to 2 episodes per patient-year. The use of HD catheters is a major mortality predictor in HD patients.1 Primary bacteremia is the most common cause of morbidity and the second most common cause of mortality in HD patients.2Staphylococcus aureus (S. aureus) causes up to 80% of vascular access infections and between 15% and 30% are caused by methicillin-resistant S. aureus (MRSA).3
Only a few studies have researched Gram-negative bacilli (GNB’s) nasal and skin colonization.4 there are reports in medical literature of a low incidence of catheter-related GNB infections, theoretically it is attributed to those who have a lesser adherence to vascular endothelial contrary to Gram-positive cocci.5,6 GNB, which colonizes nasal mucus and the pericatheter in patients in peritoneal dialysis has not showed a major association with infections in the dialysis catheter’s exit point, nor in the development of peritonitis associated with peritoneal dialysis.7,8 Conversely, a discrete association between nasal and skin colonization by GNB and vascular access infection in HD patients has been demonstrated.8,9
The number of hemodialysis-related primary bacteremias increased notoriously in our Hospital between 2010 and 2011, with a predominance of GNB in up to 60% of patients. On the other hand, as described in medical literature, MRSA is the causal pathogen of primary bacteremia with the highest morbidity; however its prevalence is unknown.
For this reason we focused this study on finding the prevalence of GNB and MRSA in patients and healthcare staff and their association with primary bacteremia developed in the HD Unit of the “Dr. José Eleuterio González” University Hospital.
Methods
The present study was conducted at the Renal Unit of the “Dr. José Eleuterio González” University Hospital, from January to December of 2012, including all patients and nursing staff in the HD Unit. We used the following operational definition for primary bacteremia: The presence of bacteria in the blood stream in a patient with a vascular catheter for over 48 hours, with positive hemoculture and clinical manifestation of infections without any other infectious focus.
The study was divided into 3 stages:
I. Supervision of a cohort of patients in the HD program in order to identify primary bacteremia cases and determine the rate of primary bacteremia per 1,000 catheter-day and patient-year episodes.
We identified the patients who developed fever during HD and we performed a hemoculture to monitor them in the bacteriology lab and verify GNB and MRSA isolations. We calculated the rate of primary bacteremia per 1,000 catheter-day and patient-year episodes.
II. Detection of patients colonized by GNB and MRSA in nasal mucous and pericatheter skin, also detection of nasal mucous and hands colonization in the nursing staff on the HD Unit; and determination of the prevalence of colonization in both groups. We performed a nasal swab culture and pericatheter skin in all patients in the HD Unit, and we performed nasal and predominant hand swabs in the healthcare personnel involved in the connection of patients in HD. Subsequently, we determined nasal and skin colonization prevalence in both groups.
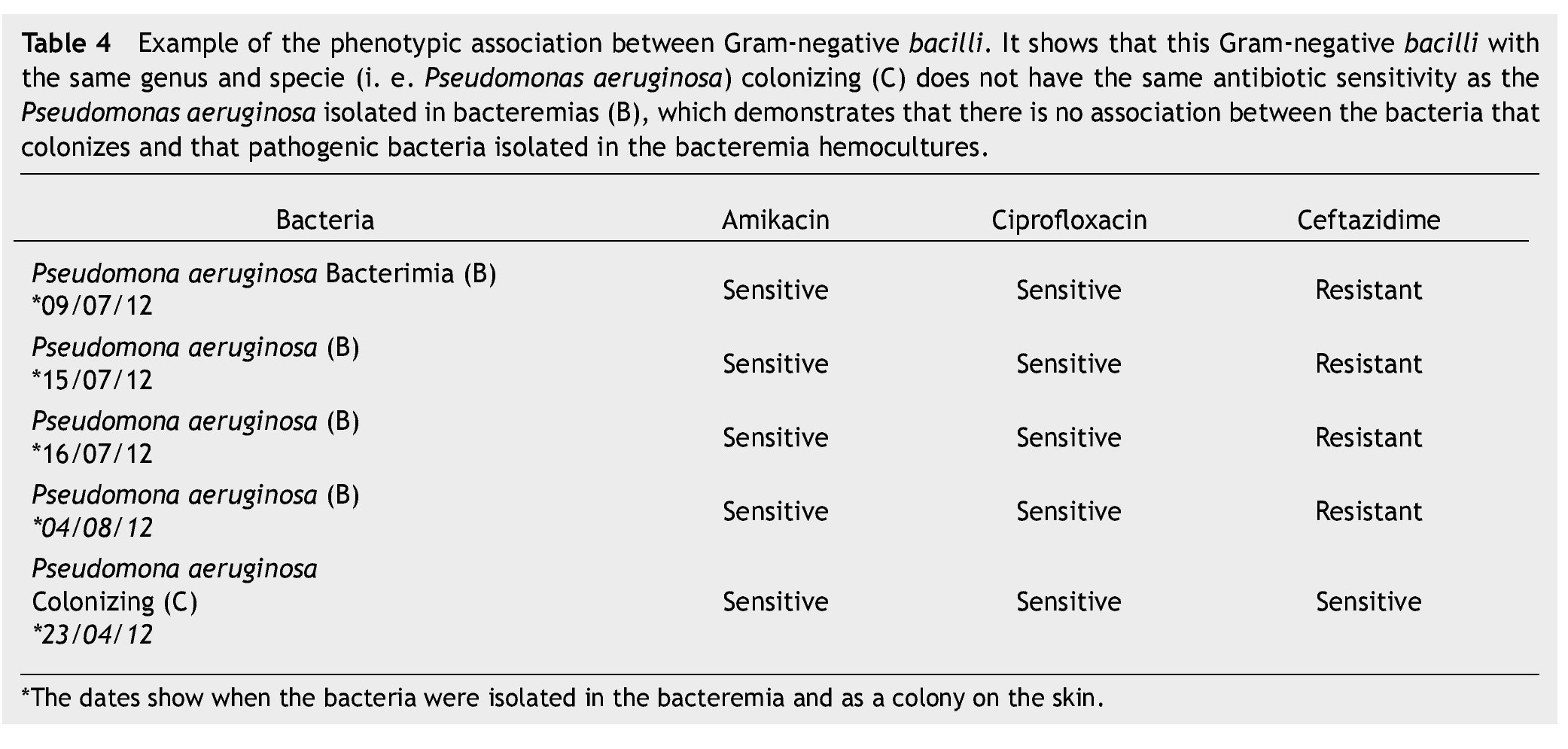
III. Determination of phenotypic association between GNB’s isolated from primary bacteremias and GNBs colonizing the nasal mucous and skin.
We identified bacteria genus and species in all bacteremia cases, as well as the colonizing strains, using conventional biochemistry performed by the clinical pathology lab. We carried out antibiotic susceptibility testing (AST) in the following GNBs: ceftazidime, ciprofloxacin and amikacin. In the S. aureus we performed the AST to cefoxitin and if it wasn’t sensitive to this antibiotic we determined its methicillin resistance. We searched for an association between GNB’s isolated from primary bacteremia and colonizing GNB’s through phenotypic comparison with genus, species and sensitivities described in the antibiogram. In a second stage of the same study we determined whether or not isolated MRSA’s were clones using pulsed field electrophoresis. The results were analyzed with descriptive statistics in frequencies and proportions.
Results
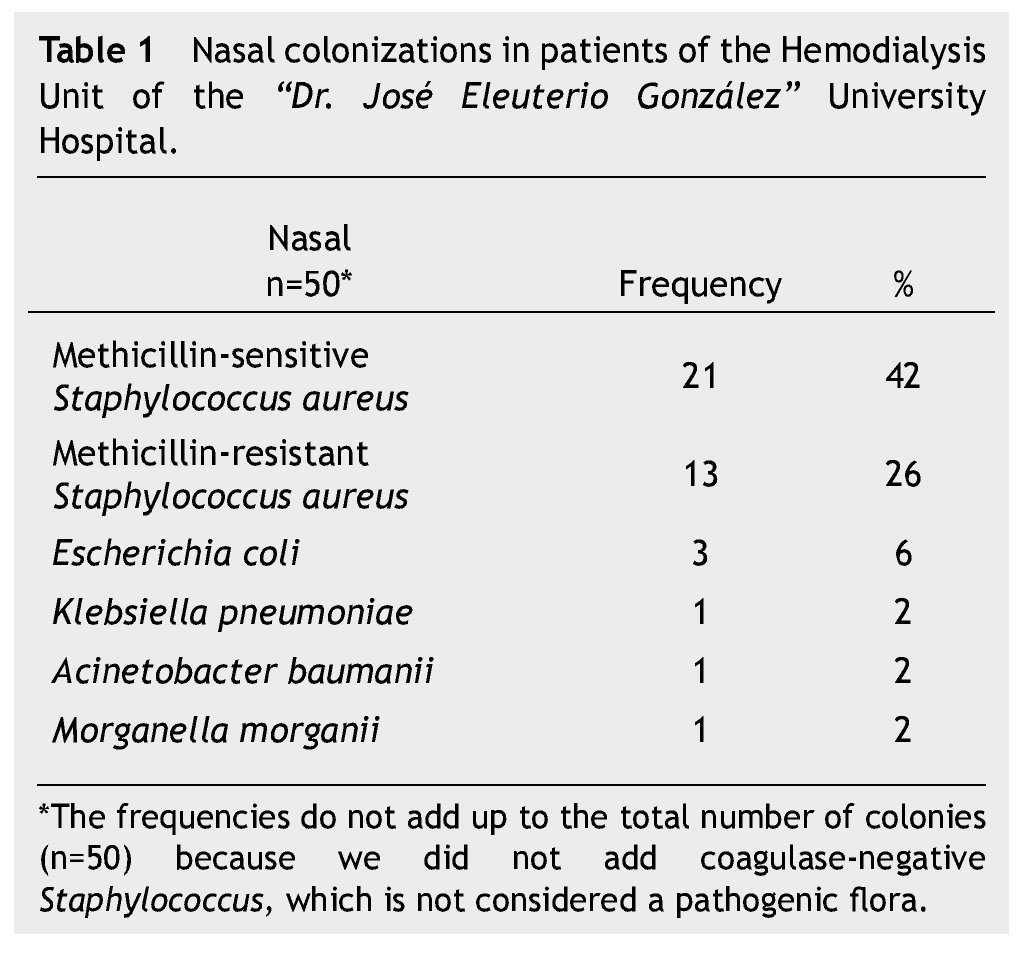
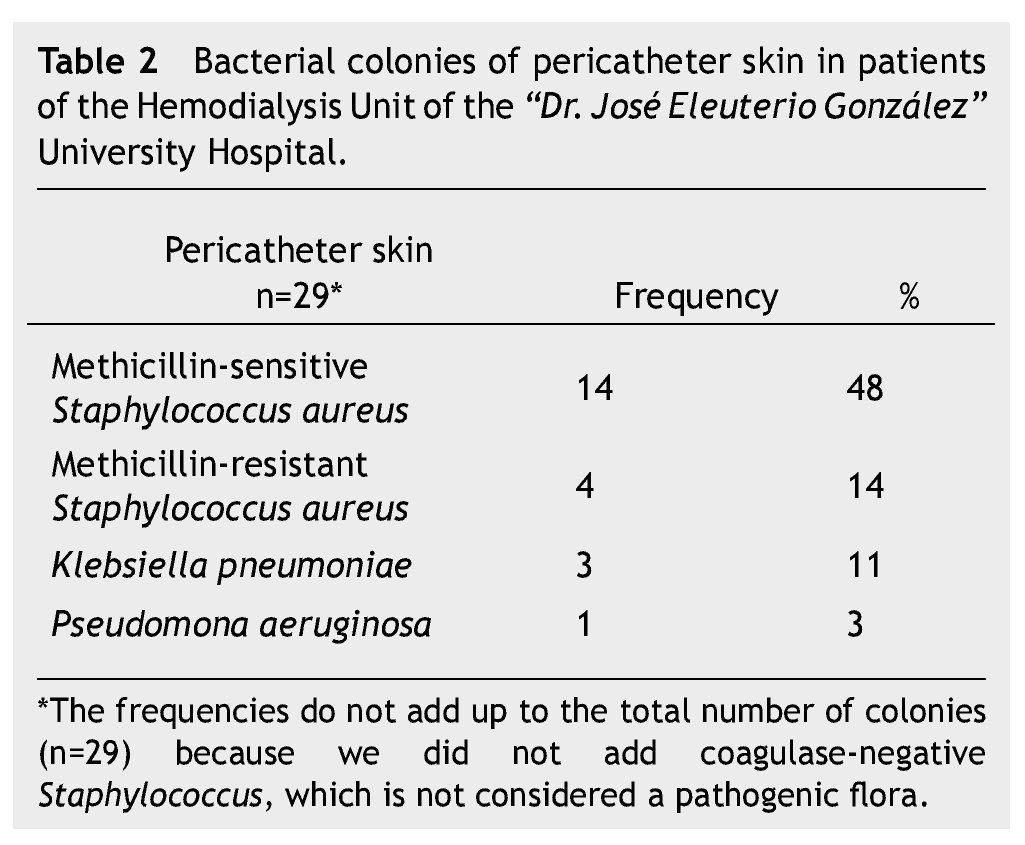
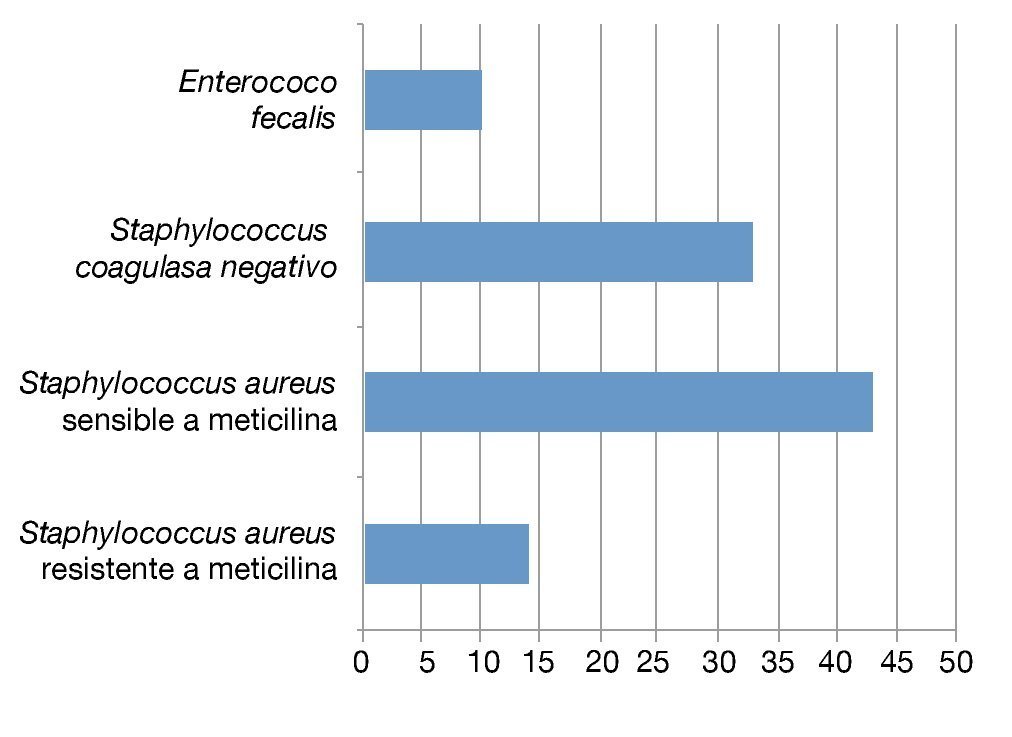
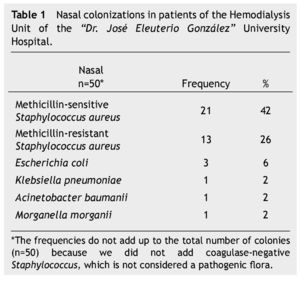
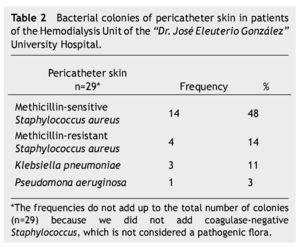
We conducted colonization cultures from each of the 70 patients in the HD Unit. We documented nasal colonization in 47 patients (67%) and 50 isolations because 3 patients had 2 bacteria colonizing the nasal mucous. Pericatheter colonization was evidenced in 27 patients (39%) and 29 isolations because 2 patients had 2 bacteria colonizing the pericatheter skin. The most relevant nasal and pericatheter skin-colonizing isolations can be found in tables 1 and 2.
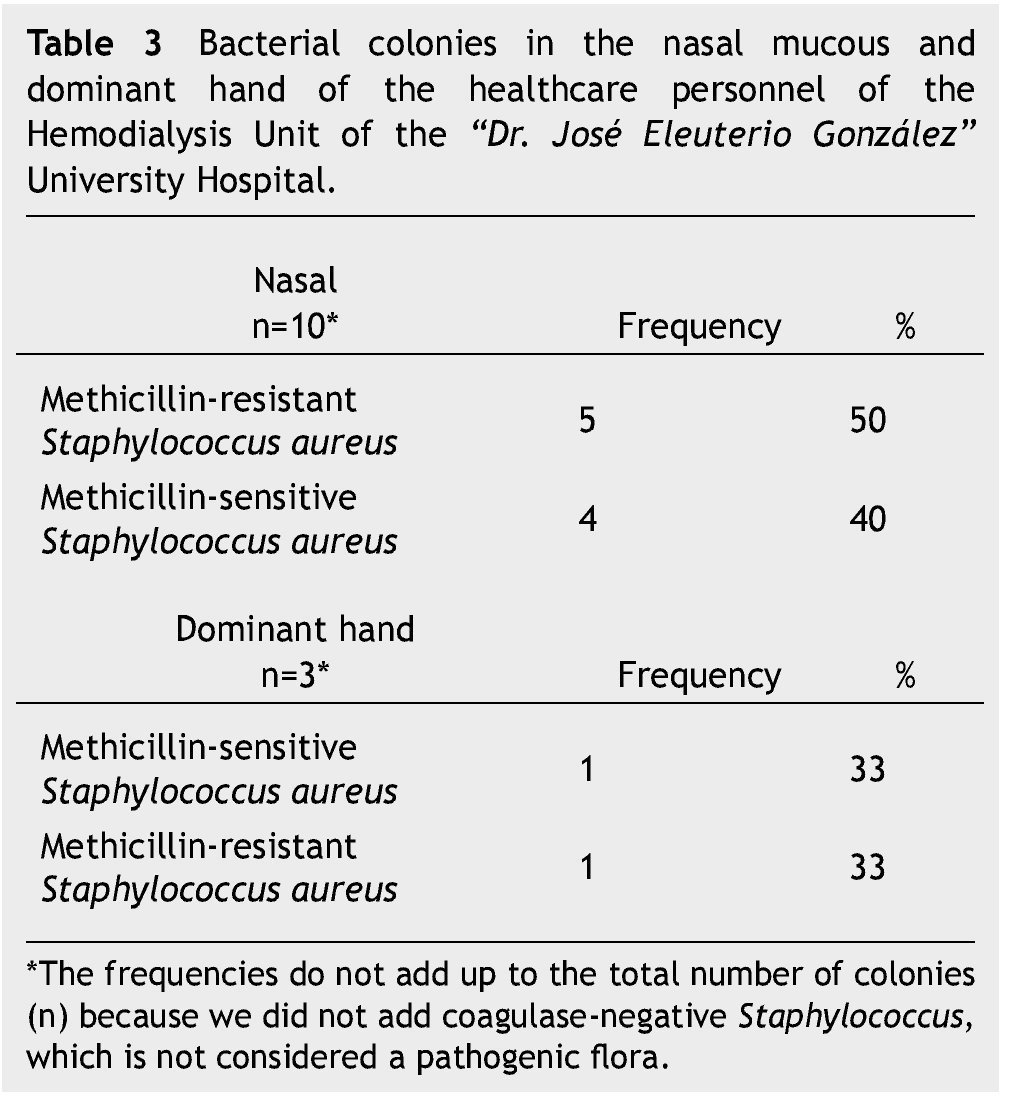
Regarding healthcare personnel in the HD Unit, we documented nasal colonization in 10 nurses (100%) and 10 isolations. We found colonization in the predominant hand in 3 nurses (30%) and 3 isolations. The most relevant nasal and predominant hand colonizations in healthcare personnel can be found in table 3. The prevalence of nasal colonization in patients by MRSA was 19% and by GNB, 9%; the prevalence in pericatheter skin by GNB and MRSA was 6% for both. Regarding the nursing staff, the prevalence of nasal colonization by MRSA was 50% and 10% in the predominant hand; we did not find GNB colonization.
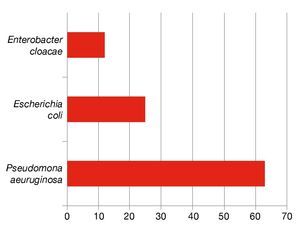
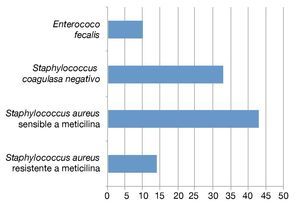
During the study we identified 29 primary bacteremia cases confirmed microbiologically. The rate of bacteremia caused by GNB was 28%, you can read each of the percentages on bacteremia-isolated GNBs in Figure 1. Primary bacteremias caused by S. aureus were 12 (67%) and 25% was by MRSA, you can read each percentage of bacteremia-isolated CGP in Figure 2. Primary bacteremia rate was 1.5 per 1,000 catheter-day or 0.4 episodes per patient-year. In the patients with isolations by GNB in their primary bacteremia blood cultures, none of them displayed phenotypic association with nasal mucous and skin (Table 4).
Figure 1 the percentage of each of the Gram-negative bacilli isolated from the primary bacterimias.
Figure 2 the percentage of each of the Gram-positive cocci isolated from the primary bacterimias.
Discussion
A low prevalence of GNB colonization in patients was demonstrated, with 6% and 9% for skin and nasal mucous respectively, similar to the rate described in medical literature. Prevalence of MRSA colonization was 6% and 19% for skin and nasal mucous respectively.10 In healthcare personnel, a prevalence of 10% in the predominant hand and 50% in nasal mucous was demonstrated, between both groups this means that at least one in every 3 individuals is an MRSA carrier.
Primary bacteremia rate was 1.5 per 1,000 catheter-day or 0.4 episodes per patient-year, lower than the rate reported in international literature.11 Bacteremias caused by MRSA were 10%, but there is no previous information regarding our grounds to compare to previous years. Primary bacteremias caused by GNB were 28%, representing a reduction of over 50% of the cases identified as GNB in the years 2010 and 2011, during which it was 60% of the total of bacteremias. The reduction of primary bacteremias by GNB during the present study with regard to the last 2 years is probably caused by hygiene actions performed by the nephrology department at the beginning of that year, including the standardization of asepsis of the pericatheter region with chlorhexidine, and having enough supplies for proper hand-washing, such as alcohol antibacterials and electronic-sensor sinks.
In conclusion, an association between carriers (patients) of GNB and primary bacteremias by GNB was not proved, which is consistent with other epidemiologic studies. In addition, a high prevalence of colonizing MRSA in patients and nursing staff in the HD Unit was demonstrated.
Conflicts of interest
The authors have no conflicts of interest to declare.
Funding
No financial support was provided.
Received: December 2013;
Accepted: June 2014
* Corresponding author:
Internal Medicine Department,
“Dr. José Eleuterio González” University Hospital.
Francisco I. Madero and Gonzalitos Avenue,
Mitras Centro, Monterrey, N.L., Mexico.
Phone: (81) 8389 1111, ext. 3243, 3107.
E-mail address: carlos_quinonez@hotmail.com (C. G. Quiñonez-Olivas).