Introduction: Amyloidosis is used to describe a range of disorders defined by extracellular deposition of abnormal protein fibrils. The larynx is the most common site of localized amyloidosis in the head and neck region and constitutes less than 1% of benign laryngeal lesions. Hoarseness is the most common symptom.
Objective: Prospective clinical evaluation of patients with localized laryngeal amyloidosis.
Clinical cases: Presented are 4 cases of patients with localized laryngeal amyloidosis who were treated at the Otolaryngology and Head and Neck Surgery Department at the “Dr. José Eleuterio González” University Hospital in Monterrey, Mexico. Three patients underwent phonomicrosurgery by direct microlaryngoscopy with the removal of the amyloid implantation using a cold knife excision with great results. In each patient the major site of involvement was the supraglottis with a small focus on the false vocal cord. A medical work-up, including a complete blood count (CBC), a basic metabolic panel, urinalysis, liver function test, chest X-ray and physical examination were performed to rule out the presence of systemic disease; no amyloidosis or signs of systemic disease were found. Congo red staining confirms the diagnosis of amyloidosis in all surgical specimens.
Conclusions: In laryngeal amyloidosis, the treatment should be directed toward the improvement of the voice and the maintenance of the airway.
Introduction
Amyloidosis is used to describe a range of disorders defined by extracellular deposition of abnormal protein fibrils. Amyloid deposits were first described by Von Rokitansky in 1842, and the term amyloid was first used by Virchow in 1851 to describe the reaction of this tissue to iodine and sulfate.1 Borrow and Neuman (1873) were the first to report laryngeal amyloidosis. Over 300 cases have been reported since then.2 Current classifications of amyloidosis are based on the biochemical nature of the protein subunit (Chastonay, Hurliman in 1986 and Lewis et al. in 1992). AL amyloidosis (derived from light immunoglobulin chains) is associated with systemic amyloidosis.
Fibrillar proteins have a characteristic pattern when observed under an electronic microscope after Congo red staining, displaying apple-green birefringence when examined with polarized light.3
The larynx is the most common site of localized amyloidosis in the head and neck region and constitutes less than 1% of benign laryngeal lesions.4 Hoarseness is the most common symptom. The male-female ratio is 3:1, with an age range between 8 and 80 years old, and a peak incidence occurring in the 5th decade of life.5-7
There are different treatments and resection methods for these lesions, though a few stand out, such as resection with a CO2 laser and cold technique. Radiotherapy has recently been described in cases where the lesions cannot be completely resected. Follow up is important in the long term, because these lesions have a high recurrence rate.3,4,8,9
Methods
Presented are 4 cases of patients with localized laryngeal amyloidosis who were treated at the Otolaryngology and Head and Neck Surgery Service at the “Dr. José Eleuterio González” University Hospital in Monterrey, Mexico.
A flexible nasal fiber laryngoscopy was performed on all of the patients. Lab studies were ordered to rule out the presence of a systemic disease: a complete blood count (CBC) and basic metabolic panel, urinalysis, hepatic function test, thoracic X-rays, and a full physical examination was performed, all of which were reported to be within normal parameters. Rectal or bone marrow biopsies were not performed. Maximum phonation time, voice handicap index, reflux symptoms (described by Belafsky et al.), and glottic function and features in all patients were measured.
A resection by microlaryngoscopy with cold technique on all the lesions was performed. Congo red stains were applied to all surgical specimens.
The approval of the ethics Committee of the “Dr. José Eleuterio González” University Hospital was obtained, as well as signed informed consents from all the patients.
Cases presentation
A laryngeal amyloidosis diagnosis was performed on 3 men and one woman, whose ages ranged from 14 to 67 years. The most common symptoms are: hoarseness, pharyngodynia, vocal pauses, and vocal fatigue. The duration of the symptoms before diagnosis was between 2 and 12 years.
Diagnosis and treatment were implemented to rule out systemic involvement; the results were negative in all patients.
Resections of the lesions by microlaryngoscopy with cold technique were executed, and samples were sent out for histopathology analysis. Congo red staining was used, where we were able to observe green birefringence through the use of the electronic microscope.
The results of the questionnaires conducted before and after the surgical procedure were documented. With the use of this technique we were able to observe favorable results in the subjective symptoms as well as in the maximum phonation time.
Case 1
A 67-year-old male, came to the Voice Clinic for the first time presenting hoarseness with an evolution of 10 years, progressive, vocal fatigue, glottic leak and inability to reach high notes. He denies any systemic diseases or smoking. He scored a glottic closure force index of 9, reflux index of 8 and quality of life index of 3.
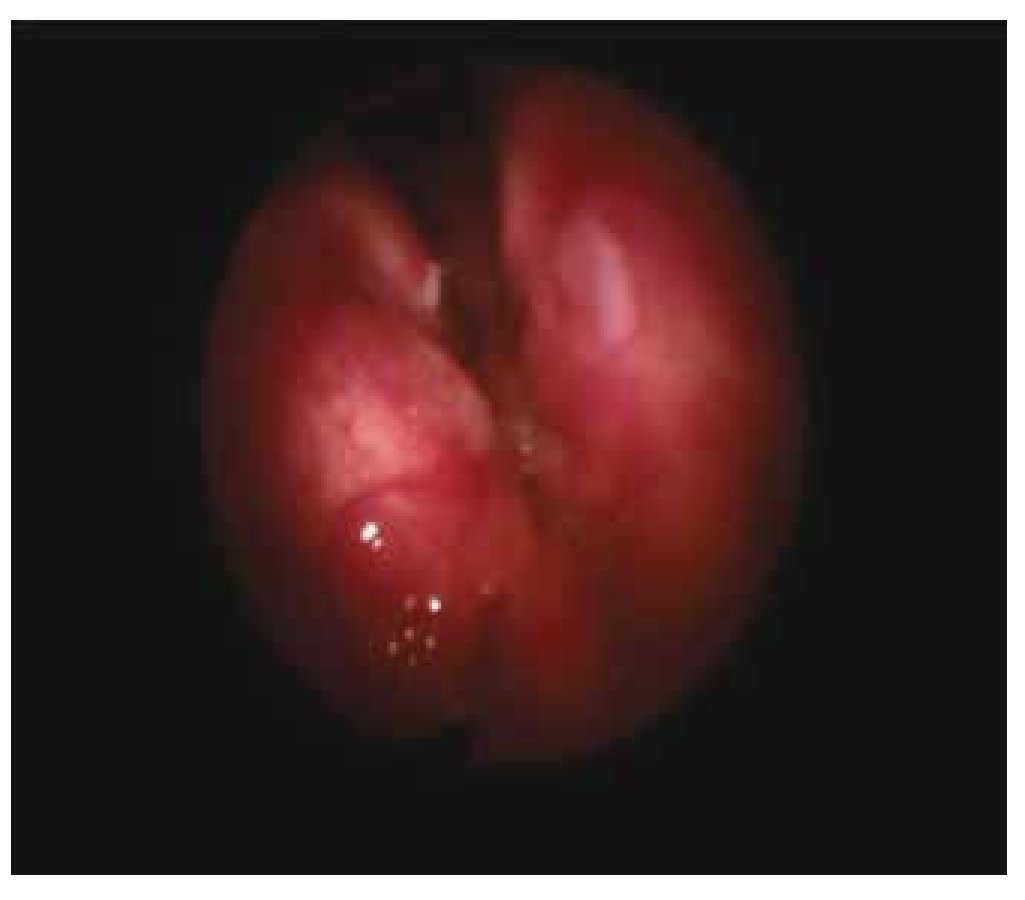
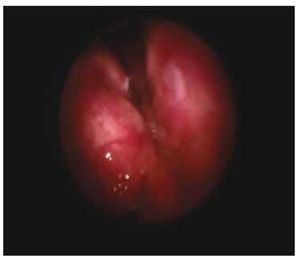
At the physical examination: Maximum phonation time was 17 seconds, S:Z ratio of 25:27. The videolaryngoscopy displayed an elevated lump towards the right false vocal cord and anterior commissure (Fig. 1).
Figure 1 Patient 1, first visit. An increase in submucus volume can be observed in the photograph, altering the anatomy of the false vocal cords at the supraglottic level.
Case 2
A 52-year-old female, teacher, came to the Voice Clinic as a result of hoarseness with a 3-year evolution, accompanied by vocal fatigue, vocal pauses and inability to reach high notes. She did not improve by resting her voice. She denies smoking or ethilism. She previously received steroids and antibiotics without improvement.
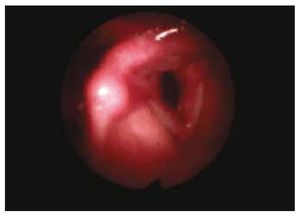
Her glottic closure force index was 12, reflux index of 17 and quality of life index of 7. Her maximum phonation time was 7 seconds, S:Z ratio of 5:3. We were able to observe a major glottis edema with the videolaryngoscopy (Fig. 2). A phonomicrosurgery with cold technique was performed, and the sample was sent for histopathological analysis with an amyloidosis report.
Figure 2 Patient 2, first visit. An increase in volume is observed in the left lower lip of the true vocal cord, creating premature contact upon glottal closure.
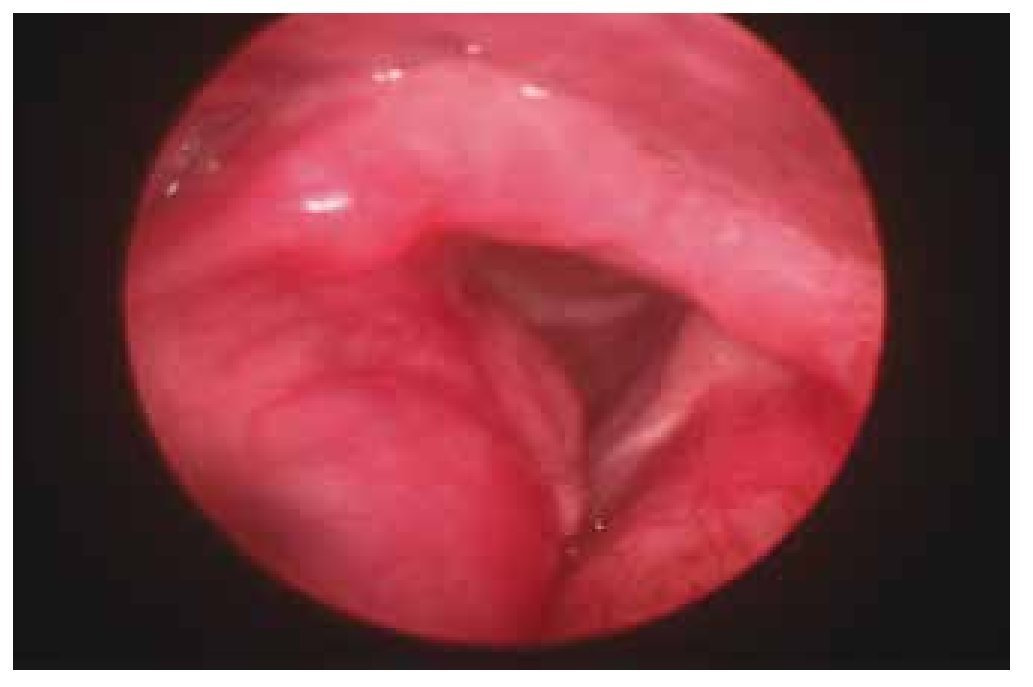
Post-surgically, she showed an improvement in her maximum phonation time to 12 seconds, a glottic force closure rate index to 4, reflux index to 4, and a quality of life index of 3 (Fig. 3).
Figure 3 Patient 2, one month post-surgery. A lessening of the increase in volume can be observed at the true vocal cords. There is now no premature contact upon glottal closure.
Case 3
A 33-year-old male, presenting hoarseness with an evolution of 3 years, accompanied by vocal fatigue, vocal pauses and inability to reach high notes, occasional ethilism and denied smoking.
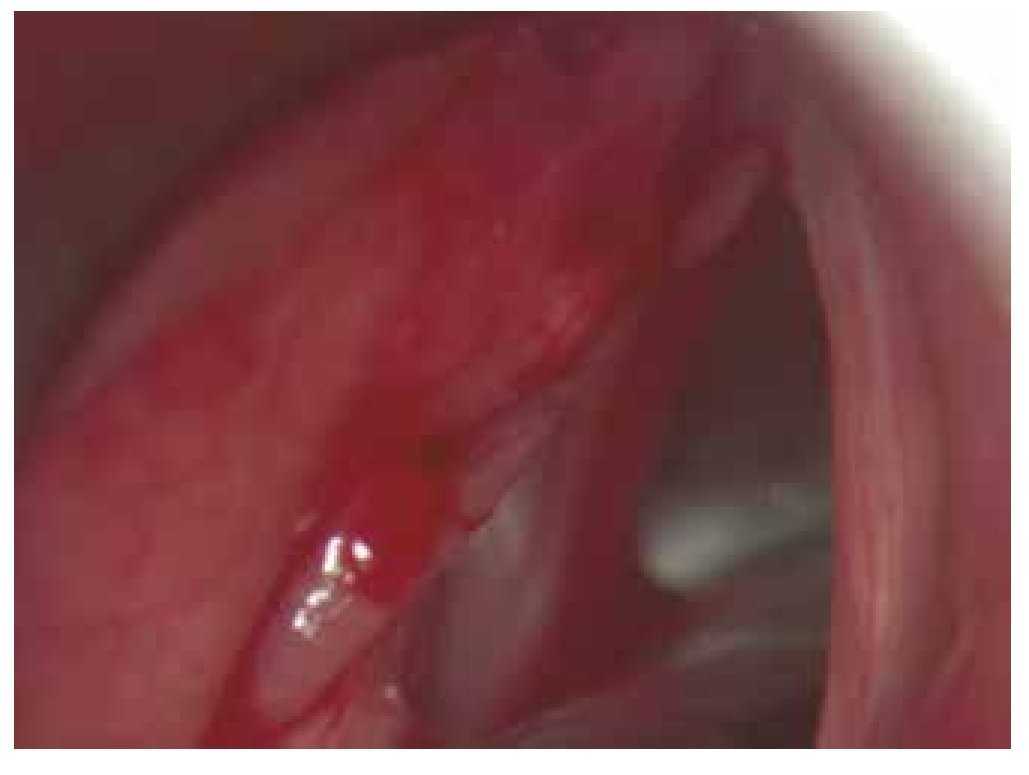
At physical examination: Glottic leak, a glottic force closure rate index of 19, reflux index of 25, and a quality of life index of 18, maximum phonation time was 9 seconds, S:Z ratio of 32:8. The videolaryngoscopy displayed an elevated lump towards the right false vocal cord which impedes glottic closure, with a wide glottal gap (Fig. 4). A resection using the cold technique was performed, and we confirmed a diagnosis of amyloidosis. Post-surgical data: Glottic force closure rate index of 10, reflux index of 5, quality of life index of 9, and maximum phonation time of 16 seconds (Fig. 5).
Figure 4 Patient 3, first visit. Increased exophytic volume can be seen, at the right level of the false vocal cords, which does not obstruct the glottal light. And a plain deformity of the right true vocal cord with premature contact and alteration of the chordal wave vibration.
Figure 5 Patient 3, one month post-surgery. There is no evidence of supraglottic lesions, or obstruction of glottic light.
Case 4
A 14-year-old male with hoarseness, with a 2-year evolution, progressive, with vocal fatigue and vocal pauses during conversation.
A videolaryngoscopy was performed, where we were able to observe a lump which deformed both false and true vocal cords, thus conditioning a premature glottic closure (Fig. 6).
Figure 6 Patient 4, first visit. Submucous lesions at the left false vocal cord level can be observed.
Glottic force closure rate index of 13, reflux index of 10, and a quality of life index of 6, maximum phonation time was 12 seconds, S:Z ratio of 17:12 seconds.
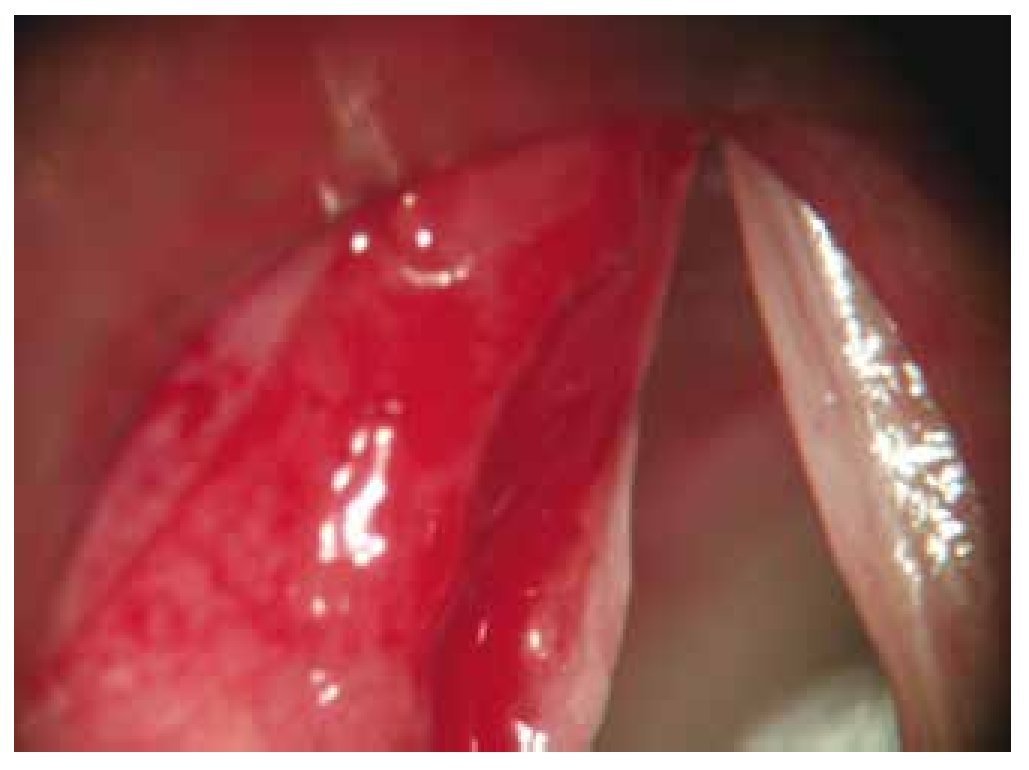
The same surgical procedure was executed, and we sent a sample for histopathological analysis. Post-surgical data: Maximum phonation time of 21 seconds, glottic force closure rate index of 4, reflux index of 2, quality of life index of 5 (Fig. 7).
Figure 7 Patient 4, post-surgery. No evidence of lesions at the supraglotic or glotic level.
Discussion
The larynx is the most common site for primary amyloidosis in the head and neck region. The male-female ratio in our patients was the same as the one reported in medical literature, with a variation in age range.
In order of frequency, lesions were most commonly found in the ventricle, vestibular folds, vocal folds, epiglottis, and aryepiglottic folds. In our patients the most common was the involvement of false vocal cords.
In general, the symptoms of this pathology are specific and do not lead to diagnosis, thus requiring a high level of suspicion, because they will appear depending on the size and site of the lesion. The most common reported symptom in our patients was hoarseness and vocal fatigue.
It is important to rule out the involvement of a systemic disease in patients with this pathology. It is worth noting the fact that in order to obtain our diagnosis, we did not perform any invasive procedures in our patients (i. E. Rectal or bone marrow biopsies).
The treatment for these patients is surgical, and a complete resection is essential to avoid recurrence; however, there are few comparative studies between lesion resection with cold technique and laser to estimate their recurrence. Studies have suggested the use of radiotherapy combined with surgery in those lesions where complete resection is not possible.7
Conclusions
Laryngeal amyloidosis is a rare disease with a rate of 8 in 1,000,000 and a higher incidence during the 5th decade of life. Diagnosis is confirmed by Congo red staining observing an apple-green birefringence under an electronic microscope. Resection with cold technique is an adequate method to remove lesions with positive subjective and objective results. It is important to rule out a systemic involvement in these patients.
Conflicts of interest
The authors have no conflicts of interest to declare.
Funding
No financial support was provided.
Received: November 2013;
Accepted: January 2014
* Corresponding author:
Otolaryngology and Head and Neck Surgery Departament,
“Dr. José Eleuterio González” University Hospital.
Francisco I. Madero and Gonzalitos Avenue,
Mitras Centro, Monterrey, N.L., Mexico.
Telephone: (81) 8333 2917.
E-mail address: vicentevilla@yahoo.com (V. J. Villagómez-Ortiz).