The A-S-C-O classification may be better than other methods for classifying ischaemic stroke by aetiology. Our aims are to describe A-S-C-O phenotype distribution (A: atherosclerosis, S: small vessel disease, C: cardiac source, O: other causes; 1: potential cause, 2: causality uncertain, 3: unlikely to be a direct cause although disease is present) and compare them to the Spanish Society of Neurology's Cerebrovascular Disease Study Group (GEECV/SEN) classification. We will also find the degree of concordance between these classification methods and determine whether using the A-S-C-O classification delivers a smaller percentage of strokes of undetermined cause.
MethodsWe analysed those patients with ischaemic stroke admitted to our stroke unit (SU) in 2010 with strokes that were classified according to GEECV/SEN and A-S-C-O criteria.
ResultsThe study included 496 patients. The percentages of strokes caused by atherosclerosis and small vessel disease according to GEECV/SEN criteria were higher than the percentages for potential atherosclerotic stroke (A1) (14.1% vs. 11.9%; P=.16) and potential small vessel stroke (S1) (14.3% vs. 3%; P<.001). Cardioembolic stroke (C1) was more frequent (22.2% vs. 31%; P<.001). No differences between unusual cause of stroke and other potential causes (O1) were observed. Some degree of atherosclerosis was present in 53.5% of patients (A1, A2, or A3); 65.5% showed markers of small vessel disease (S1, S2, or S3), and 74.9% showed signs of cardioembolism (C1, C2, or C3). Fewer patients in the group without scores of 1 or 2 for any of the A-S-C-O phenotypes were identified as having a stroke of undetermined cause (46.6% vs. 29.2%; P<.001).
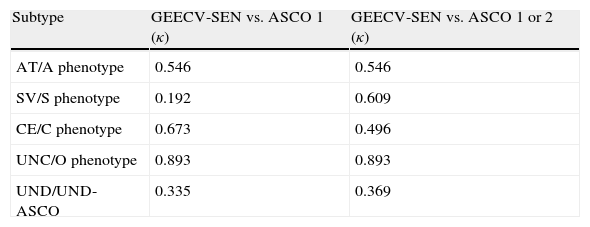
The agreement between the 2 classifications ranged from κ<0.2 (small vessel and S1) to κ>0.8 (unusual causes and O1).
ConclusionOur results show that GEECV/SEN and A-S-C-O classifications are neither fully comparable nor consistent. Using the A-S-C-O classification provided additional information on co-morbidities and delivered a smaller percentage of strokes classified as having an undetermined cause.
La nueva clasificación A-S-C-O puede suponer una mejora en la clasificación etiológica del ictus isquémico. Nuestros objetivos son describir la distribución de los fenotipos A-S-C-O (A: aterotrombótico, S: «small vessel» pequeño vaso, C: cardioembólico, O: otras causas; 1: causa probable, 2: causa posible, 3: enfermedad presente, pero causa improbable), compararlos con la clasificación del Grupo de Estudio de Enfermedades Cerebrovasculares de la Sociedad Española (GEECV/SEN), conocer la concordancia entre ambas clasificaciones y determinar si la clasificación A-S-C-O reduce la proporción de ictus de causa indeterminada.
MétodosAnalizamos los pacientes con ictus isquémicos ingresados en nuestra unidad de ictus durante el 2010, clasificados según las clasificaciones GEECV/SEN y A-S-C-O.
ResultadosIncluímos 496 pacientes. La proporción de ictus aterotrombóticos y por enfermedad de pequeño vaso según criterios GEECV/SEN fue mayor al porcentaje de ictus aterotrombótico probable (A1) (14,1 vs. 11,9%; p=0,16) e ictus por enfermedad de pequeño vaso probable (S1) (14,3 vs. 3%; p<0,001). Los ictus cardioembólicos probables (C1) fueron más frecuentes (22,2 vs. 31%; p<0,001). No observamos diferencias entre los ictus de causa infrecuente y otras causas probables (O1). Un 53,5% presentó algún grado de ateromatosis (A1, A2 o A3), el 65,5% rasgos de pequeño vaso (S1, S2 o S3) y el 74,9% características cardioembólicas (C1, C2 o C3). Una menor proporción de pacientes se clasificaron como de origen indeterminado al considerar aquellos que no obtuvieron puntuación 1 o 2 en ninguno de los fenotipos A-S-C-O (46,6 vs. 29,2%; p<0,001).
La concordancia entre ambas clasificaciones osciló entre κ<0,2 (pequeño vaso y S1) y κ>0,8 (causa infrecuente y O1).
ConclusiónNuestros resultados muestran que las clasificaciones GEECV/SEN y A-S-C-O no son plenamente comparables ni concordantes. La clasificación A-S-C-O aportó información adicional sobre enfermedades coexistentes y permitió reducir la proporción de ictus clasificados como de causa indeterminada.
Ischaemic stroke is an entity with very heterogeneous aetiologies. Researchers have identified multiple causes which combine or act alone to produce cerebral ischaemia.
An ischaemic stroke's aetiology must be identified correctly if doctors are to select the most appropriate preventive treatment and thereby lower the risk of recurrence.
Several different aetiological classification systems for ischaemic stroke are currently in use. Some of the most common include TOAST (Trial of ORG 10172 in Acute Stroke Treatment Subtype Classification),1 the Lausanne Stroke Registry classifications,2 and in Spain, the classification used by the Spanish Society of Neurology's Study Group for Cerebrovascular Diseases (GEECV/SEN in Spanish).3,4 These systems only contemplate the most probable cause of the stroke and ignore other possible coexisting causes.
The recently introduced A-S-C-O (phenotypic) system5 classifies patients with ischaemic stroke according to 4 aetiological phenotypes: atherosclerosis, small vessel, cardiac sources, and other causes. The probability of being the cause of the stroke is determined for each of the phenotypes. This approach provides a more overarching view of the potential causes of stroke in each patient, and also reduces the percentage of strokes classified as being of undetermined origin.
The purposes of this study are to describe the distribution of A-S-C-O phenotypes in a series of ischaemic stroke patients receiving care at our hospital; compare results with those yielded by the GEECV/SEN aetiological classification system; determine the degree of concordance between the systems; and determine if using the A-S-C-O system reduces the percentage of stroke patients placed in the ‘undetermined’ category.
MethodsPatientsWe analysed patients with ischaemic stroke or transient ischaemic attack (TIA) who were hospitalised between 1 January and 31 December 2010 at the stroke unit (SU) pertaining to the neurology department at Hospital General Universitario Gregorio Marañón. Data were entered in a prospective database. Demographic data and risk factors included age, sex, hypertension (HTN), diabetes mellitus (DM), dyslipidaemia (DL), ischaemic heart disease (IHD), atrial fibrillation (AF), and smoking.
Aetiological study of patients with ischaemic strokePatients admitted to the SU were studied in the 24 to 72hours after onset of symptoms. The initial aetiological study, completed for all patients with ischaemic stroke or TIA, included a complete medical history (anamnesis, personal and family history, prior medications), physical examination, and complementary tests. The ‘basic’ complementary study consisted of a blood test (complete blood count); haemostasis; erythrocyte sedimentation rate (ESR); biochemical/glycaemia study; liver profile; kidney function; electrolytes, cholesterol and triglycerides; vitamin B12 and folic acid; glycated haemoglobin; homocysteine; thyroid hormones (TSH and free T4) and high-sensitivity C-reactive protein; and electrocardiogram, chest X-ray, cranial CT, neurosonology study (duplex ultrasonography, transcranial and supra-aortic trunks), and transthoracic echocardiogram.
Neurologists in the SU may opt to expand the aetiological study when the basic study is unable to identify a clear cause of stroke. Complementary tests in the expanded study may include CT-angiography of the supra-aortic trunks and/or circle of Willis, angiography of the supra-aortic trunks or cerebral territories, brain MRI, Holter ECG, transoesophageal echocardiogram, detecting patent foramen ovale using transcranial Doppler ultrasound (the ‘bubble study‘), immunology study (anti-nuclear antibodies, ANCA, anti-DNA antibodies, anti-cardiolipin antibodies and cryoglobulins), serology study (hepatitis B and C, HIV, and syphilis), and checking for coagulation disorders.
Classification system used by the Spanish Society of Neurology's Study Group for Cerebrovascular Diseases (GEECV/SEN).
In daily practice, we use the GEECV/SEN system4 to establish an aetiological diagnosis for patients who have experienced ischaemic stroke or TIA. The GEECV/SEN system only contemplates the most likely cause of the stroke out of the following 5 aetiological categories:
- -
Cardioembolic stroke: caused by emboligenic heart disease such as AF or flutter, mitral stenosis, aortic or mitral valve replacement, intracardiac thrombus, etc.
- -
Atherothrombotic stroke: related to stenosis of more than 50% in a large extracranial or intracranial artery, or stenosis of less than 50% when cardiovascular risk factors are present.
- -
Stroke due to small vessel disease: infarction smaller than 1.5cm in the territory of a perforating artery. The stroke manifests clinically with a typical lacunar syndrome.
- -
Strokes of unusual causes: for example, arterial dissection, vasculitis, prothrombotic states, etc.
- -
Strokes of undetermined causes: the system contemplates 3 subgroups: cause undetermined after a complete study, cause undetermined because the study was incomplete, and cause undetermined due to presence of 2 or more causes.
The A-S-C-O classification system5 groups patients according to 4 aetiological phenotypes: phenotype A (atherosclerosis), phenotype S (small vessel disease), phenotype C (cardiac source), and phenotype O (other causes). Each of these 4 phenotypes is scored from 0 to 3 according to its likelihood of causing the stroke. A score of 1 indicates a potential cause, 2 indicates uncertain causality, 3 indicates that disease is present, but unlikely to be the cause, and 0 indicates that disease is not present. A score of 9 shows that the work-up was insufficient.
Patients included in the study were reclassified retrospectively according to A-S-C-O criteria and based on the results of the aetiological study completed either during the stay in the SU or during subsequent follow-up. Complex and problematic cases were revised by a neurologist specialising in cerebrovascular disease (AGP).
Definitions used in the A-S-C-O classificationWe analysed the distribution of different scores for the 4 A-S-C-O phenotypes and differentiated between the presence of a potential cause (ASCO 1), a potential or uncertain cause (ASCO 1 or 2), and a disease that might or might not be related to the cause of the stroke (ASCO 1, 2, or 3). The study also analysed the prevalence of strokes with a ‘clear’ aetiology, defined as a score of 1 for a single phenotype and scores of 0 on the other 3.
Two models were used to define stroke of undetermined cause according to A-S-C-O criteria.
- -
Model 1, Undetermined stroke-ASCO 1: patients for whom no likely cause of stroke was identified, and who therefore had no scores of 1 on any of the A-S-C-O phenotypes.
- -
Model 2, Undetermined stroke-ASCO 1–2: patients for whom no potential or uncertain causes were found for any of the 4 phenotypes, that is, with no scores of 1 or 2.
We calculated the frequencies of qualitative variables and the means and standard deviations of quantitative variables. Proportions were compared by designing 2×2 contingency tables and using the chi-square and McNemar tests. The Kappa index was calculated to analyse concordance between the 2 aetiological classification systems.6 Values on the Kappa index were interpreted as follows: values below 0.2 reflect poor concordance; those from 0.21 to 0.4 show weak concordance; from 0.41 to 0.6, moderate concordance; 0.61 to 0.8, good concordance; and 0.81 to 1, very good concordance.6 Intergroup differences were understood to be statistically significant for values of P<.05. Statistical analysis of the data was performed using SPSS software, version 15.0, and Epidat (Programa para Análisis Epidemiológico de Datos Tabulados), version 3.1.
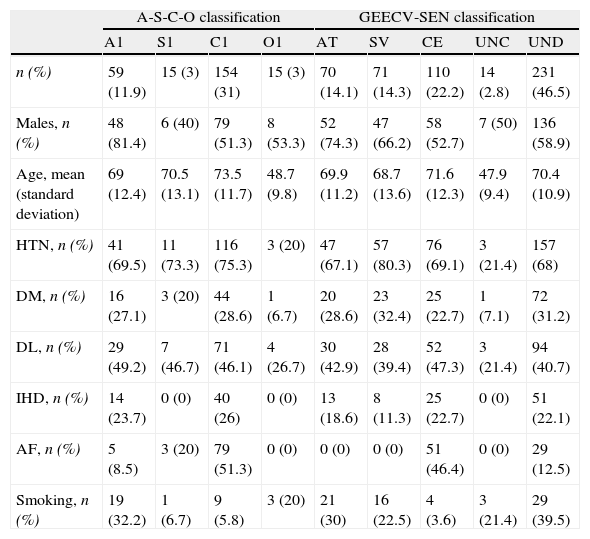
ResultsClinical characteristicsDuring 2010, 549 patients were admitted to the SU. This total included 496 cases (90.3%) of ischaemic stroke or TIA comprising 378 cases of ischaemic stroke (76.2%) and 118 cases of TIA (23.8%). Table 1 displays the demographical characteristics and risk factor distribution for each aetiological subtype of stroke.
Descriptive table showing demographic data and the distribution of risk factors by aetiological subtype for each aetiological classification system.
| A-S-C-O classification | GEECV-SEN classification | ||||||||
| A1 | S1 | C1 | O1 | AT | SV | CE | UNC | UND | |
| n (%) | 59 (11.9) | 15 (3) | 154 (31) | 15 (3) | 70 (14.1) | 71 (14.3) | 110 (22.2) | 14 (2.8) | 231 (46.5) |
| Males, n (%) | 48 (81.4) | 6 (40) | 79 (51.3) | 8 (53.3) | 52 (74.3) | 47 (66.2) | 58 (52.7) | 7 (50) | 136 (58.9) |
| Age, mean (standard deviation) | 69 (12.4) | 70.5 (13.1) | 73.5 (11.7) | 48.7 (9.8) | 69.9 (11.2) | 68.7 (13.6) | 71.6 (12.3) | 47.9 (9.4) | 70.4 (10.9) |
| HTN, n (%) | 41 (69.5) | 11 (73.3) | 116 (75.3) | 3 (20) | 47 (67.1) | 57 (80.3) | 76 (69.1) | 3 (21.4) | 157 (68) |
| DM, n (%) | 16 (27.1) | 3 (20) | 44 (28.6) | 1 (6.7) | 20 (28.6) | 23 (32.4) | 25 (22.7) | 1 (7.1) | 72 (31.2) |
| DL, n (%) | 29 (49.2) | 7 (46.7) | 71 (46.1) | 4 (26.7) | 30 (42.9) | 28 (39.4) | 52 (47.3) | 3 (21.4) | 94 (40.7) |
| IHD, n (%) | 14 (23.7) | 0 (0) | 40 (26) | 0 (0) | 13 (18.6) | 8 (11.3) | 25 (22.7) | 0 (0) | 51 (22.1) |
| AF, n (%) | 5 (8.5) | 3 (20) | 79 (51.3) | 0 (0) | 0 (0) | 0 (0) | 51 (46.4) | 0 (0) | 29 (12.5) |
| Smoking, n (%) | 19 (32.2) | 1 (6.7) | 9 (5.8) | 3 (20) | 21 (30) | 16 (22.5) | 4 (3.6) | 3 (21.4) | 29 (39.5) |
Under GEECV/SEN system: AT: atherothrombotic stroke; CE: cardioembolic stroke; UND: stroke of undetermined cause; UNC: stroke of uncommon cause; SV: stroke due to small-vessel disease.
More than one category may have a score of 1 under the A-S-C-O system.
Aetiological subtypes according to the Spanish Society of Neurology's Study Group for Cerebrovascular Diseases.
Table 1 shows the distribution of different aetiological subtypes of stroke according to GEECV/SEN criteria. Stroke aetiology was established as ‘undetermined’ for 231 patients (46.6%). Eighty cases (16.1%) were considered undetermined due to finding 2 or more coexisting causes; 83 (16.7%) were considered undetermined after a full aetiological study; and 68 cases (13.7%) were undetermined because the work-up was incomplete.
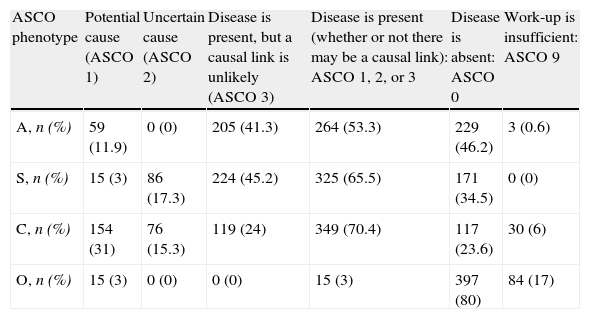
Distribution of A-S-C-O phenotypesTwo hundred twenty-five patients (45.4% of the total) scored 1 on one or more of the 4 A-S-C-O phenotypes. At least one likely or possible cause of stroke was determined for the 351 patients (70.8%) scoring 1 or 2 on at least one A-S-C-O phenotype. Table 2 breaks down A-S-C-O phenotypes by distribution.
Distribution of A-S-C-O phenotypes.
| ASCO phenotype | Potential cause (ASCO 1) | Uncertain cause (ASCO 2) | Disease is present, but a causal link is unlikely (ASCO 3) | Disease is present (whether or not there may be a causal link): ASCO 1, 2, or 3 | Disease is absent: ASCO 0 | Work-up is insufficient: ASCO 9 |
| A, n (%) | 59 (11.9) | 0 (0) | 205 (41.3) | 264 (53.3) | 229 (46.2) | 3 (0.6) |
| S, n (%) | 15 (3) | 86 (17.3) | 224 (45.2) | 325 (65.5) | 171 (34.5) | 0 (0) |
| C, n (%) | 154 (31) | 76 (15.3) | 119 (24) | 349 (70.4) | 117 (23.6) | 30 (6) |
| O, n (%) | 15 (3) | 0 (0) | 0 (0) | 15 (3) | 397 (80) | 84 (17) |
A ‘clear’ stroke aetiology was determined for 57 patients (11.5%). Of the total, 13 cases (2.6%) were considered clearly atherothrombotic (A1-S0-C0-O0); 1 case (0.2%) was identified as clearly small-vessel disease (A0-S1-C0-O0). Another 33 cases (6.7%) were considered clearly cardiac (A0-S0-C1-O0), and 10 cases (2%) were identified as clearly another rare cause (A0-S0-C0-O1).
No causes of stroke could be determined for 6 patients (1.2% of the total), meaning that they scored 0 for all 4 phenotypes (A0-S0-C0-O0). The work-up was insufficient in 98 patients (19.8%), as indicated by scores of 9 on 1 or more phenotypes. Eighteen patients (3.6%) demonstrated 2 or more potential causes (scores of 1 on two or more A-S-C-O phenotypes).
No potential causes of stroke could be determined for 271 patients (54.6%) as reflected by no scores of 1 on any of the A-S-C-O phenotypes. This group was therefore classified as ‘undetermined stroke-ASCO 1’. In 145 cases (29.2%), no potential or uncertain causes could be identified (no scores of 1 or 2 for any of the phenotypes), and they were therefore classified as ‘undetermined stroke-ASCO 1–2’.
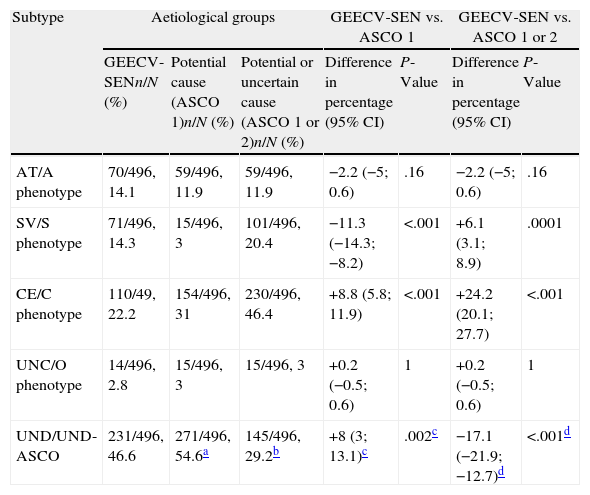
Comparing the A-S-C-O system to the classification devised by the Spanish Society of Neurology's Cerebrovascular Disease Study GroupThe percentage of strokes categorised as atherothrombotic in origin according to GEECV/SEN criteria was slightly higher than the percentage of patients classified as A1 under A-S-C-O (14.1% vs. 11.9%; P=.16). We observed a significantly higher percentage of stroke due to small vessel disease according to GEECV/SEN criteria than of stroke categorised as S1 (14.3% vs. 3%; P<.001). This tendency inverts when we compare the group designated as small-vessel by GEECV/SEN criteria to patients categorised as S1 or S2 (14.3% vs. 20.4%; P<.001). The A-S-C-O system identified more strokes of potentially cardiac origin (C1) than the GEECV/SEN system did (22.2% vs. 31%; P<.001). We observed no differences between groups for strokes of uncommon causes and the O1 group (Table 3).
Differences observed in the distribution of different aetiologies according to the system used.
| Subtype | Aetiological groups | GEECV-SEN vs. ASCO 1 | GEECV-SEN vs. ASCO 1 or 2 | ||||
| GEECV-SENn/N (%) | Potential cause (ASCO 1)n/N (%) | Potential or uncertain cause (ASCO 1 or 2)n/N (%) | Difference in percentage (95% CI) | P-Value | Difference in percentage (95% CI) | P-Value | |
| AT/A phenotype | 70/496, 14.1 | 59/496, 11.9 | 59/496, 11.9 | −2.2 (−5; 0.6) | .16 | −2.2 (−5; 0.6) | .16 |
| SV/S phenotype | 71/496, 14.3 | 15/496, 3 | 101/496, 20.4 | −11.3 (−14.3; −8.2) | <.001 | +6.1 (3.1; 8.9) | .0001 |
| CE/C phenotype | 110/49, 22.2 | 154/496, 31 | 230/496, 46.4 | +8.8 (5.8; 11.9) | <.001 | +24.2 (20.1; 27.7) | <.001 |
| UNC/O phenotype | 14/496, 2.8 | 15/496, 3 | 15/496, 3 | +0.2 (−0.5; 0.6) | 1 | +0.2 (−0.5; 0.6) | 1 |
| UND/UND-ASCO | 231/496, 46.6 | 271/496, 54.6a | 145/496, 29.2b | +8 (3; 13.1)c | .002c | −17.1 (−21.9; −12.7)d | <.001d |
Under the GEECV/SEN system: AT: atherothrombotic stroke; CE: cardioembolic stroke; UND: stroke of undetermined cause; UND-ASCO: stroke of undetermined cause; UNC: stroke of uncommon cause; SV: stroke due to small-vessel disease.
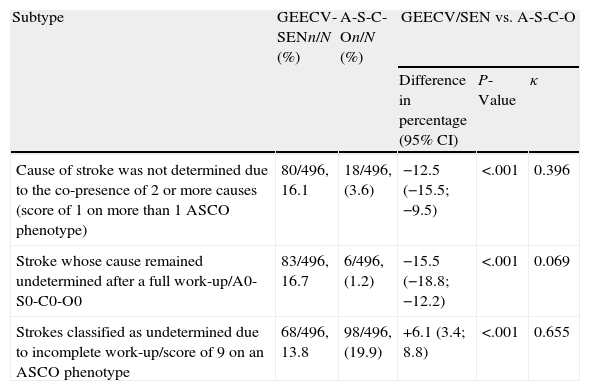
The proportion of ‘undetermined stroke-ASCO 1’ was significantly larger than the percentage of stroke of undetermined cause according to GEECV/SEN criteria (46.6% vs. 54.6%; P<.002). Nevertheless, considering only the undetermined stroke-ASCO 1–2 category, the percentage of strokes of undetermined origin was higher under the GEECV/SEN classification than under ASCO (46.6% vs. 29.2%; P<.001). Table 4 compares the GEECV/SEN's 3 undetermined origin subgroups to the A-S-C-O subgroups.
Differences observed between distributions of different subtypes of stroke of unknown causes according to the GEECV/SEN and A-S-C-O systems. Kappa index (κ) for concordance between the 2 systems.
| Subtype | GEECV-SENn/N (%) | A-S-C-On/N (%) | GEECV/SEN vs. A-S-C-O | ||
| Difference in percentage (95% CI) | P-Value | κ | |||
| Cause of stroke was not determined due to the co-presence of 2 or more causes (score of 1 on more than 1 ASCO phenotype) | 80/496, 16.1 | 18/496, (3.6) | −12.5 (−15.5; −9.5) | <.001 | 0.396 |
| Stroke whose cause remained undetermined after a full work-up/A0-S0-C0-O0 | 83/496, 16.7 | 6/496, (1.2) | −15.5 (−18.8; −12.2) | <.001 | 0.069 |
| Strokes classified as undetermined due to incomplete work-up/score of 9 on an ASCO phenotype | 68/496, 13.8 | 98/496, (19.9) | +6.1 (3.4; 8.8) | <.001 | 0.655 |
Concordance between the 2 systems studied here ranges from poor levels of concordance with κ<0.2 (between small-vessel and S1 categories, for example) and very good levels of concordance with κ-values >0.08, as in the case of strokes of uncommon causes and the O1 category. Kappa values for concordance between the GEECV/SEN and ASCO systems are shown in Table 5.
Kappa index (κ) for concordance between the GEECV/SEN and ASCO systems for classifying different aetiological subtypes of stroke.
| Subtype | GEECV-SEN vs. ASCO 1 (κ) | GEECV-SEN vs. ASCO 1 or 2 (κ) |
| AT/A phenotype | 0.546 | 0.546 |
| SV/S phenotype | 0.192 | 0.609 |
| CE/C phenotype | 0.673 | 0.496 |
| UNC/O phenotype | 0.893 | 0.893 |
| UND/UND-ASCO | 0.335 | 0.369 |
According to GEECV/SEN: AT: atherothrombotic stroke; CE: cardioembolic stroke; UND: stroke of undetermined cause; UNC: stroke of uncommon cause; SV: stroke due to small-vessel disease.
There are 2 main types of aetiological categories: causative and phenotypic.
Causative categories reflect only the most likely cause of the stroke. These are interpretive categories that require integrating multiple aspects of stroke assessment, including symptoms, vascular risk factors, and results from diagnostic tests.7,8 Some of the most frequently-used causal classification systems include TOAST,1 the system developed by the Lausanne Stroke Registry,2 and the GEECV/SEN system.3,4
Phenotypic classifications group patients in more than 1 causal subtype and assign each subtype a degree of likelihood of there being a causal relationship. Examples of such systems include Baltimore–Washington,9 the Causative Classification of Stroke System (CCS),10 and the A-S-C-O classification.5
In this study, we performed a comparative analysis of a causative system (GEECV/SEN) and a phenotypic system (A-S-C-O).
We observed significant differences in how specific aetiological subtypes are distributed depending on which system was employed. One of the most obvious differences is a smaller proportion of the S1 phenotype compared to the percentage of stroke caused by small-vessel disease according to GEECV/SEN criteria. This may be due to the fact that A-S-C-O criteria for a score of 1 (potential cause) in the S phenotype are very strict. In many patients in our study, these criteria could not be applied retrospectively. In contrast, when patients classified as S1 or S2 are considered, the proportion increases and the degree of concordance between the systems also improves (increase in κ-value from 0.192 to 0.609). The same findings have been described in other studies comparing the A-S-C-O and TOAST systems.11,12
The percentage of cardioembolic strokes (classified as C1) was higher than that detected by the GEECV/SEN system, and the difference increased when both C1 and C2 phenotypes were considered. A possible explanation is that some patients with a substantial cardioembolic cause according to the GEECV/SEN system also harboured another potential cause of stroke. These patients would therefore have been placed in the ‘undetermined cause’ group due to the presence of multiple causes. Furthermore, the A-S-C-O system may overestimate strokes of cardiac origin given that patients with a history of AMI or those with bilateral infarcts or infarcts in different vascular territories are classified as C2, indicating uncertain causality. Our results do not support observations from other studies that compared the proportion of strokes that were cardioembolic according to TOAST criteria and the percentage of C1 phenotype in younger patients. Those studies found a lower frequency of cardiac-related stroke when using the A-S-C-O classification.13–15 In contrast, other studies in patients of all ages found no differences in cardioembolic stroke distribution between the 2 classification systems.11,12
Our study did not find significant differences in the percentage of atherothrombotic strokes as determined by either GEECV/SEN or A-S-C-O criteria (11.9% vs. 14.1%). Despite the above, the ASCO system may underestimate the atherosclerotic category given that presence of 50% to 69% stenosis in the absence of thrombus is classified as A3 (disease present, but a causal link is unlikely). In contrast, the GEECV/SEN system may overestimate atherothrombotic causes; in the absence of other causes, patients older than 50 presenting 2 vascular risk factors and atheromatous plaque in the affected vascular territory will be classified as having strokes of atherothrombotic origin.
The main drawback of using causative systems is that they classify a high percentage of strokes as ‘undetermined; between 25% and 39% of all patients will fall into this category.7 This stroke subtype does not exist as such according to the A-S-C-O system. Our study considers 2 approaches to defining stroke of undetermined causes according to the A-S-C-O criteria. The category ‘undetermined stroke-ASCO 1’ yields a higher percentage of strokes of unclear causes than the GEECV/SEN definition (54.6% vs. 46.6%). However, the category ‘undetermined stroke-ASCO 1–2’ contains a much lower percentage of strokes with unclear causes (29.2% vs. 46.6%). Some earlier comparative studies were unable to demonstrate a decrease in the percentage of strokes classified as undetermined under the A-S-C-O system.11,13,15 In contrast, Chatzikonstantinou et al. reported a lower percentage of strokes of undetermined causes (A0-S0-C0-O0) than that yielded by the TOAST system.14 As in our study, Shang and Liu12 demonstrated that a lower percentage of strokes was classified as ‘undetermined’ when patients scoring 1 or 2 on any of the A-S-C-O phenotypes were excluded.
The GEECV/SEN category ‘stroke of undetermined cause’ is very heterogeneous. It includes cases in which multiple causes linked to stroke were identified; strokes in which causes were not established because of an insufficient work-up; and cases in which a complete work-up could not identify a cause of the stroke. (This may be the only group that should truly be regarded as ‘stroke of undetermined cause’.) The A-S-C-O system accounts for all causes potentially contributing to the stroke and makes them visible such that the co-presence of 2 or more causes does not nullify the aetiological diagnosis. Furthermore, this system permits identification of the phenotypes for which the work-up was insufficient. Our model for ‘undetermined stroke-ASCO 1–2’ includes strokes classified as ‘undetermined’ due to the work-up being incomplete (patients with a score of 9 on one or more phenotypes) as well as strokes for which no potential or uncertain causes were determined (scores of 0 or 3 on all 4 phenotypes). As in other studies,12,16 strokes with a ‘clearly’ undetermined cause (A0-S0-C0-O0) were exceptional (a mere 6 cases, 1.2% of the total). This was because there were many cases in which no potential or uncertain causes of stroke were detected, whereas pathological findings unlikely to be direct causes were present (many patients had a score of 3 on one or more of the A-S-C-O phenotypes).
The A-S-C-O classification allows identification of ‘clearly’ attributable cases of stroke, which in our study made up only a small proportion of the total (57 patients or 11.5%). This result confirms the aetiological heterogeneity of stroke and the co-presence of different pathological alterations in the same individual. The A-S-C-O system also lets us identify disease that may not be causally linked to the stroke (scores of 3).11,12
Our study is mainly limited by the fact that the patient reclassification method was retrospective. A potential result of this approach is that the aetiological studies performed on some patients may not have coincided with the requirements of the A-S-C-O system, which would limit the quality of the data.
Using causative systems (especially TOAST, or GEECV/SEN in Spain) is a widespread practice in the sphere of clinical neurology. These easy-to-apply systems simplify the process of making treatment decisions, and are therefore very useful in daily clinical practice. Their main disadvantage is their extreme rigidity, as they admit only one diagnostic category per patient. This results in losses of significant amounts of information on coexisting conditions. Additionally, given that these approaches interpret results from diagnostic tests, the diagnostic process becomes somewhat subjective. Last of all a large patient percentage remains locked into the ‘undetermined cause’ category, which is excessively heterogeneous.
The A-S-C-O classification, in contrast, provides a more global, objective, and flexible diagnosis while also decreasing data loss. It may prove especially useful for selecting patients for clinical trials, as well as for genetic or epidemiological studies. In daily clinical practice, it allows doctors to select more personalised treatments for each case, and enables monitoring of different risk factors and potential causes of new strokes. However, it may prove complex to use – hundreds of different phenotypic combinations are possible – and this can impede the treatment decision-making process.
Results from our study show that GEECV/SEN and A-S-C-O systems are neither fully comparable nor concordant. The A-S-C-O system provides further information about coexisting pathologies and classifies a smaller proportion of strokes as being of undetermined causes.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Sobrino García P, García Pastor A, García Arratibel A, Vicente Peracho G, Rodriguez Cruz PM, Pérez Sánchez JR, et al. Clasificación etiológica del ictus isquémico: comparación entre la nueva clasificación A-S-C-O y la clasificación del Grupo de Estudio de Enfermedades Cerebrovasculares de la Sociedad Española de Neurología. Neurología. 2013;28:417–424.