Motor neuron diseases (MND) do not constitute one of the classically established paraneoplastic neurological syndromes (PNS). Most published examples are of single cases or small series, with a minimal evidence that this is more than chance.1 Herein, we describe the case of a 63-year-old woman with lower motor neuron disease and anti-Hu antibodies who developed a lung neoplasm and autonomic symptoms.
A 63-year-old woman with a history of smoking, thoracic hyperkyphosis and severe pulmonary emphysema is admitted into the intensive care unit due to a respiratory infection requiring intubation and mechanical ventilation. In this context, after presenting a favorable evolution she was assessed by neurologists to complete a 7-month progressive weakness study in both upper extremities that began asymmetrically. In addition, she reported having lost 10kg in the last 6 months. Neurological examination revealed weakness in the neck extensor muscles and a severe weakness of the upper limbs, both proximal and distal, with inability to raise both arms. Atrophy of the shoulder girdle and intrinsic muscles of both hands was observed without visible fasciculations. She also had generalized arreflexia with normal superficial sensitivity and no upper motor neuron signs.
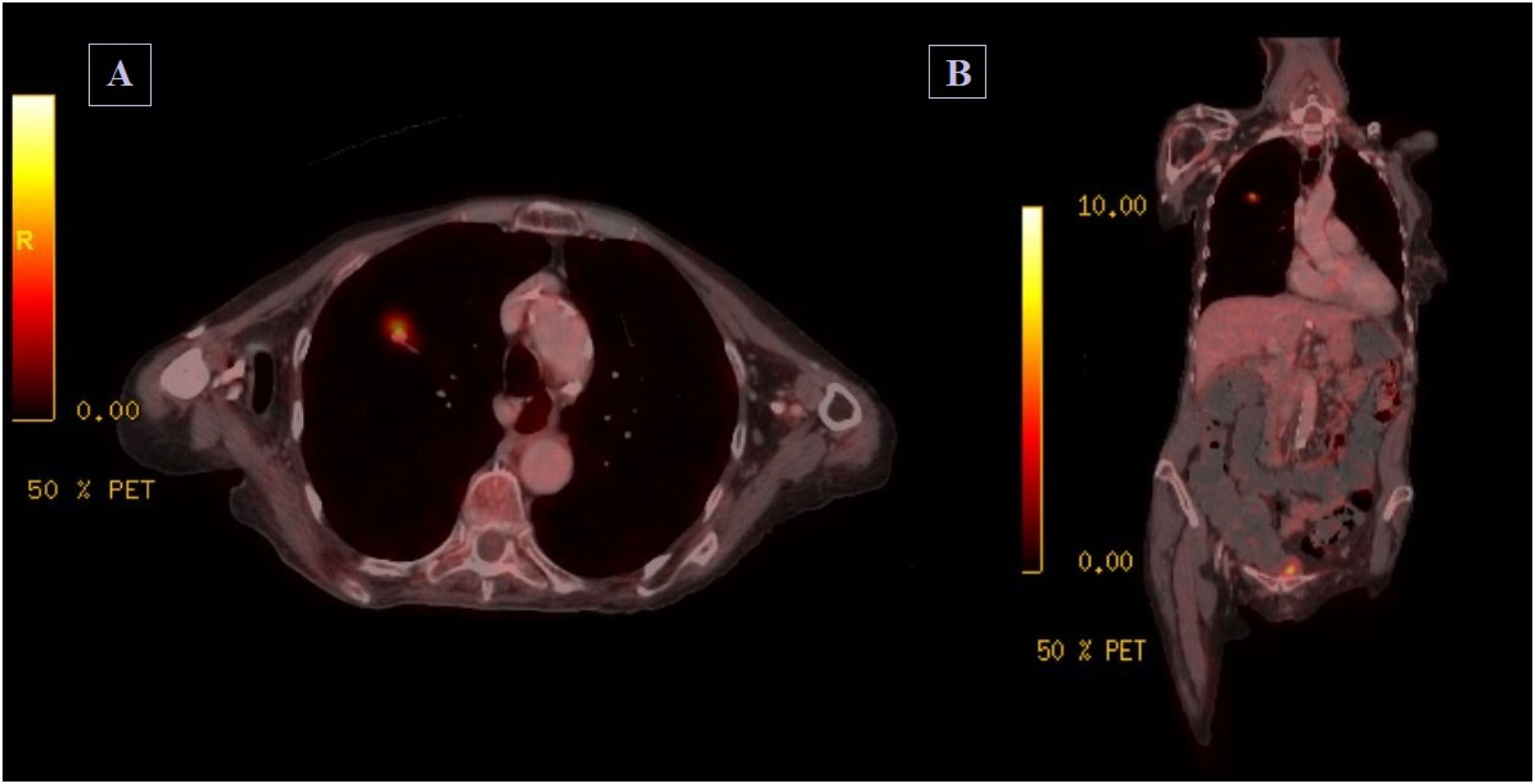
Cervical MRI revealed no significant foraminal or canal stenosis. Blood tests were normal including serologies and serum immunofixation. High titers of ANA and high titers of anti-Hu antibodies were detected (Western Blot technique). The biochemical analysis of the cerebrospinal fluid was normal. Electrodiagnostic findings show extensive neurogenic involvement predominantly in the cervical and thoracic region, with signs of ongoing denervation/reinnervation and massive loss of motor units, without signs of segmental demyelination or sensory neurographic involvement. Whole-body PET-CT scan detected a 10mm diameter hypermetabolic pulmonary nodule in right upper lobe, suggestive of malignancy. See Fig. 1.
A course of intravenous immunoglobulin 0.4g/kg/day was administered for 5 days, with no effect on the neurological condition. The case was presented to a multidisciplinary committee, deciding on radiotherapy treatment given the high surgical risk and the impossibility to perform needle biopsy given the deep location of the lesion and the anatomical characteristics.
After 8 months we observed a progression of the neuromuscular disease, with functionality loss of the upper limbs and development of weakness of the lower limbs, making her unable to stand and walk, with no other signs of the first motor neuron. However, in the control CT scan, the nodule had decreased in size (3mm×4mm). The patient was admitted 4 months later due to a 2-week history of constipation, with a large dilated loop observed on the abdominal CT scan, diagnosing paralytic ileus. During this admission, the patient presented deterioration in her general condition, with bronchial aspiration, so it was decided together with the relatives to limit the therapeutic effort, and she finally died during admission.
Various studies have argued that routinely screening MND cases for anti-neuronal antibodies is of no value.2,3 Nevertheless, few case series have reported well-characterized onconeuronal antibodies in patients with MND, and the pathophysiology of these onconeuronal antibodies is disputed. A recent review by Tolkovsky et al. has analyzed the 17 cases described in the literature about MND and anti-Hu.4 The most common phenotype was women with pattern of “flail arm syndrome” with anti-Hu antibodies and SCLC, as in our case. In most of these patients, lung cancer was diagnosed within a year of the onset of neurological signs.4–7 However, most patients responded little or not at all to immunotherapy and tumor treatment, except in 2 cases that improved after chemoradiotherapy.4,6
In our case, we do not have a pathological diagnosis, but due to the PET characteristics uptake and association with Hu antibodies, the most probable diagnosis was SCLC. Some authors consider that the presence of anti-Hu antibodies in serum could be a marker of SCLC. In this study by List M et al., all patients evaluated with positive anti-Hu antibodies had SCLC.8 On the other hand, Dalmau J et al. evaluated the presence of anti-Hu antibodies in patients with SCLC and healthy subjects. It was found that all those who presented paraneoplastic syndrome had positive anti-Hu and those who did not present paraneoplastic syndrome had positive anti-Hu 7/44 patients. No healthy subject presented anti-Hu antibodies. The anti-Hu antibodies appears, when present, to be a good marker for SCLC.9
In addition, we must consider the autonomic involvement that our patient had, with the development of a paralytic ileus. This could be related to enteric neuropathy in the context of anti-Hu antibodies, although its appearance is not rare as a complication of seriously ill and bedridden patients. Dysautonomia is described in PNS associated with anti-Hu antibodies10 and has also been described only in one case of 32-year-old woman with brachial amyotrophic dyparesis with anti-Hu antibodies,11 with no other cases described in the literature, apart from our case.
Although PMND is considered a non-classical syndrome, the PNS diagnostic criteria proposed by Graus et al.12 allow us to diagnose a “definitive PNS” in the presence of a well-characterized onconeuronal antibody, even in the absence of a classical clinical syndrome.
In conclusion, our case indicated a possible link between antineuronal antibodies and MND, but further investigations are required to evaluate their pathophysiological significance.
EthicsThis article has been reviewed by the Ethical Review board of the Balearic Islands (CEI-IB). The confidentiality of the patient has been preserved (neither text nor images contain identification data nor dates) and the patient's husband has granted his consent for publication. Therefore, this CEI-IB authorizes its publication (IB 4898/22).
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestOn behalf of all authors, the corresponding author states that there is no conflict of interest.