Gamification consists of the use of games in non-playful contexts. It is widely employed in the motor rehabilitation of neurological diseases, but mainly in adult patients. The objective of this review was to describe the use of gamification in the rehabilitation of children and adolescents with neuromotor impairment.
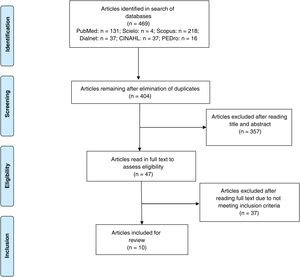
MethodsWe performed a systematic review of clinical trials published to date on the MEDLINE (PubMed), Scielo, SCOPUS, Dialnet, CINAHL, and PEDro databases, following the PRISMA protocol. The methodological quality of the studies identified was assessed using the PEDro scale.
ResultsFrom a total of 469 studies, 11 clinical trials met the inclusion criteria. We analysed the gamification systems used as part of the rehabilitation treatment of different neuromotor conditions in children and adolescents. Cerebral palsy was the most frequently studied condition (6 studies), followed by developmental coordination disorder (3), neurological gait disorders (1), and neurological impairment of balance and coordination (1).
ConclusionThe use of gamification in rehabilitation is helpful in the conventional treatment of neuromotor disorders in children and adolescents, with increased motivation and therapeutic adherence being the benefits with the greatest consensus among authors. While strength, balance, functional status, and coordination also appear to improve, future research should aim to determine an optimal dosage.
La ludificación consiste en emplear el juego en contextos no lúdicos. Su uso en la rehabilitación motora de patologías neurológicas está muy extendido, pero sobre todo en pacientes adultos. El objetivo de esta revisión fue describir el uso de la ludificación en los tratamientos de rehabilitación en niños y adolescentes con afectación neuromotora.
MétodosSe realizó una revisión sistemática de ensayos clínicos en diferentes bases de datos: Medline (a través de Pubmed), Scielo, SCOPUS, Dialnet, Cinahl y PEDro de la literatura científica publicada hasta la fecha siguiendo el protocolo PRISMA. La calidad metodológica de los estudios identificados se evaluó a través de la escala PEDro.
ResultadosDe un total de 469 estudios localizados se seleccionaron 11 ensayos clínicos que cumplieron los criterios de inclusión. Se analizaron los sistemas de ludificación utilizados como parte del tratamiento rehabilitador en distintas afecciones neuromotoras en niños y adolescentes. La Parálisis Cerebral fue la afección con mayor número de estudios (n=6) seguida del Trastorno del Desarrollo de la Coordinación (n=3). También se estudió la alteración de la marcha por causa neurológica (n=1) y la alteración del equilibrio y coordinación por causa neurológica (n=1).
ConclusiónEl uso de la ludificación en rehabilitación aporta beneficios al tratamiento convencional de las alteraciones neuromotoras en niños y adolescentes siendo el incremento de la motivación y adherencia terapéutica los que mayor consenso han alcanzado entre autores. Fuerza, equilibrio, funcionalidad y coordinación son otras variables analizadas que, si bien sugieren mejoras, necesitarían futuras investigaciones para determinar una óptima dosificación.
Neurorehabilitation is a complex healthcare process that aims to restore, minimise, or compensate to the greatest possible extent for functional deficits in individuals with severe disability secondary to central nervous system lesions.1 In recent years, contributions from neuroscience research have led to an important paradigm shift in therapeutic approaches to neurological disease. In paediatric rehabilitation, physiotherapists working as part of interdisciplinary teams are incorporating new approaches into the treatment of motor disorders. This perspective includes task-oriented functional training, practising activities in a context relevant to the child, with a movement towards “hands-off” therapy.2–5 Treatment adherence and motivation are fundamental elements of this new approach, and have played a particularly important role in paediatric treatment since the publication of the International Classification of Functioning, Disability and Health for Children and Youth (ICF-CY),6 which describes in detail the health status of children and adolescents in the first 2 decades of life.
Gamification is defined as the use of game-related elements in a non-play setting.7,8 Such settings could include the workplace, education, or healthcare contexts.9 Most studies on gamification in healthcare are specifically related to the rehabilitation of chronic diseases, physical activity, and mental health.10–12 The majority of neurorehabilitation research addresses adult patients.13–16
In the paediatric field, interactive games should be used in a context in which the therapist observes and treats the child, using the game as a tool to boost motivation and training intensity in a given task. Motivation is needed to modify motor learning programmes.17 van der Kooij et al.18 showed that the inclusion of gamification techniques in the development of a given exercise made the task more pleasant, leading to better results. It should be noted that the therapeutic use of gamification differs from the use of environments enriched with toys, which are understood as complex environments that facilitate cognitive, motor, and sensory stimulation.19,20
In physiotherapy, the use of computer games to attract, motivate, and engage children and adolescents does not guarantee that the desired therapeutic effect will be achieved. However, the characteristics of video games involve dopaminergic reward systems in the brain. This facilitates learning through the generation of synaptic connections.21 The use of games in treatment sessions also triggers cognitive patterns necessary to the treatment and recovery of numerous neurological disorders, assisting in the development of new skills or training in specific activities.22 Treatment adherence, or engagement, and motivation therefore represent essential pillars in the rehabilitation provided by gamification.23 This new approach helps therapists in creating challenging, attractive environments that encourage children and adolescents to practice skills.21,24 Gamification offers clear objectives and new challenges through the use of increasing levels of difficulty, and shows their achievements and provides feedback using a story that offers “rewards.”25
The use of conventional games consoles presents several disadvantages due to the difficulty of adapting the game to the child’s abilities, as games are typically designed for users with normal motor function. Furthermore, the quantification of motor performance is inexact, which may be a hindrance for reliable, systematic follow-up.26 However, said limitations should not prevent the use of these techniques, as several studies suggest that the use of physiotherapy treatments combined with gamification improves treatment success rates.27–29
Identifying and disseminating knowledge on gamification among neurorehabilitation professionals will lead to new treatment opportunities. It will also facilitate the accomplishment of some treatment objectives, taking into account certain important elements alluded to in the ICF-CY, such as participation, activity, or environmental and personal factors. Among physiotherapists, in particular, clinical practice may be optimised by incorporating task-oriented activities, motivation for motor learning, encouraging engagement, etc. This study reports a systematic review of the literature published to date on the use of gamification in physiotherapy treatments in children and adolescents with motor disorders, with an analysis of the methodological quality of the studies identified.
Material and methodsWe conducted a systematic review, following the PRISMA guidelines for the selection of articles.30 The literature search was conducted on the PubMed, Scielo, Scopus, Dialnet, CINAHL, and PEDro databases in July 2020.
The search strategy was adapted to the different databases using the Boolean operators AND and OR. The literature search used the following MeSH terms: “games, experimental” OR “video games” OR “games, recreational” AND “neurological rehabilitation,” “physical therapy modalities,” “child*,” “infant,” “pediatrics,” and “adolescent.” We also added the terms “gamification,” “serious game,” and “game base.”
Inclusion and exclusion criteriaInclusion criteria were: clinical trials using some physiotherapy intervention to treat patients aged 0–18 years with some neuromotor disorder, published in English or Spanish.
Results were not filtered by date of publication, and we only excluded articles that did not report results related to the physiotherapy intervention.
Selection of articlesTwo reviewers (MP and MG) independently searched the different databases, eliminating duplicates and verifying that articles met the selection criteria. Both reviews were submitted to a third reviewer (RR), who resolved any discrepancies. A total of 11 studies were finally included for analysis (Fig. 1).
Assessment of methodological qualityThe PEDro scale was used to determine the methodological quality of the articles selected.31 This scale measures the internal validity and interpretability of results of clinical trials using 11 items, scored 1 or 0 depending on whether each is present in the study. The maximum possible score is 10 points, as the first item is not counted for the final score. Methodological quality is considered high for studies scoring 6 points or more, moderate for scores of 4–5, and low for studies scoring below 4.32
The procedure for the assessment of studies meeting the eligibility criteria mentioned above was the same as that used to select the final results: 2 reviewers (MP and MG) independently evaluated articles, and a third reviewer (RR) resolved any discrepancies.
ResultsThe initial literature search yielded 469 articles; 404 remained after elimination of 65 duplicate results. Subsequently, results were screened by applying the search terms to the titles and abstracts only; 47 remained after screening and were read in full text to apply the eligibility criteria. A total of 10 studies were finally included for qualitative analysis (Fig. 1).
In the qualitative assessment of studies, PEDro scores ranged from 2 points36 to 8 points.33,40 Seven studies scored 6 points or higher, and were therefore considered to be of high quality.33–35,37–39 Only the study by Hammond et al.40 was classed as being of moderate quality (5/10 points). The 2 remaining studies were of low quality, meeting only one36 and 3 criteria,41 respectively.
It should be noted that 2 items were not present in any of the studies analysed: blinding of patients and blinding of therapists. On the other hand, one item was fulfilled by all studies: comparison between groups.
Table 1 presents the structural characteristics of the studies reviewed. The studies reviewed included a total of 344 participants, although sample sizes varied greatly, ranging from 6 participants36 in one study to 62 in another.33 Participants’ ages ranged from 5 years35,37,38 to 17 years.35,39
Main characteristics of the final sample of articles included in the study.
| Authors, year | Sample size (no. girls) | Age | Disorder | Interventions | Sessions | Outcome variables | Time of measurement |
|---|---|---|---|---|---|---|---|
| Arnoni et al.,38 2019 | 15 | 5−13 | CP | IG: conventional therapy+virtual reality (20+20min/session) | 2 sessions/week (8 weeks) | Balance | Pre-/post-intervention |
| IG: 7 (1) | CG: conventional therapy (50min/session stretching and strength exercises) | GMFM | |||||
| CG: 8 (2) | |||||||
| Bonney et al.,39 2017 | 43 | 13−16 | DCD | Nintendo Wii with Wii Balance Board and the Wii Fit game | 1 session/week (14 weeks) | -Isometric muscle strength | Pre-/post-intervention |
| Nintendo Wii: 21 | Task-oriented functional training | -Motor coordination (MABC-2) | |||||
| NTT: 22 | -Self-efficacy in activities of daily living | ||||||
| Chiu et al.,33 2014 | 62 | 6−13 | CP | IG: conventional therapy+training at home with Wii Sport Resort (10min/game; 4 games=40min.) | IG: 3 days/week (6 weeks) | -Coordination (tracking task) | Pre-intervention and at 6/12 weeks |
| IG: 32 (17) | -Strength (dynamometer) | ||||||
| -Hand function (Nine-Hole Peg Test and Jebsen-Taylor Hand Function Test) | |||||||
| -Caregiver perception of hand function (Functional Use Survey) | |||||||
| CG: 30 (17) | CG: conventional therapy | ||||||
| Ferguson et al.,43 2013 | 56 | 6−10 | DCD | Training with Wii Fit, using the Wii Balance Board and 18 games (30min/session) | 3 sessions/week (6 weeks) | -Motor coordination (MABC-2) | Pre-/post-intervention |
| Wii: 19 | Task oriented training (NTT); 45−60min/session | 2 sessions/week (9 weeks) | -Hand strength (FSM) | ||||
| NTT: 37 | -Grip strength (dynamometer) | ||||||
| -Muscle strength (MPST) | |||||||
| -Aerobic capacity (20mSRT) | |||||||
| Gatica-Rojas et al.,34 2017 | 32 | 7−14 | CP | IG: Wii Fit Plus game with Nintendo Balance Board. 2 series of one game and 1 series of Yoga; 30min/session | 3 sessions/week (6 weeks) | -Standing balance (posturography) | Pre-intervention; 2, 4, and 6 weeks. Follow-up at weeks 8 and 10 |
| IG: 16 (6) | CG: conventional physiotherapy; 40min/session | ||||||
| CG: 16 (7) | |||||||
| Hammond et al.,40 2013 | 18 | 7−10 | DCD | IG: training with Wii Fit, using the Wii Balance Board and 9 games (phase 1: 10min/day) | Phase 1: 3 days/week (4 weeks) | -Motor proficiency (short-form BOT-2): fine manual control, coordination, strength, and agility | Pre-intervention, between phases, after phase 2 |
| IG: 10 (2) | CG: conventional therapy (1h/week) | Phase 2 (2.5months after phase 1): 3 days/week (4 weeks) | -Self-perceived ability and satisfaction with motor tasks (CSQ) | ||||
| CG: 8 (2) | -Emotional and behavioural development (SDQ) for parents | ||||||
| Hsieh,37 2018 | 40 | 5−10 | CP | IG: computer game+standing platform (40min/session) | 5 days/week (12 weeks) | -Postural balance (centre-of-pressure sway) | Pre-/post-intervention |
| IG: 20 | -Functional balance (BBS) | ||||||
| CG: 20 | CG: computer game+mouse (40min/session) | -Standing and dynamic balance (FAB) | |||||
| -Functional mobility and dynamic balance (TUG) | |||||||
| Jelsma et al.,41 2014 | 34 | 6−12 | BD | Playing 2 Wii Fit Plus games, selected from 18 options | 3 days/week (6 weeks) | -Motor coordination (MABC-2) | Pre-/post-intervention |
| IG: 14 | -Motor proficiency (BOT-2): fine manual control, coordination, running speed and agility | ||||||
| CG: 20 | -Standing balance (Wii Fit Ski Slalom test) | ||||||
| -Level of enjoyment (Enjoyment Scale) | |||||||
| Kassee et al.,36 2017 | 6 | 7−12 | CP | Wii Sports Resort game (40min/day; 5 days/week) | 5 days/week (6 weeks) | -Upper limb function (MA2; ABILHAND-Kids) | Pre-/post-intervention |
| Wii: 3 | 6 upper-limb resistance exercises (12 repetitions each) | -Grip strength (dynamometer) | |||||
| Resistance: 3 | -Motivation and feasibility (parent-reported questionnaire) | ||||||
| Sajan et al.,35 2016 | 18 | 5−16 | CP | Nintendo Wii game (boxing+tennis) (20min/session) + conventional multidisciplinary therapy (25min/session) | 6 days/week (3 weeks) | -Posture control (static posturography) | Pre-/post-intervention |
| IG: 9 | Conventional multidisciplinary therapy | -Balance (paediatric BBS) | |||||
| CG: 9 | -Manual dexterity (Box and Block Test) | ||||||
| -Quality of upper limb use (QUEST) | |||||||
| -Visual perception (TVPS-3) | |||||||
| -Functional ambulation (walking distance and speed) |
20mSRT: 20-m Shuttle Run Test; BBS: Berg Balance Scale; BD: balance disorder; BOT-2: Bruininks-Oseretsky Test-2; CG: control group; CP: cerebral palsy; CSQ: Coordination Skills Questionnaire; DCD: developmental coordination disorder; FAB: Fullerton Advanced Balance scale; FSM: Functional Strength Measure; GMFM: Gross Motor Function Measure; IG: intervention group; MA2: Melbourne Assessment of Unilateral Upper Limb Function-2; MABC-2: Movement Assessment Battery for Children-2; MPST: Muscle Power Sprint Test; NTT: Neuromotor Task Training; QUEST: Quality of Upper Extremity Skills Test; SDQ: Strengths and Difficulties Questionnaire; TUG: Timed Up and Go; TVPS-3: Test for Visual-Perceptual Skills-3rd edition.
Cerebral palsy (CP) was the neurological disorder addressed in the greatest number of studies analysing gamification (n=6).33–38 Secondly, developmental coordination disorder (DCD) was explicitly addressed in 3 studies.39,40 Only one study analysed gamification in children and adolescents with probable DCD and balance problems.41
All intervention groups completed treatment programmes that included the use of new technologies. The duration of the intervention ranged from 14 sessions39 to 60 sessions.37 Participants completed between one39 and 6 sessions35 per week. Finally, the duration of interventions ranged from 3 to 14 weeks.39Table 1 presents in greater detail the remaining structural characteristics of the reviewed studies.
Table 2 shows the results of all the studies reviewed, classifying measurements into 3 time periods: short term (< 6 weeks), medium term (6−12 weeks), and long term (> 12 weeks). A total of 21 outcome variables were analysed, although not all were measured over all 3 time periods. Specifically, 8 variables were studied over the short term, 11 over the medium term, and 9 over the long term.
Short-, medium-, and long-term results for the outcome variables analysed in the different studies.
| Outcome variable | Study | Measuring instrument | Measurement variable | Group | Pre-intervention | Short term | Medium term | Long term |
|---|---|---|---|---|---|---|---|---|
| (< 6 weeks) | (6−12 weeks) | (> 12 weeks) | ||||||
| Mean (SD) | Mean (SD) | Mean (SD) | ||||||
| Quality of upper limb movement | Kassee et al.,36 2017 | MA2 | Intervention group | 77.94 | – | 87.27 | 82.59 | |
| Control group | 82.02 | – | 85.77 | 84.64 | ||||
| ABILHAND | Intervention group | 1.84 | – | 2.93 | 0.87 | |||
| Control group | 1.50 | – | 1.38 | 0.11 | ||||
| Grip strength | Intervention group | 2.00 | – | 3.08 | 3.42 | |||
| Control group | 2.83 | – | 2.25 | 2.50 | ||||
| Posture control | Sajan et al.,35 2016 | Static posturography | Sway velocity- eyes open (mm/s) | Intervention group | 137.67 | 83.06 | – | – |
| Control group | 137.66 | 127.93 | – | – | ||||
| Sway velocity-eyes closed (mm/s) | Intervention group | 131.29 | 86.92 | – | – | |||
| Control group | 120.33 | 123.93 | – | – | ||||
| Paediatric BBS | Intervention group | 15.70 | 18.7 | – | – | |||
| Control group | 20.44 | 25.00 | – | – | ||||
| Compliance, motivation, and feasibility | Kassee et al.,36 2017 | Compliance and parent feedback questionnaire | Q1 | Intervention group | – | – | 4.00 | – |
| Control group | – | – | 2.00 | – | ||||
| Q2 | Intervention group | – | – | 3.00 | – | |||
| Control group | – | – | .67 | – | ||||
| Q3 | Intervention group | – | – | 2.33 | – | |||
| Control group | – | – | .67 | – | ||||
| Q4 | Intervention group | – | – | 5.00 | – | |||
| Control group | – | – | 4.67 | – | ||||
| Ambulation | Sajan et al.,35 2016 | Walking speed (m/min) | Intervention group | 12.61 | 34.31 | – | – | |
| Control group | 23.89 | 24.61 | – | – | ||||
| Walking endurance (distance in metres) | Intervention group | 131.10 | 317.22 | – | – | |||
| Control group | 151.00 | 218.44 | – | – | ||||
| Gross manual dexterity | Sajan et al.,35 2016 | Box and Block Test | Intervention group | 46.90 | 68.00 | – | – | |
| Control group | 55.2 | 59.33 | – | – | ||||
| Balance | Arnoni et al.,38 2019 | Force plate | Total CoP displacement (cm) | Intervention group | – | –15.93 | – | – |
| Control group | – | –14.53 | – | – | ||||
| AP CoP displacement (cm) | Intervention group | – | 1.45 | – | – | |||
| Control group | – | –2.22 | – | – | ||||
| ML CoP displacement (cm) | Intervention group | – | 2.45 | – | – | |||
| Control group | – | –2.44 | – | – | ||||
| AP amplitude of CoP displacement (cm) | Intervention group | – | –3.66 | – | – | |||
| Control group | – | 2.03 | – | – | ||||
| ML amplitude of CoP displacement (cm) | Intervention group | – | 6.23 | – | – | |||
| Control group | – | –4.85 | – | – | ||||
| Area (cm2) | Intervention group | – | 23.32 | – | – | |||
| Control group | – | 13.29 | – | – | ||||
| Mean velocity (cm/s) | Intervention group | – | 20.22 | – | – | |||
| Control group | – | 46.84 | – | – | ||||
| Gatica-Rojas et al.,34 2017 | AMTI OR6−7 force plate | CoP sway, eyes open (cm2) | Intervention group | 3.75 | 3.58 | 3.06 | 2.19 | |
| Control group | 3.92 | 4.08 | 4.84 | 4.68 | ||||
| CoP sway, eyes closed (cm2) | Intervention group | 4.17 | 4.73 | 4.85 | 4.83 | |||
| Control group | 6.64 | 6.26 | 5.36 | 3.69 | ||||
| SDML, eyes open (cm) | Intervention group | 0.43 | 0.39 | 0.42 | 0.36 | |||
| Control group | 0.46 | 0.42 | 0.46 | 0.44 | ||||
| SDML, eyes closed (cm) | Intervention group | 0.45 | 0.42 | 0.48 | 0.45 | |||
| Control group | 0.51 | 0.53 | 0.50 | 0.43 | ||||
| SDAP, eyes open (cm) | Intervention group | 0.43 | 0.61 | 0.47 | 0.47 | |||
| Control group | 0.48 | 0.55 | 0.60 | 0.64 | ||||
| SDAP, eyes closed (cm) | Intervention group | 0.45 | 0.70 | 0.64 | 0.60 | |||
| Control group | 0.51 | 0.63 | 0.60 | 0.60 | ||||
| ML velocity, eyes open (cm/s) | Intervention group | 0.85 | 1.00 | 0.90 | 0.84 | |||
| Control group | 0.97 | 0.91 | 0.94 | 0.88 | ||||
| ML velocity, eyes closed (cm/s) | Intervention group | 0.92 | 1.15 | 1.07 | 0.96 | |||
| Control group | 1.05 | 1.03 | 0.96 | 0.91 | ||||
| AP velocity, eyes open (cm/s) | Intervention group | 0.94 | 1.00 | 0.95 | 1.00 | |||
| Control group | 1.10 | 0.97 | 1.02 | 1.06 | ||||
| AP velocity, eyes closed (cm/s) | Intervention group | 1.11 | 1.18 | 1.13 | 1.22 | |||
| Control group | 1.32 | 1.14 | 1.05 | 1.15 | ||||
| Balance | Hsieh,37 2018 | CoP kinematics | AP sway (mm) | Intervention group | 9.94 (2.27) | 9.17 (1.69) | – | – |
| Control group | 10.87 (1.41) | 10.55 (1.29) | – | – | ||||
| ML sway (mm) | Intervention group | 6.62 (0.69) | 6.35 (1.00) | – | – | |||
| Control group | 7.13 (1.08) | 6.72 (0.70) | – | – | ||||
| Sway area (cm2) | Intervention group | 14.42 (2.35) | 13.71 (2.24) | – | – | |||
| Control group | 14.33 (2.39) | 13.93 (2.12) | – | – | ||||
| Sway velocity (cm/s) | Intervention group | 4.04 (0.45) | 3.56 (0.47) | – | – | |||
| Control group | 3.69 (0.37) | 3.67 (0.23) | – | – | ||||
| Hsieh,37 2018 | Specific tests | BBS (score) | Intervention group | 44.74 (2.75) | 48.81 (4.74) | – | – | |
| Control group | 44.39 (2.33) | 45.37 (2.68) | – | – | ||||
| FAB (score) | Intervention group | 21.32 (1.47) | 23.41 (2.09) | – | – | |||
| Control group | 22.07 (2.23) | 22.25 (1.90) | – | – | ||||
| TUG (s) | Intervention group | 16.43 (2.12) | 17.51 (1.70) | – | – | |||
| Control group | 15.60 (1.10) | 15.91 (1.87) | – | – | ||||
| Strength | Chiu et al.,33 2014 | PowerTrack IITM | Pressure | Intervention group | 23.5 (21.5) | – | 28.3 (22.3) | 29.7 (23.3) |
| Control group | 26.0 (17.8) | – | 26.9 (23.3) | 29.4 (21.4) | ||||
| Functional strength | Ferguson et al.,43 2013 | FSM | Total FSM | Intervention group | 10.59 (4.50) | – | 6.24 (2.72) | – |
| Control group | 6.87 (3.58) | – | 6.95 (3.95) | – | ||||
| Over-hand throwing | Intervention group | 2.16 (0.73) | – | 2.04 (0.55) | – | |||
| Control group | 1.98 (0.45) | – | 2.09 (0.53) | – | ||||
| Long-jump | Intervention group | 1.09 (0.31) | – | 1.09 (0.18) | – | |||
| Control group | 1.03 (0.25) | – | 1.05 (0.36) | – | ||||
| Under-hand throwing | Intervention group | 2.72 (0.77) | – | 2.80 (0.60) | – | |||
| Control group | 2.50 (0.50) | – | 2.70 (0.60) | – | ||||
| Lateral step up right | Intervention group | 27.85 (6.47) | – | 34.48 (5.49) | – | |||
| Control group | 32.47 (4.97) | – | 33.00 (4.24) | – | ||||
| Lateral step up left | Intervention group | 27.48 (6.47) | – | 35.19 (5.76) | – | |||
| Control group | 33.05 (5.06) | – | 32.42 (4.87) | – | ||||
| Chest pass | Intervention group | 1.69 (0.52) | – | 1.83 (0.38) | – | |||
| Control group | 1.69 (0.25) | – | 1.67 (0.29) | – | ||||
| Sit to stand | Intervention group | 20.30 (5.14) | – | 25.56 (4.66) | – | |||
| Control group | 25.95 (6.72) | – | 26.58 (5.50) | – | ||||
| Lift box | Intervention group | 16.52 (6.56) | – | 22.15 (6.88) | – | |||
| Control group | 18.79 (3.63) | – | 20.89 (4.37) | – | ||||
| Stairs | Intervention group | 61.04 (13.11) | – | 69.46 (11.81) | – | |||
| Control group | 63.84 (9.10) | – | 64.79 (7.56) | – | ||||
| Isometric strength | Ferguson et al.,43 2013 | Hand-held dynamometer | Right elbow flexors | Intervention group | 104.62 (25.06) | – | 109.21 (33.24) | – |
| Control group | 97.48 (20.11) | – | 90.53 (21.13) | – | ||||
| Left elbow flexors | Intervention group | 101.71 (26.91) | – | 105.43 (28.48) | – | |||
| Control group | 92.50 (24.28) | – | 89.69 (19.79) | – | ||||
| Right elbow extensors | Intervention group | 84.47 (21.51) | – | 80.96 (19.44) | – | |||
| Control group | 70.54 (20.59) | – | 76.32 (17.36) | – | ||||
| Left elbow extensors | Intervention group | 86.72 (21.16) | – | 81.41 (21.10) | – | |||
| Control group | 71.77 (20.83) | – | 79.58 (27.94) | – | ||||
| Right knee extensors | Intervention group | 152.25 (51.17) | – | 150.65 (48.75) | – | |||
| Control group | 127.22 (32.72) | – | 139.37 (34.67) | – | ||||
| Left knee extensors | Intervention group | 151.71 (51.46) | – | 145.54 (51.55) | – | |||
| Control group | 120.43 (35.35) | – | 137.57 (31.71) | – | ||||
| Right grip force | Intervention group | 43.33 (12.37) | – | 47.03 (13.32) | – | |||
| Control group | 35.56 (7.57) | – | 49.42 (12.92) | – | ||||
| Left grip force | Intervention group | 37.83 (10.21) | – | 43.58 (12.64) | – | |||
| Control group | 35.03 (8.64) | – | 42.94 (8.83) | |||||
| Muscle strength | Bonney et al.,39 2017 | Knee extensors (N) | Intervention group | 139.5 (27.1) | – | 263.6 (49.2) | ||
| Control group | 157.9 (22.9) | – | 302.3 (68.1) | |||||
| Ankle | Intervention group | 98.9 (17.7) | – | 281.0 (34.5) | ||||
| Control group | 109.4 (20.0) | – | 271.0 (51.3) | |||||
| Ankle plantar flexors (N) | Intervention group | 119.3 (17.8) | – | 213.0 (34.9) | ||||
| Control group | 128.7 (12.9) | – | 229.4 (38.9) | |||||
| Hand function | Chiu et al.,33 2014 | Nine-Hole Peg Test | Intervention group | 0.10 (0.09) | – | 0.10 (0.19) | 0.11 (0.11) | |
| Control group | 0.12 (0.10) | – | 0.13 (0.11) | 0.13 (0.11) | ||||
| Jebsen-Taylor Hand Function Test | Intervention group | 0.21 (0.14) | – | 0.26 (0.18) | 0.31 (0.19) | |||
| Control group | 0.22 (0.15) | – | 0.27 (0.20) | 0.34 (0.21) | ||||
| Upper limb function | Sajan et al.,35 2016 | QUEST | QUEST: grasp domain | Intervention group | 67.82 | 73.35 | – | – |
| Control group | 81.05 | 83.95 | – | – | ||||
| QUEST: dissociated movements domain | Intervention group | 77.94 | 80.40 | – | – | |||
| Control group | 92.61 | 92.96 | – | – | ||||
| QUEST: total score | Intervention group | 72.86 | 76.38 | – | – | |||
| Control group | 86.83 | 88.45 | – | – | ||||
| Generalised self-efficacy | Bonney et al.,39 2017 | CSAPPA total score | Intervention group | 52.7 (10.7) | – | – | 55.6 (11.2) | |
| Control group | 50.0 (12.8) | – | – | 53.9 (9.9) | ||||
| Adequacy score | Intervention group | 19.8 (4.5) | – | – | 19.9 (4.9) | |||
| Control group | 17.6 (5.4) | – | – | 19.6 (5.4) | ||||
| Enjoyment score | Intervention group | 9.8 (2.5) | – | – | 9.5 (2.2) | |||
| Control group | 9.7 (2.5) | – | – | 9.4 (1.6) | ||||
| Predilection score | Intervention group | 23.2 (6.5) | – | – | 26.1 (5.9) | |||
| Control group | 22.8 (7.3) | – | – | 24.9 (4.3) | ||||
| GMFM | Arnoni et al.,38 2019 | GMFM | Standing | Intervention group | – | –2.310 | – | – |
| Control group | – | NA | – | – | ||||
| Walking, running, and jumping | Intervention group | – | –2.672 | – | – | |||
| Control group | – | NA | – | – | ||||
| Visual-perceptual skills | Sajan et al.,35 2016 | TVPS-3 | TVPS (total score) | Intervention group | 32.10 | 43.44 | – | – |
| Control group | 36.50 | 37.30 | – | – | ||||
| MABC-2 (motor proficiency) | Bonney et al.,39 2017 | Total standard score | Intervention group | 61.4 (10.4) | – | – | 74.0 (10.3) | |
| Control group | 63.0 (5.6) | – | – | 78.1 (8.8) | ||||
| Manual dexterity | Intervention group | 5.5 (2.1) | – | – | 8.9 (2.7) | |||
| Control group | 5.9 (1.5) | – | – | 9.7 (1.5) | ||||
| Aiming and catching | Intervention group | 9.0 (2.3) | – | – | 8.9 (2.5) | |||
| Control group | 9.3 (2.6) | – | – | 10.1 (2.9) | ||||
| Balance | Intervention group | 7.0 (2.9) | – | – | 8.9 (2.6) | |||
| Control group | 6.9 (2.1) | – | – | 9.1 (2.5) | ||||
| Ferguson et al.,43 2013 | Total standard score | Intervention group | 4.26 (1.02) | – | 8.67 (2.51) | – | ||
| Control group | 5.32 (1.45) | – | 6.05 (2.83) | – | ||||
| Manual dexterity | Intervention group | 6.04 (2.23) | – | 9.04 (2.56) | – | |||
| Control group | 6.05 (2.42) | – | 6.16 (3.02) | – | ||||
| Aiming and catching | Intervention group | 7.56 (2.72) | – | 8.52 (2.44) | – | |||
| Control group | 6.53 (3.27) | – | 6.84 (3.18) | – | ||||
| Balance | Intervention group | 4.26 (2.44) | – | 9.48 (2.31) | – | |||
| Control group | 7.00 (2.31) | – | 8.11 (2.47) | – | ||||
| Caregiver perception | Chiu et al.,33 2014 | Functional Use Survey | Quantity (0−65) | Intervention group | 28.1 (17.9) | – | 32.7 (15.9) | 35.6 (15.8) |
| Control group | 34.0 (16.9) | – | 32.6 (13.4) | 33.8 (15.5) | ||||
| Quality (0−65) | Intervention group | 30.1 (17.6) | – | 34.0 (16.7) | 34.8 (13.4) | |||
| Control group | 34.7 (14.9) | – | 34.5 (14.9) | 35.3 (14.5) | ||||
| Aerobic and anaerobic performance | Ferguson et al.,43 2013 | MPST | Intervention group | 104.92 (45.91) | – | 139.70 (63.63) | – | |
| Control group | 115.88 (36.91) | – | 136.54 (41.64) | – | ||||
| 20mSRT | Intervention group | 1.28 (0.40) | – | 1.74 (1.05) | – | |||
| Control group | 1.63 (0.86) | – | 1.61 (0.92) | – | ||||
| Functional performance | Bonney et al.,39 2017 | BOT-2 Running and agility (SS) | Intervention group | 14.1 (3.9) | – | – | 18.5 (3.2) | |
| Control group | 14.4 (2.9) | – | – | 18.3 (1.6) | ||||
| 10×5m straight sprint (s) | Intervention group | 24.8 (3.9) | – | – | 22.2 (3.0) | |||
| Control group | 25.0 (3.5) | – | – | 21.7 (2.1) | ||||
| 10×5m slalom sprint (s) | Intervention group | 24.3 (4.1) | – | – | 22.2 (3.1) | |||
| Control group | 24.6 (3.8) | – | – | 20.6 (2.0) | ||||
| Stair climbing | Intervention group | 67.5 (14.9) | – | – | 74.8 (10.4) | |||
| Control group | 72.0 (7.3) | – | – | 78.0 (7.9) | ||||
| Motor proficiency | Hammond et al.,40 2013 | BOT-2 | Fine motor precision | Intervention group | 9.2 (1.95) | 10.3 (2.39) | 10.2 (2.92) | – |
| Control group | 10.4 (3.26) | 10.0 (2.51) | 12.25 (2.38) | – | ||||
| Fine motor integration | Intervention group | 7.5 (2.17) | 8.9 (2.45) | 7.6 (2.06) | – | |||
| Control group | 9.0 (0.82) | 8.25 (1.83) | 9.25 (1.16) | – | ||||
| Manual dexterity | Intervention group | 4.3 (1.23) | 5.3 (1.04) | 5.3 (1.39) | – | |||
| Control group | 4.14 (1.07) | 4.5 (1.31) | 5.5 (0.76) | – | ||||
| Bilateral coordination | Intervention group | 4.6 (1.83) | 6.4 (0.91) | 5.8 (1.46) | – | |||
| Control group | 6.29 (0.76) | 5.5 (0.93) | 7.38 (1.06) | – | ||||
| Balance | Intervention group | 5.9 (2.84) | 7.8 (2.91) | 7.5 (3.28) | – | |||
| Control group | 7.57 (0.79) | 6.88 (1.46) | 8 (0) | – | ||||
| Running speed and agility | Intervention group | 1.2 (4.12) | 2.3 (3.86) | 1.3 (3.88) | – | |||
| Control group | 1.57 (0.53) | 1.5 (0.53) | 1.75 (0.46) | – | ||||
| Upper limb coordination | Intervention group | 7.8 (2.99) | 8.9 (2.43) | 8.2 (2.27) | – | |||
| Control group | 6.71 (1.5) | 9.13 (1.89) | 10 (2) | – | ||||
| Strength | Intervention group | 5.7 (2.31) | 6.8 (1.93) | 7.2 (2.35) | – | |||
| Control group | 5.29 (1.5) | 7.63 (4.31) | 8.88 (3.09) | – | ||||
| Aerobic endurance | Bonney et al.,39 2017 | Shuttle run (level) | Intervention group | 2.3 (1.5) | – | – | 2.4 (1.6) | |
| Control group | 1.9 (0.9) | – | – | 2.3 (1.1) |
20mSRT: 20-m Shuttle Run Test; AP: anterior-posterior; BBS: Berg Balance Scale; BOT-2: Bruininks-Oseretsky Test-2; CoP: centre of pressure; CSAPPA: Children’s Self-Perceptions of Adequacy in and Predilection for Physical Activity scale; FAB: Fullerton Advanced Balance scale; FSM: Functional Strength Measure; GMFM: Gross Motor Function Measure; MA2: Melbourne Assessment of Unilateral Upper Limb Function-2; MABC-2: Movement Assessment Battery for Children-2; ML: medial-lateral; MPST: Muscle Power Sprint Test;NA: not available; QUEST: Quality of Upper Extremity Skills Test; SDAP: standard deviation of AP centre of pressure; SDML: standard deviation of ML centre of pressure; SS: scale scores; TUG: Timed Up and Go; TVPS-3: Test for Visual-Perceptual Skills-3rd edition.
Variables can be classified into 3 different categories: quantitatively analysed functional capacities (9 variables); qualitatively analysed functional capacities (9); and subjective assessment using questionnaires (4). Some variables (e.g., motor performance) were analysed with more than one instrument, and therefore may appear in more than one of these categories. Table 2 presents detailed information on the results for each variable.
Ferguson et al.43 compared the effects of 2 task-oriented intervention strategies in children aged 6−10 years with DCD. One strategy used the Nintendo Wii console. The variables measured included motor performance, aerobic/anaerobic capacity, and muscle strength. Both groups presented significant improvements, with anaerobic capacity being the only one for which gamification was associated with statistically significant differences compared to neuromotor task training based on cognitive neuroscience and motor learning theories. Outcome variables were measured with the most recent version of the Movement Assessment Battery for Children-2 (MABC-2), the 20-m Shuttle Run Test, the Muscle Power Sprint Test, and hand-held dynamometer measurement of grip strength.
Hammond et al.40 used the Nintendo Wii Fit game, on the Nintendo Wii console, to compare efficacy against the conventional therapy. They selected 9 balance- and coordination-based games, which members of the intervention group played for 10minutes, 3 times weekly. In the second phase, both groups switched interventions for 4 weeks. The outcome variables studied were motor skills, self-perceived ability and satisfaction with the motor task, and emotional and behavioural development. Regarding motor skills, both groups presented improvements in the short-form Bruininks-Oseretsky Test (BOT-2), a measure of manual dexterity. However, the change was only statistically significant in the intervention group. Similarly, both groups showed improvements in self-perceived ability and satisfaction with the motor task at the end of phase 1, and the improvement persisted after phase 2; however, these results were not statistically significant. These variables were measured with the Coordination Skills Questionnaire. Emotional and behavioural development was analysed with the parent-reported Strengths and Difficulties Questionnaire; only 7 families (for a total of 18 participating patients) responded, with the intervention group showing a quantifiable improvement.
Chiu et al.33 used the Nintendo Wii console with the Wii Sports Resort game in a sample of 62 children with hemiplegic CP, comparing this intervention against conventional physiotherapy in the paretic upper limb. The authors analysed coordination and hand strength and function, as well as caregivers’ perception of hand function. These variables were measured before the intervention, at the end of the intervention, and at 6 weeks post-intervention. The games used (bowling, air sports, Frisbee, and basketball) were selected because of the ability to select progressive difficulty levels. Improvements were observed in the intervention group, but were not statistically significant; therefore, the study does not demonstrate that the use of video games offers advantages over conventional therapy in such variables as coordination, strength, or hand function (measured with the Nine-Hole Peg Test, Jebsen-Taylor Hand Function Test, and dynamometry measurement) in children with hemiplegia. However, perceived hand function, measured with the parent-reported Functional Use Survey, did show improvements in the intervention group.
Jelsma et al.41 studied the effect on balance of training with the Nintendo Wii, with the Wii Fit Plus game and the Wii Balance Board. The sample was made up of children with balance problems and typically developing children. Although the study used the MABC-2 to assess balance, the authors did not assert that children scoring below percentile 16 presented DCD. All participants used these platforms for sessions of 30minutes, 3 times weekly. During that time, they could choose from 18 games available in Wii Fit Plus, with the exception of the Ski Slalom game, which was used for assessment. Participants had to play each game twice before they could choose a different one. Before and after the intervention, participants were assessed to test motor ability (MABC-2), motor proficiency (BOT-2), standing balance (Wii Fit Ski Slalom), and enjoyment (Enjoyment Scale). Analysis of the results showed that the typically developing children scored better for the balance test. Children with balance problems also showed a significant improvement after the intervention, with positive results persisting after the non-intervention period. All children enjoyed the intervention, and continued to show motivation at 6 weeks post-intervention.
Gatica-Rojas et al.34 analysed standing balance in children with CP, comparing the results after a conventional physiotherapy intervention (stretching, strengthening, flexibility, and balance) against use of Wii Fit Plus with the Nintendo Wii Balance Board. Participants completed 2 sets on the Snowboard, Penguin Slide, and Super Hula Hoop games. The intervention group showed statistically significant improvements in all variables, with the effect persisting 6 weeks after completion of the intervention. However, the improvement in centre-of-pressure sway did not persist in the long term. Outcome variables were measured using posturography.
The study by Sajan et al.35 measured posture control, manual dexterity, upper limb function, and ambulation in children and adolescents with CP. Both the control group and the intervention group, who completed a game-based intervention with the Nintendo Wii system, showed similar results in the different study variables. Only manual dexterity as measured with the Quality of Upper Extremity Skills Test showed significant improvements in the intervention group after treatment. The variables postural control, balance, unilateral gross manual dexterity, visual-perceptual skills, and functional ambulation (studied with static posturography, the Berg Balance Scale, the Box and Block Test, the Test for Visual-Perceptual Skills, and walking speed and distance, respectively) showed no significant difference after adding conventional physiotherapy to the intervention.
Bonney et al.39 compared the efficacy of Nintendo Wii training against task-oriented functional training in 43 girls aged 13−16 years with DCD. They measured strength in the knee flexors, ankle plantar flexors, and dorsiflexors, coordination, and self-efficacy, among other variables. No differences between the 2 interventions were observed in the different outcome measures used, including the MABC-2, BOT-2, and Participation in Activities of Daily Living for Adolescents Questionnaire.
Kassee et al.36 compared upper limb functional ability and strength and treatment adherence in 6 children with CP. The intervention consisted in Nintendo Wii training, and was compared against resistance training with a series of 6 exercises to be performed each week. Both interventions were followed at home. This study found significant differences between groups, with greater improvements in the intervention group for all variables except grip strength, for which dynamometry showed better results in the conventional training group. Motivation and feasibility of home training were studied with a questionnaire completed by participants’ parents.
In a sample of 40 children with CP, Hsieh37 studied 2 interventions to treat balance alterations, measuring centre-of-pressure sway, the Berg Balance Scale, the Fullerton Advanced Balance Scale, and the Timed Up and Go test. Results were compared between the intervention group, who used a platform through which children used their whole body to play computer games, and the control group, who played the same games with a computer mouse rather than the standing platform. The author concluded that the platform could be used to improve balance in children with CP.
Finally, Arnoni et al.38 compared the effect on balance and gross motor function of conventional therapy and a virtual reality game in 15 children and adolescents with CP. Outcome variables were measured with a force platform and with the Gross Motor Function Measure tool. The intervention group showed statistically significant improvements in gross motor function but not in standing stability.
DiscussionThe aim of this study was to review the scientific literature on the use of gamification in the neurorehabilitation of children. After gathering and critically analysing clinical trials of children with motor disorders, we observed that gamification is a treatment strategy that should be considered. Short-, medium-, and long-term improvements were observed in motivation, balance, strength, function, coordination, and family satisfaction, among other variables, when gamification was incorporated into the treatment of children and adolescents with neuromotor disorders. Our conclusions are supported by the high methodological quality of the majority of the studies analysed.
Game mechanics are essential, and lead to engagement and motivation in a field that was not originally related to the game, such as neurorehabilitation. However, several studies included motivation as an outcome variable.36,40–42 This is highly relevant, as treatment adherence is often a challenge in the treatment of children and adolescents.
A systematic review by Sardi et al.,10 addressing the use of gamification in healthcare contexts, analysed 46 articles mainly including patients with chronic diseases and mental illness. Video games have been incorporated into the neurorehabilitation treatment of adults by authors including Yates et al.,13 Psychouli et al.,14 Tsekleves et al.,15 and Trombetta et al.16
It is essential to consider both personal and environmental factors in the development of treatments, in accordance with the recommendations of the ICF-CY.6 Thus, some researchers apply interventions in the environments in which children and adolescents naturally develop, such as the home33,36 or at school.40 Thus, promotion and monitoring of community participation39 and involvement of parents in treatment33,36,40 are approaches that follow these recently developed principles, which are not always present in intervention proposals.
The use of conventional games consoles presents several challenges, such as the difficulty of adapting the game to the child’s abilities, as games are usually designed for users without motor alterations. Furthermore, the quantification of motor performance is inexact, which may constitute a hindrance to reliable, systematic follow-up.26 However, authors including Ferguson et al.,43 Hammond et al.,40 Chiu et al.,33 Jelsma et al.,41 Gatica-Rojas et al.,34 Sajan et al.,35 Bonney et al.,39 and Kassee et al.36 did not hesitate to use commercially available games and platforms; other authors designed video games for specific purposes.42 Nonetheless, these limitations should not prevent the use of these games, as several studies suggest that the use of physiotherapy treatments combined with gamification improves treatment success rates.27–29
Short-term effectsThe short-term results of interventions in patients with CP show improvements in the vast majority of the variables analysed. Thus, intervention groups participating in rehabilitation programmes including gamification strategies showed short-term improvements in such areas as posture control,35 ambulation,35 gross manual dexterity,35 and visual perceptual skills,35 compared to controls. However, variables including upper limb function35 and balance34,37 showed similar values after the intervention, although patients with CP did show short-term improvements compared to controls in one balance parameter (centre-of-pressure sway, open-eyes).34
Patients with DCD displayed significant short-term improvements in motor performance.40 The results reported support the need to develop specific treatment protocols for the outcome variable of interest, as very good short-term benefits have been observed in patients participating in 3 or 6 sessions per week,35,40 whereas patients undergoing programmes with 3 or 5 sessions per week showed similar outcomes to controls.34,37
Medium-term effectsAs was the case with short-term effects, the majority of variables analysed in patients with CP showed greater medium-term benefits in intervention groups than in controls (Table 2). Specifically, intervention programmes including gamification showed greater compliance, motivation, and feasibility,36 with participating patients showing better upper limb quality of movement36 and balance (with eyes open),34 and grip strength,33 compared to controls. Furthermore, analysis of a measure as subjective as caregiver perception revealed an increase of over 10% compared to baseline, in both qualitative and quantitative assessments.33
However, results for hand function presented a similar trend to that observed in the control group.33
One important consideration is the fact that the study by Gatica-Rojas et al.34 was the only one to include assessment and follow-up in the medium term. In that study, the short-term benefits observed persisted in the medium term. In this sense, balance (eyes open) improved significantly more in the intervention group than in the control group. However, this trend was not observed in the other variables analysed, with both groups showing comparable results.
In patients with DCD, 4 outcome variables were analysed in the medium term. Specifically, neither isometric strength43 nor motor performance40 showed significant differences between the intervention and the control groups. However, functional strength43 and motor proficiency43 did show significant differences between groups, with better results in the conventional physiotherapy group. Specifically, motor proficiency43 showed an increase in total test score, particularly conditioned by scores for 2 components (manual dexterity and balance).
Long-term effectsEight outcome variables were analysed in the long term, in 2 studies (assessing 4 variables) that included patients with CP33,35 and one (4 variables) that included individuals with DCD.39 Specifically, patients with CP showed poorer upper limb quality of movement in 2 of the variables analysed, whereas a third (grip strength) improved with respect to baseline.35 This long-term improvement is consistent with that observed by Chiu et al.,33 who also observed significant differences compared to baseline, although the magnitude of the effect was not significantly larger than that observed in the control group.33 This similarity in the progression of outcome variables in the intervention and the control groups was also observed for hand function. Caregiver perception not only showed persistence of the improvement observed in the medium term, but even a slight increase.33
Another 4 variables were analysed in a study of patients with DCD.39 Three of these (muscle force, self-efficacy, and functional performance) behaved similarly in both the intervention and the control groups. Furthermore, analysis of running performance after the intervention showed better results in the control group than in the intervention group in the long term.39
This review is not free of potential limitations due to the databases selected, filtering for language of publication, and the inclusion criteria applied in the literature search. The heterogeneity of the studies reviewed in terms of methodology and the outcome measures studied prevented us from conducting a meta-analysis.
In this sense, raising awareness of gamification among neurorehabilitation professionals in general, and physiotherapists in particular, will lead to new therapeutic opportunities. Thus, realistic use of gamification in physiotherapy may enable optimisation of clinical practice, and represents a promising approach.21
Future studies should use larger patient samples in order to obtain more robust results. It would also be interesting to establish the most beneficial dose of neurorehabilitation treatments incorporating gamification.
In conclusion, the literature consulted on gamification in paediatric neurology supports its use in clinical practice, either in isolation or as a supplement to conventional therapy; these techniques are safe to use in natural environments such as the home or school settings, and offer motivation for children and adolescents with neuromotor impairment.
FundingThis study has received no specific funding from any public, commercial, or non-profit organisation.
Conflicts of interestThe authors have no conflicts of interest to declare.