Cerebrovascular disease is associated with high morbidity and mortality. In 2008, the Spanish Ministry of Health published its Clinical Practice Guidelines for stroke prevention, but implementation of that document has not yet been assessed. Our study aims to investigate compliance with the Guidelines by analysing control over vascular risk factors, antithrombotic treatment and lipid lowering treatment in patients who had suffered an acute ischaemic stroke and who were under the care of neurologists or internists.
MethodsCross-sectional study based on data from clinical reports (vascular risk factors, diagnosis and treatment), blood pressure readings and laboratory tests pertaining to 203 patients diagnosed with acute ischaemic stroke and admitted to a medium-to-long stay hospital for rehabilitation and care.
ResultsThe mean patient age was 75±10 years; 56% were women. The most common risk factors were hypertension (68%) and diabetes mellitus (40%). Intravenous fibrinolytic therapy had been administered to 8.9% of the patients. Of the patients with thrombotic cerebral infarction, 91.7% received antiplatelet agents; 59.4% of patients with embolic infarction received anticoagulants. Statins were prescribed to 65% of patients with thrombotic infarction. Laboratory tests upon admission showed that 23% of patients had total cholesterol levels above 175mg/dl and 26.6% had plasma glucose levels above 126mg/dl. Of the patient total, 70% received antihypertensive therapy, but 47.5% had blood pressure levels above 130/80mm Hg.
ConclusionsIn our opinion, secondary prevention of acute cerebrovascular disease could be improved, mainly by increasing the percentage of patients treated with antiplatelet or anticoagulant drugs (depending on aetiology), increasing prescription of statins, and improving blood pressure control.
La enfermedad cerebrovascular se asocia a una elevada morbimortalidad. En el año 2008, el Ministerio de Sanidad publicó la «Guía de práctica clínica» sobre prevención del ictus sin que se haya evaluado su implementación. Nos planteamos investigar el seguimiento de dicha guía a través del análisis del control de factores de riesgo vascular y el tratamiento antitrombótico e hipolipemiante en pacientes con ictus isquémico agudo atendidos por neurólogos o internistas.
MétodosEstudio transversal descriptivo basado en los datos obtenidos de informes clínicos (factores de riesgo vascular, diagnóstico y tratamientos), cifras tensionales y analíticas de 203 pacientes con diagnóstico principal de ictus isquémico agudo que ingresaron para rehabilitación y cuidados en un hospital de media-larga estancia.
ResultadosLa edad media±DE de los pacientes incluidos fue de 75±10 años con un 56% de mujeres. Los factores de riesgo más frecuentes fueron hipertensión arterial (68%) y diabetes mellitus (40%). El 8,9% de los pacientes había recibido fibrinólisis por vía intravenosa. El 91,7% de los pacientes con ictus aterotrombótico recibía antiagregantes; el 59,4% de los pacientes con ictus cardioembólico estaba anticoagulado. Se prescribieron estatinas al 65% de los pacientes con ictus aterotrombótico. En la analítica de ingreso, el 23% de los pacientes presentaba una colesterolemia total mayor de 175mg/dl y el 26,6% una glucemia plasmática mayor de 126mg/dl. El 70% de los pacientes tenía tratamiento antihipertensivo, aunque el 47,5% presentaba cifras tensionales mayores de 130/80mmHg.
ConclusionesCreemos que aún es posible mejorar la prevención secundaria en enfermedad cerebrovascular, principalmente aumentando el porcentaje de pacientes tratados con antiagregantes o anticoagulantes según la etiología, la prescripción de estatinas y mejorando el control tensional.
Atherothrombotic vascular diseases manifest clinically as ischaemic heart disease, cerebrovascular disease, or peripheral artery disease. They are the most frequent causes of both mortality and morbidity in Spain. According to that country's National Institute of Statistics, cardiovascular disease was the most common cause of death in Spain in 2007 (the second-most common in men and the most common in women). There were 124126 deaths due to cardiovascular disease compared to 103329 due to neoplasia during that year.1
Few studies in our country have examined adherence to secondary prevention measures for cerebrovascular disease,2–4 while other topics in atherothrombosis, such as ischaemic heart disease, have received more attention. Regarding secondary prevention for cardiovascular disease, the literature2 reports that only 43% of patients have well-controlled blood pressure, while 51.8% have cholesterol levels within the recommended range and 70% have good blood sugar levels. Studies of treatment prescribed to patients with acute ischaemic stroke2,3 reveal that 77% to 83% of these patients are treated with antiplatelet drugs while 17% to 18% are on anticoagulants; statin drugs are prescribed to 11% to 52%.2,4
In 2008, the Ministry of Health published clinical practice guidelines (CPG) for primary and secondary stroke prevention.5 For patients who are stable after having suffered ischaemic stroke or transient ischaemic attack (TIA), the guidelines recommend gradually decreasing blood pressure to reach a target of 130/80mm Hg (grade B recommendation). Ideally, this is achieved through treatment with an angiotensin converting enzyme (ACE) inhibitor associated with a diuretic drug (grade A recommendation). Depending on the patient's tolerance and concomitant illnesses, another approach may be monotherapy (grade B recommendation) with diuretics, ace inhibitors, or angiotensin II receptor blockers (ARBs). The guidelines also recommend prescribing atorvastatin at a dose of 80mg/day (grade A recommendation) or simvastatin at a dose of 40mg/day (grade B recommendation) in patients with ischaemic stroke or TIA due to an atherothrombotic cause, regardless of baseline LDL cholesterol readings. In patients with atrial fibrillation who have a prior history of stroke and no formal contraindications for treatment, the CPG5 recommends indefinite treatment with oral anticoagulation drugs with an INR of between 2 and 3 (grade A recommendation). For patients with ischaemic stroke or non-cardioembolic TIA, the guidelines indicate antiplatelet treatment with aspirin, triflusal, clopidogrel, or a combination of aspirin and slow-release dipyridamole (grade A recommendation).
The Spanish Society of Neurology's study group for cerebrovascular diseases recently published guidelines for preventative treatment of ischaemic stroke and TIA.6 This document coincides with the 2008 CPG5 in recommending the following secondary stroke prevention measures: blood pressure levels below 130/80mm Hg, good blood sugar control in diabetics to achieve an HbA1c below 7%, and LDL cholesterol levels below 100mg/dL (below 70mg/dL in patients with known atherosclerosis). These guidelines6 also recommend that all patients who have suffered TIA or cerebral infarct due to atherothrombosis or small vessel disease receive treatment with 80mg atorvastatin daily. The second section of the guidelines published by the Spanish Society of Neurology7 recommends the use of antiplatelet drugs in the secondary prevention of ischaemic stroke associated with large vessel arteriosclerosis and small vessel disease. Oral anticoagulants are also recommended for strokes of cardioembolic origin.
Given that the most important Spanish studies on the implementation of secondary prevention measures for cerebrovascular disease2–4 pre-date the new CPG on stroke,5–7 we decided to undertake a study of current compliance with the recommendations cited by the guidelines. To this end, we listed the following objectives:
-Describe the prevalence of vascular risk factors among hospitalised patients completing medium to long neurorehabilitation programmes following an acute ischaemic stroke.
-Examine adherence to CPG recommendations for stroke prevention by analysing the degree of control over vascular risk factors, anti-thrombotic treatment according to stroke aetiology (atherothrombosis, cardioembolism, etc.), and antihypertensive/statin treatment among the patients described above.
Patients and methodsHospital Universitario San Rafael (Hospitaller Order of Saint John of God) is a medium-to-long stay hospital. Its patients include stroke patients in acute and subacute phases who are undergoing neurorehabilitation and/or receiving care for clinical and functional sequelae. These patients were referred from hospitals in the province of Granada. We completed a descriptive transversal study with a view to the objectives described above and using the 2008 CPG for stroke5 as our reference.
Inclusion criteria: patients of any age and either sex admitted by the Internal Medicine division of Hospital Universitario San Rafael in 2009 or 2010 with a primary diagnosis of acute ischaemic stroke. Patients were selected by means of a search using Acticx software that filtered records to locate cases with the following diagnoses (ICD-9) upon admission: hemiplegia and hemiparesis (342), stenosis of precerebral arteries (433), occlusion of cerebral arteries (434), ill-defined cerebrovascular disease (436), and other and ill-defined cerebrovascular disease (437).
Exclusion criteria: patients without a discharge report from the referring hospital and patients diagnosed with haemorrhagic stroke.
Study variables were age, sex, referring department (neurology, internal medicine, rehabilitation, or the emergency department), and referring hospital. We also recorded history of HTN, type 2 diabetes mellitus (DM-2), dyslipidaemia (when type was not specified in the discharge report), high cholesterol, high triglycerides, prior stroke/transient ischaemic attack (TIA), atrial fibrillation and smoking (includes active smokers and former smokers). Data included the admitting diagnosis from the referring hospital, including aetiology of ischaemic stroke, and the treatment prescribed. Treatment information included whether or not intravenous fibrinolysis was performed, any anti-platelet drugs prescribed, any anticoagulants prescribed, motive or explanation for not prescribing anticoagulants in cases of embolic stroke, statin drugs and dose, and antihypertensive drugs and type. We also recorded any supplementary antihypertensive drugs (those taken depending on blood pressure readings) as indicated by the discharge report. Data also include blood pressure readings (measured with an OMRON M6 digital sphygmomanometer) at time of admission to Hospital San Rafael, plus fasting plasma glucose, total cholesterol and triglyceride levels (Hitachi 917) from the first analysis performed at our centre. HbA1c levels to determine diabetes control are not included, since this measurement is not routinely taken in all patients admitted to our hospital. Likewise, LDL cholesterol levels were not included due to data not being available for many of our patients, while we did have total cholesterol data for all patients.
The following measurements were considered to indicate good control over cardiovascular risk factors, according to CPGs for stroke5,6 and vascular disease prevention8: blood pressure below 130/80mm Hg, plasma glucose below 126mg/dL, total cholesterol below 175mg/dL, and triglycerides below 150mg/dL.
Statistical analysisResults for numerical variables were expressed as arithmetic means±standard deviation (X±SD) and categorical variables were given as frequencies (%). The t-test was used to compare means of different numerical variables when population variances were equal. The Welch t-test was used for samples with unequal variances. Pearson's χ2 test was employed to compare categorical variables; Fisher's exact test was also used when necessary. Values of P<.05 were considered statistically significant. Statistical analysis was performed using SPSS software version 15.0.
ResultsDemographical data, services, and referring hospitalsThe study includes data from 203 patients with a mean age of 75.7±10.3 years; 56% were women. Mean age was significantly lower for male patients than for female patients (71.8±12.2 years and 78.8±7.5 years, respectively; P<.0001). Patients were referred by the following units: neurology (75.4%), internal medicine (16.7%), rehabilitation (6.9%), and emergency department/other (1%). Patients’ referring hospitals were Hospital Clínico San Cecilio (72.9%), which has a neurology department but no stroke unit; Virgen de las Nieves Rehabilitation and Traumatology Centre (20.7%), which has a neurology department and a stroke unit; Hospital Santa Ana in Motril; (3.9%) and the Virgen de las Nieves General Hospital (1.5%), both of which lack neurology departments.
Ischaemic stroke aetiology and vascular risk factorsRegarding ischaemic stroke aetiologies, 31.5% were cardioembolic in origin; 29.6% were atherothrombotic; 8.4% were lacunar; and in 30.5%, the cause was either undetermined or unspecified (either several causes were present or the study was incomplete).
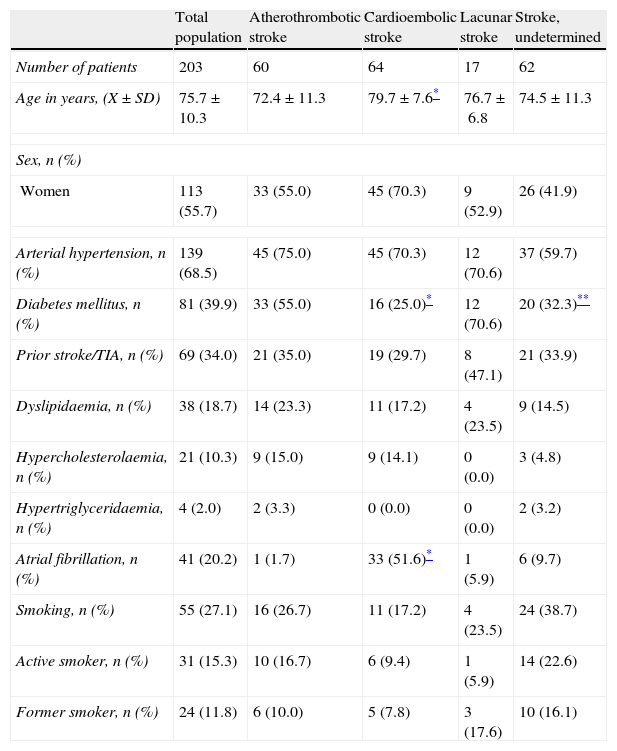
Table 1 shows the prevalence of each of the vascular risk factors in the total study population and its subgroups broken down by stroke aetiology. Patients with cardioembolic stroke were significantly older than patients with atherothrombotic stroke (P=.0001). We also observed that patients with atherothrombotic stroke had a higher prevalence of type 2 DM than did patients with cardioembolic stroke (P=.001). The latter group showed a higher prevalence of atrial fibrillation (P=.0001).
Demographic data and vascular risk factor prevalence for the total population and subgroups broken down by ischaemic stroke aetiology.
| Total population | Atherothrombotic stroke | Cardioembolic stroke | Lacunar stroke | Stroke, undetermined | |
| Number of patients | 203 | 60 | 64 | 17 | 62 |
| Age in years, (X±SD) | 75.7±10.3 | 72.4±11.3 | 79.7±7.6* | 76.7±6.8 | 74.5±11.3 |
| Sex, n (%) | |||||
| Women | 113 (55.7) | 33 (55.0) | 45 (70.3) | 9 (52.9) | 26 (41.9) |
| Arterial hypertension, n (%) | 139 (68.5) | 45 (75.0) | 45 (70.3) | 12 (70.6) | 37 (59.7) |
| Diabetes mellitus, n (%) | 81 (39.9) | 33 (55.0) | 16 (25.0)* | 12 (70.6) | 20 (32.3)** |
| Prior stroke/TIA, n (%) | 69 (34.0) | 21 (35.0) | 19 (29.7) | 8 (47.1) | 21 (33.9) |
| Dyslipidaemia, n (%) | 38 (18.7) | 14 (23.3) | 11 (17.2) | 4 (23.5) | 9 (14.5) |
| Hypercholesterolaemia, n (%) | 21 (10.3) | 9 (15.0) | 9 (14.1) | 0 (0.0) | 3 (4.8) |
| Hypertriglyceridaemia, n (%) | 4 (2.0) | 2 (3.3) | 0 (0.0) | 0 (0.0) | 2 (3.2) |
| Atrial fibrillation, n (%) | 41 (20.2) | 1 (1.7) | 33 (51.6)* | 1 (5.9) | 6 (9.7) |
| Smoking, n (%) | 55 (27.1) | 16 (26.7) | 11 (17.2) | 4 (23.5) | 24 (38.7) |
| Active smoker, n (%) | 31 (15.3) | 10 (16.7) | 6 (9.4) | 1 (5.9) | 14 (22.6) |
| Former smoker, n (%) | 24 (11.8) | 6 (10.0) | 5 (7.8) | 3 (17.6) | 10 (16.1) |
TIA: transient ischaemic attack; X±SD: mean±standard deviation.
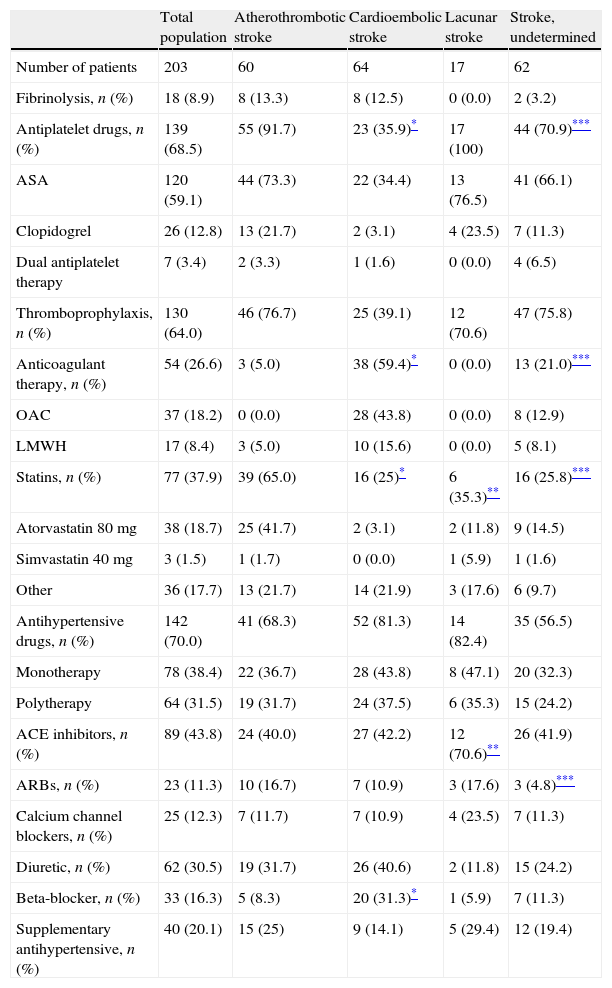
Table 2 displays the antithrombotic treatments prescribed (fibrinolysis, antiplatelet drugs, and anticoagulants) for the study total and the study population broken down by stroke aetiology. Antiplatelet drugs were administered to 91.7% of the patients with atherothrombotic stroke, while 59.4% of the patients with cardioembolic stroke were prescribed anticoagulants at therapeutic doses. Patients with atherothrombotic stroke were significantly more likely to have a prescription for antiplatelet drugs than patients with cardioembolic stroke (91.7% vs 35.9%, P=.0001). Patients with cardioembolic stroke were more likely than those in the atherothrombotic group to receive anticoagulant drugs (59.4% vs 5%, P=.0001). A comparison between cases of atherothrombotic stroke and those of undetermined aetiology revealed statistically significant differences in the use of antiplatelet drugs. These drugs were more frequently prescribed to patients with atherothrombotic stroke (P=.006), while anticoagulant treatment was more common in patients with an undetermined cause of stroke (P=.009).
Patients treated with indicated drugs as a percentage of the total population and of aetiological subgroups.
| Total population | Atherothrombotic stroke | Cardioembolic stroke | Lacunar stroke | Stroke, undetermined | |
| Number of patients | 203 | 60 | 64 | 17 | 62 |
| Fibrinolysis, n (%) | 18 (8.9) | 8 (13.3) | 8 (12.5) | 0 (0.0) | 2 (3.2) |
| Antiplatelet drugs, n (%) | 139 (68.5) | 55 (91.7) | 23 (35.9)* | 17 (100) | 44 (70.9)*** |
| ASA | 120 (59.1) | 44 (73.3) | 22 (34.4) | 13 (76.5) | 41 (66.1) |
| Clopidogrel | 26 (12.8) | 13 (21.7) | 2 (3.1) | 4 (23.5) | 7 (11.3) |
| Dual antiplatelet therapy | 7 (3.4) | 2 (3.3) | 1 (1.6) | 0 (0.0) | 4 (6.5) |
| Thromboprophylaxis, n (%) | 130 (64.0) | 46 (76.7) | 25 (39.1) | 12 (70.6) | 47 (75.8) |
| Anticoagulant therapy, n (%) | 54 (26.6) | 3 (5.0) | 38 (59.4)* | 0 (0.0) | 13 (21.0)*** |
| OAC | 37 (18.2) | 0 (0.0) | 28 (43.8) | 0 (0.0) | 8 (12.9) |
| LMWH | 17 (8.4) | 3 (5.0) | 10 (15.6) | 0 (0.0) | 5 (8.1) |
| Statins, n (%) | 77 (37.9) | 39 (65.0) | 16 (25)* | 6 (35.3)** | 16 (25.8)*** |
| Atorvastatin 80mg | 38 (18.7) | 25 (41.7) | 2 (3.1) | 2 (11.8) | 9 (14.5) |
| Simvastatin 40mg | 3 (1.5) | 1 (1.7) | 0 (0.0) | 1 (5.9) | 1 (1.6) |
| Other | 36 (17.7) | 13 (21.7) | 14 (21.9) | 3 (17.6) | 6 (9.7) |
| Antihypertensive drugs, n (%) | 142 (70.0) | 41 (68.3) | 52 (81.3) | 14 (82.4) | 35 (56.5) |
| Monotherapy | 78 (38.4) | 22 (36.7) | 28 (43.8) | 8 (47.1) | 20 (32.3) |
| Polytherapy | 64 (31.5) | 19 (31.7) | 24 (37.5) | 6 (35.3) | 15 (24.2) |
| ACE inhibitors, n (%) | 89 (43.8) | 24 (40.0) | 27 (42.2) | 12 (70.6)** | 26 (41.9) |
| ARBs, n (%) | 23 (11.3) | 10 (16.7) | 7 (10.9) | 3 (17.6) | 3 (4.8)*** |
| Calcium channel blockers, n (%) | 25 (12.3) | 7 (11.7) | 7 (10.9) | 4 (23.5) | 7 (11.3) |
| Diuretic, n (%) | 62 (30.5) | 19 (31.7) | 26 (40.6) | 2 (11.8) | 15 (24.2) |
| Beta-blocker, n (%) | 33 (16.3) | 5 (8.3) | 20 (31.3)* | 1 (5.9) | 7 (11.3) |
| Supplementary antihypertensive, n (%) | 40 (20.1) | 15 (25) | 9 (14.1) | 5 (29.4) | 12 (19.4) |
ASA: acetylsalicylic acid; OAC: oral anticoagulants; ARB: angiotensin II receptor blockers; LMWH: low molecular-weight heparin; ACE inhibitors: angiotensin converter enzyme inhibitors.
Dual antiplatelet therapy refers to use of ASA in conjunction with clopidogrel. The dose of LMWH indicated for anticoagulation corresponds to enoxaparin at 1mg/kg/12hours or bemiparin at 115U/kg/day. Thromboprophylaxis refers to treatment with enoxaparin at 20 or 40mg/day or bemiparin at 2500 or 3500U/day.
Our comparison of percentages of patients receiving antiplatelet drugs for atherothrombotic stroke according to whether they were referred by neurology or by internal medicine revealed no statistically significant differences (90% for neurology and 100% for internal medicine; P=.738). Likewise, no significant differences could be detected between the percentages of patients on anticoagulants for cardioembolic stroke based on the referring department (58.5% for neurology, 55.6% for internal medicine; P=.573).
A total of 26 patients had cardioembolic stroke and no anticoagulant treatment (40.6% of the total patients with that aetiology). The reasons for not providing anticoagulants were listed in the reports for 14 of those patients (53.8%): high risk of haemorrhage or haemorrhagic transformation (28.5%); significant residual deficit (28.5%); and disease or poor baseline condition (21.4%).
Statin drugs in secondary prevention of ischaemic strokeTable 2 lists the percentages of patients treated with statins in keeping with CPG recommendations for stroke.5 Prescription of statins was significantly higher among patients with atherothrombotic stroke than among those with embolic stroke (P=.0001), lacunar stroke (P=.028) and stroke of undetermined cause (P=.0001).
An analysis of referring departments’ prescription of statin drugs for patients with atherothrombotic stroke revealed no statistically significant differences (62.0% for neurology; 66.7% for internal medicine; P=.684). Similarly, there were no significant differences between referring departments regarding the percentage of patients treated with the recommended doses of atorvastatin or simvastatin (74.2% for neurology vs 50% for internal medicine, P=.477).
Diagnosis and treatment of hypertension as secondary stroke preventionA history of HTN was present in 68.5% of the patients in the total study population, although 21.1% of the patients diagnosed with HTN did not receive antihypertensive drugs. Table 2 lists the antihypertensive drug groups prescribed to all patients in the sample, who are broken down by stroke aetiology. Supplementary antihypertensive treatment was prescribed to 20% of the patients (captopril in 73.8% and labetalol in 16.6%).
Comparison of the antihypertensive drugs prescribed (Table 2) reveals a stronger tendency towards prescribing beta blockers to patients with embolic stroke than to those with atherothrombotic stroke (P=.001); ACE inhibitors were more common for patients with lacunar stroke than for those with thrombotic stroke (P=.026). ARBs were more commonly prescribed to patients with thrombotic stroke than to those with a stroke of undetermined origin (P=.034).
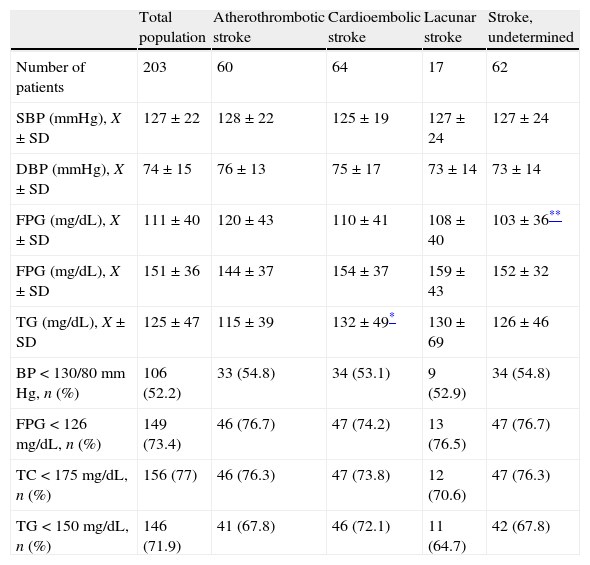
Control over vascular risk factors in secondary prevention of ischaemic strokeTable 3 displays the descriptive and comparative studies of quantitative variables (blood pressure, fasting blood glucose, and total cholesterol and triglycerides) in the total study population, broken down by stroke aetiology. This table also shows the percentage of patients presenting a good degree of control over vascular risk factors upon admission. Patients with cardioembolic stroke had significantly higher triglyceride levels than those with atherothrombotic stroke (P=.046). We also found higher glucose levels in atherothrombotic stroke patients than in those with stroke of undetermined origin, and the difference was statistically significant (P=.019).
Descriptive study of vascular risk factors at time of admission and patients with good control over identified risk factors as a percentage of the total and broken down by stroke aetiology.
| Total population | Atherothrombotic stroke | Cardioembolic stroke | Lacunar stroke | Stroke, undetermined | |
| Number of patients | 203 | 60 | 64 | 17 | 62 |
| SBP (mmHg), X±SD | 127±22 | 128±22 | 125±19 | 127±24 | 127±24 |
| DBP (mmHg), X±SD | 74±15 | 76±13 | 75±17 | 73±14 | 73±14 |
| FPG (mg/dL), X±SD | 111±40 | 120±43 | 110±41 | 108±40 | 103±36** |
| FPG (mg/dL), X±SD | 151±36 | 144±37 | 154±37 | 159±43 | 152±32 |
| TG (mg/dL), X±SD | 125±47 | 115±39 | 132±49* | 130±69 | 126±46 |
| BP<130/80mm Hg, n (%) | 106 (52.2) | 33 (54.8) | 34 (53.1) | 9 (52.9) | 34 (54.8) |
| FPG<126mg/dL, n (%) | 149 (73.4) | 46 (76.7) | 47 (74.2) | 13 (76.5) | 47 (76.7) |
| TC<175mg/dL, n (%) | 156 (77) | 46 (76.3) | 47 (73.8) | 12 (70.6) | 47 (76.3) |
| TG<150mg/dL, n (%) | 146 (71.9) | 41 (67.8) | 46 (72.1) | 11 (64.7) | 42 (67.8) |
TC: total cholesterol; FPG: fasting plasma glucose; BP: blood pressure; DBP: diastolic blood pressure; SBP: systolic blood pressure; TG: triglycerides; X±SD: mean±standard deviation.
Comparison of the degree of control over vascular risk factors between patients referred by a neurology department and those referred by internal medicine did not reveal any statistically significant differences in the percentage of patients with good control over the following: blood pressure (51% from the neurology department; 55.9% from internal medicine, P=.605); fasting plasma glucose (72% from neurology and 75.8% from internal medicine, P=.661); cholesterol levels (78.2% from neurology and 72.7% from internal medicine, P=.496); and triglycerides (73.5% from neurology and 72.7% from internal medicine, P=.931).
DiscussionFrom our point of view, one of the study's limitations is that it was carried out in a single hospital. However, the fact that it included patients who had been referred by several different hospitals may increase its external validity and permit extrapolation of results. Another of our study's limitations is the possible existence of a selection bias. The study only included patients with ischaemic stroke requiring hospital rehabilitation due to sequelae, and secondary prevention measures were probably applied less strictly to patients who had suffered greater clinical and functional impairment. This may explain the percentage of patients with cardioembolic stroke and but no anticoagulant treatment, and the fact that residual clinical and/or functional impairment was one of the main reasons cited for not using anticoagulants.
In Spain, as stated in the introduction, several studies have addressed follow-up on secondary prevention measures for cerebrovascular disease. The most relevant are DIAPRESIC4 (a multi-centre retrospective study promoted by the Spanish Society of Neurology's study group for cerebrovascular diseases and completed with data taken from the discharge reports of patients hospitalised for acute cerebral infarction) and REACH2 (a record of vascular risk factor management among patients at risk for vascular events and with confirmed vascular/cerebrovascular disease).
Regarding risk factors associated with acute ischaemic stroke, our findings were similar to those described in the DIAPRESIC4 study, which calculated a prevalence of 62.6% for HTN, 30.6% for type-2 DM, and 29.9% for dyslipidaemia. On the other hand, our data did not support those from the REACH study.2 The cerebrovascular disease subgroup in REACH showed higher prevalence of HTN (74.8%), smoking (54.8%), and high cholesterol (50.3%), although the prevalence of type-2 DM was somewhat lower (37.2%).
An interesting finding is that more than a third (34%) of the total patients included in our study (and 47% of those with lacunar stroke) had a prior history of stroke or TIA. We therefore need to stress the importance and transcendence of secondary prevention in cerebrovascular disease.
When we compare antithrombotic drug prescriptions in our total population with those from the other 2 studies, we see that a smaller percentage of our patients were prescribed antiplatelet drugs than in DIAPRESIC4 (77.5%) or in REACH2 (83.2%). Meanwhile, a larger percentage of patients were treated with anticoagulants in our sample than in the DIAPRESIC4 (18.4%) or the REACH studies2 (17.9%).
In contrast to the other 2 studies,2,4 our study provides a breakdown of population by stroke aetiology. However, we have found no studies published in Spain that evaluate use of anti-thrombotic drugs for secondary stroke prevention according to stroke aetiology. Anti-platelet drugs were prescribed to more than 90% of the patients with atherothrombotic stroke, while anticoagulant drugs were only prescribed to 60% of the patients with cardioembolic stroke. We believe that the discrepancy between observations in our study and the CPG recommendations5,7 on how anti-thrombotic drugs should be used depending on stroke aetiology arises because of multiple reasons. These include the idea that anti-platelet drugs are more safe and incur less risk of haemorrhage than anticoagulants, as well as being easier to dose and requiring fewer dose adjustments. Although residual clinical and functional sequelae were not analysed in detail in this study (leaving room for later studies to do so), this may be yet another factor with a clear influence on the decision of whether or not to opt for anticoagulant treatment in certain patients with cardioembolic stroke added to a low risk of haemorrhage or haemorrhagic transformation. We would like to stress that reasons for not providing anticoagulants to patients with cardioembolic stroke were only listed in half of such cases. This information is crucial to understanding the treatment approaches of professionals who will be monitoring patients later on.
Our study also analysed the percentage of patients receiving statins dosed according to the CPG recommendations.5,7 Only 43.4% of patients with atherothrombotic stroke received atorvastatin and simvastatin at correct doses. We therefore believe that the percentage of patients with atherothrombotic stroke who benefit from the prescription of these drugs remains low in our area. It is interesting to note that although 65% of patients with atherothrombotic stroke are treated with statins, only 43.4% of them receive atorvastatin and simvastatin at their recommended doses. We cannot offer an explanation for this observation. Returning to earlier studies, REACH2 reported that statins were administered to 51.9% of the patients with cerebrovascular disease (aetiology was not specified). The same figure in the DIAPRESIC4 study was 53.8% among patients with a prior history of dyslipidaemia.
Our study also reported a higher percentage of patients with HTN and anti-hypertensive treatment than was indicated by the DIAPRESIC study4 (73.2%). The most commonly prescribed antihypertensive drugs in our sample were ACE inhibitors, followed by diuretics and beta-blockers. This was in line with CPG recommendations,5,6 which report a lower risk of stroke recurrence with a combination of perindopril and indapamide5,6 or with ramipril6 or a diuretic5 in monotherapy. Our results resemble those from the DIAPRESIC study4 in which use of ACE inhibitors (56.5%) and diuretics (27.8%) predominated. The current study also recorded supplementary antihypertensive treatment, prescribed to 20.1% of the patients; this type of treatment was not included in earlier studies.
Regarding control over vascular risk factors, we found a higher percentage of patients with good blood pressure levels in our sample (52.2%) than in the REACH study2 (only 42.9% of these subjects had blood pressure levels below 140/90mm Hg. However, we believe that still more can be done to bring blood pressure under control and meet the objectives stated in the CPG.5,6 Results for glucose and lipid control were also better than those in the REACH study, which reported glucose below 126mg/dL in 69.9% of the patients, cholesterol levels above 200mg/dL in 48.2%, and triglycerides above 150mg/dL in 31.5%. When examining lipid control, we should stress that the percentage of patients with good control over cholesterol levels could be underestimated. Cholesterol was measured upon the patient's admission to our hospital; in some cases, patients’ lipid-lowering treatment would not have had enough time to produce an effect.
We found no significant differences in prescription tendencies for antithrombotic, antihypertensive, or statin drugs. Likewise, there were no differences in the degree of control over vascular risk factors regarding the referring department (neurology or internal medicine). Lack of such differences may lie in the fact that a large percentage of the patients referred by neurology departments came from a hospital with no stroke unit (Hospital Clínico San Cecilio). In contrast, the Virgen de las Nieves Rehabilitation and Traumatology Centre, which has a stroke unit, referred fewer patients.
In summary, from the viewpoint of clinical practice, our study points to better control over vascular risk factors and improvements in the treatments prescribed for secondary prevention among patients with acute ischaemic stroke. However, we believe that further progress may still be made, especially by increasing the percentage of patients with cardioembolic stroke treated with anticoagulants, prescribing statins at the recommended doses for the subgroup of patients with atherothrombotic stroke, and increasing the percentage of patients with well-controlled blood pressure. Given that more than a third of the stroke patients included in our study had experienced a prior episode of cerebral ischaemia, we believe it important to stress the importance and transcendence of secondary prevention. This will aid in avoiding an illness with high morbidity and mortality rates and a huge social and healthcare burden owing to the dependency that it may provoke.
Conflicts of interestThe authors have no conflicts of interest to declare.
We would like to thank Dr Vanessa Pérez Arco from the Medical Reporting Service at Hospital San Rafael for helping us manage the medical histories used in the preparation of this study.
Please cite this article as: Pardo Cabello AJ, et al. Implementación de las guías de práctica clínica sobre ictus isquémico agudo en atención especializada. Neurología. 2013;28:137–44.