Thrombectomy has radically changed the management of ischaemic stroke due to large-vessel occlusion.1 Angiography requires the use of iodinated contrast agents, although gadolinium may be used in patients with a contraindication to these substances. Gadolinium has been used widely in arterial interventions and peripheral angiography.2 It has also been used in carotid artery angiography,3,4 in the treatment of dural arteriovenous fistulas,5 and even in the assessment of patients with ischaemic stroke, when results from non-invasive tests are inconclusive.6
Gadolinium-enhanced cerebral angiography for thrombectomy may be an alternative in patients with history of severe adverse reactions to iodinated contrast agents. Although this indication is known, it is rarely mentioned in the literature.7 We recently treated 2 patients with aspiration thrombectomy using gadolinium as the contrast medium.
The first patient was a 69-year-old woman with hypertension and history of papillary carcinoma of the thyroid, which was treated surgically 20 years previously. She came to our hospital due to language impairment and right limb weakness of 6 hours’ progression. The neurological examination revealed severe dysphasia with right faciobrachiocrural hemiparesis, scoring 17 points on the National Institutes of Health Stroke Scale (NIHSS). CT findings scored 8 on the Alberta Stroke Program Early CT Score (ASPECTS), with a hyperdense signal in the left middle cerebral artery; CT angiography was not performed as the patient had presented anaphylaxis to contrast during a follow-up study of the thyroid cancer. Laboratory analysis detected no remarkable alterations, with creatinine clearance of 110 mL/min. Given strong suspicion of large-vessel occlusion, we performed an angiography study with gadobutrol; our patient’s relatives gave informed consent for the compassionate use of this contrast medium. The study revealed left distal M1 segment occlusion (Fig. 1). Manual aspiration with a SOFIA 6 F catheter achieved successful recanalisation (TICI grade 3). The procedure required 26 mL Gadovist® (gadobutrol 604.72 mg/mL) for 3 angiography runs, and was performed with a monoplane angiography system; the patient was not sedated during the procedure. The patient scored 10 points on the NIHSS after the procedure, and 4 at discharge. No complications were recorded during hospitalisation; unknown atrial fibrillation was detected, and kidney function was normal. An MRI study performed a week later revealed subacute punctiform ischaemic lesions in the caudate and lentiform nuclei and the left frontal subcortical region, with no signs of haemorrhage. No complications were observed after a year of follow-up, with the patient scoring 0 on the modified Rankin Scale (mRS).
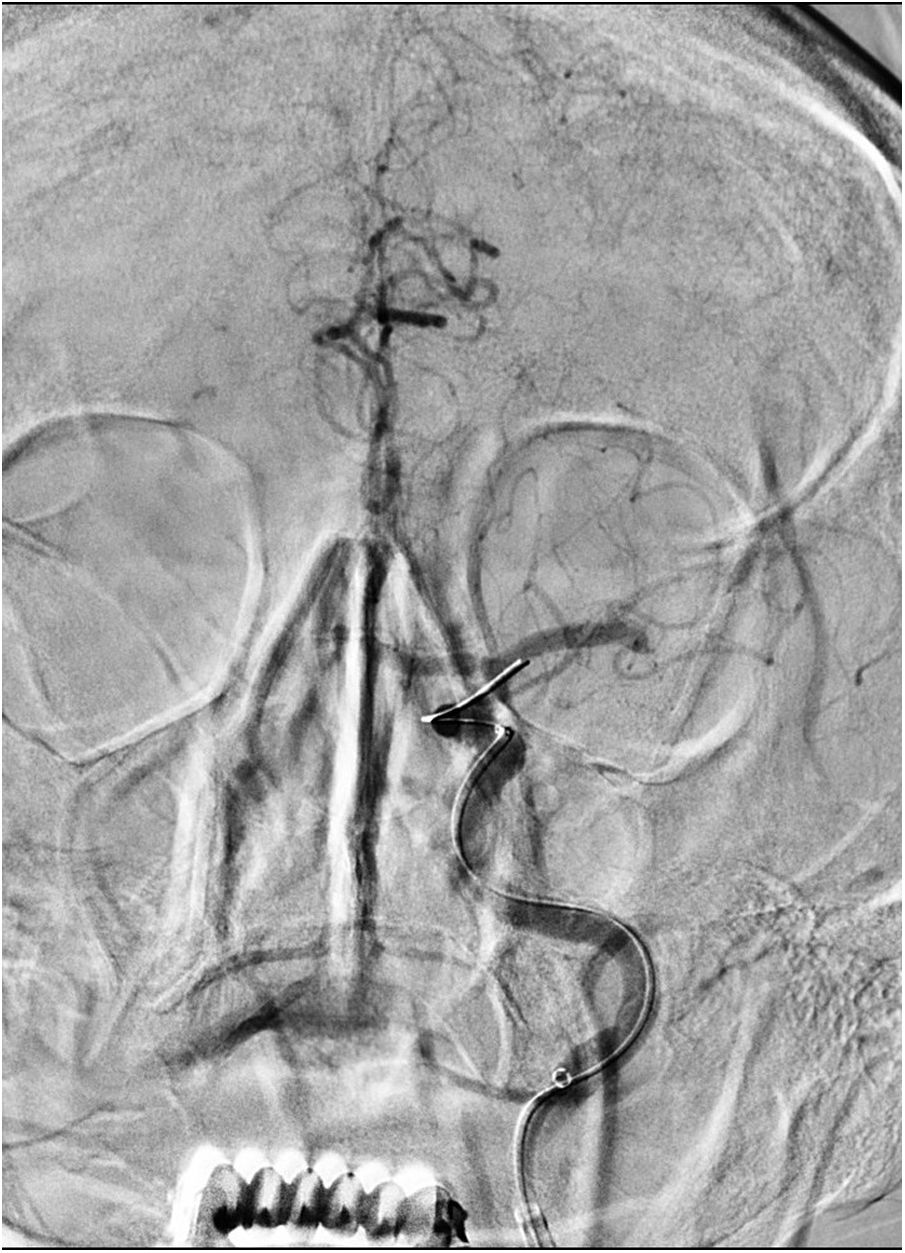
Our second patient was a 68-year-old man, a smoker, with hypertension and history of oral epidermoid carcinoma, which was treated with surgery and radiation therapy 7 years earlier. He presented sudden-onset weakness of the left limbs, difficulty speaking, and anosognosia, and scored 18 on the NIHSS. CT findings scored 10 on the ASPECTS scale, with images showing hyperdense signal in the right middle cerebral artery; CT angiography was not performed as the patient had presented a severe reaction to contrast medium during an imaging study for cancer. All laboratory parameters were within normal ranges, with creatinine clearance of 90 mL/min. Femoral puncture was performed 2 hours and 15 minutes after symptom onset. The patient’s family gave informed consent for the compassionate use of gadobutrol as a contrast medium. The angiography study revealed internal carotid artery occlusion at the cervical level (Fig. 2). We performed balloon angioplasty (3 × 20 mm) of the occluded segment and subsequently inserted a SOFIA® 6 F catheter until the internal carotid artery. Manual aspiration thrombectomy achieved complete recanalisation (TICI grade 3) with a single pass. Cervical angiography revealed underlying stenosis; balloon angioplasty (5 × 20 mm) was performed to place a Wallstent® endoprosthesis stent measuring 9 × 40 mm. No signs of aggregation or any other complications were observed after 20 minutes. We used a total of 110 mL undiluted gadobutrol for the angiography runs performed after thrombectomy and during endoprosthesis placement, and gadobutrol at a 50:50 dilution with saline solution for the rest. We performed a total of 15 angiography runs, including the study of the contralateral carotid artery. The patient received 900 mg of intravenous lysine acetylsalicylate and did not require sedation. His neurological symptoms improved, with an NIHSS score of 10 at discharge. No complications were observed during hospitalisation; the permeability of the endoprosthesis was confirmed by Doppler ultrasound; kidney function was preserved. An MRI study conducted 8 days later revealed a subacute infarction in the right temporolateral area, insula, and lentiform nucleus; the latter area displayed haemosiderin deposition. One year later, the patient scored 3 on the mRS and had presented no other remarkable events.
The families of both patients gave informed consent for the compassionate use of gadolinium.
The need for immediate treatment of ischaemic stroke precludes the administration of premedication for iodinated contrast agents in patients with history of severe allergic reactions. Male et al.7 published a similar case: they successfully performed mechanical thrombectomy for right M1 occlusion using intra-arterial gadolinium in a patient with history of anaphylaxis to iodinated contrast agents. Although gadolinium is a known alternative, few cases have been published, which is why we decided to share our experience with this contrast medium.
Gadolinium is widely used in MRI studies to characterise central nervous system lesions, and is particularly useful in patients with inflammatory and tumoural diseases. Significant efforts are currently being made to describe gadolinium deposits in the central nervous system. Although its clinical significance is uncertain, the possibility of gadolinium accumulation in the brain makes molecularly stable types of gadolinium a reasonable option. Non-ionic and macrocyclic gadolinium-based contrast agents (eg, gadobutrol) are preferred; linear contrasts are being discontinued in many countries. Gadolinium deposition in the dentate nucleus and globus pallidus may be associated with repeated exposure to high doses of this contrast agent, and may even play a role in blood-brain barrier permeability.8,9 No other specific complications of intra-arterial administration have been described.
The summary of product characteristics of gadobutrol indicates the possibility of administering doses of up to 0.3 mL/kg. We administered 0.37 mL/kg to the first patient (71 kg) and 0.77 mL/kg to the second (85 kg). This difference is explained by the difficulty of treating tandem occlusions; in these patients, angioplasty requires cervical angiography runs, in addition to a study of the contralateral carotid artery to confirm the position of the circle of Willis. We administered a 50:50 dilution to our second patient with a view to reducing the total dose of gadobutrol. In this patient, image quality was significantly lower than in conventional studies. However, images obtained with undiluted gadobutrol were practically indistinguishable from those obtained with iodinated contrast agents. Undiluted gadobutrol was used in post-thrombectomy studies and during endoprosthesis placement. Biplane imaging is not available at our centre, so we had to perform more angiography runs and therefore required more gadobutrol.
Kidney function was monitored for a week and showed no significant alterations. One year after the procedure, neither patient developed contrast-related complications, such as nephrogenic systemic fibrosis.10 MRI studies performed during hospitalisation showed no unexpected findings.
We report 2 cases of successful thrombectomy with gadobutrol-enhanced imaging and no complications associated with this contrast medium. Compassionate use of gadobutrol may be considered in patients with clear contraindications to iodinated contrast agents.
Please cite this article as: de Albóniga-Chindurza A, Ortega-Quintanilla J, Alcalde-López J, Zapata-Arriaza E, González A. Gadolinio intraarterial como alternativa al contraste yodado en la trombectomía. Neurología. 2020;35:681–683.