Capsular warning syndrome (CWS) is characterised by repeated and self-limiting episodes of motor deficit (sensory deficit is less frequent), which are caused by ischaemia limited to the internal capsule. The risk of infarction following CWS is higher than in the case of other transient ischaemic attacks (TIA).1 CWS treatment during the acute phase is controversial. The effectiveness and safety of intravenous thrombolysis (IVT) is not well-known.2,3
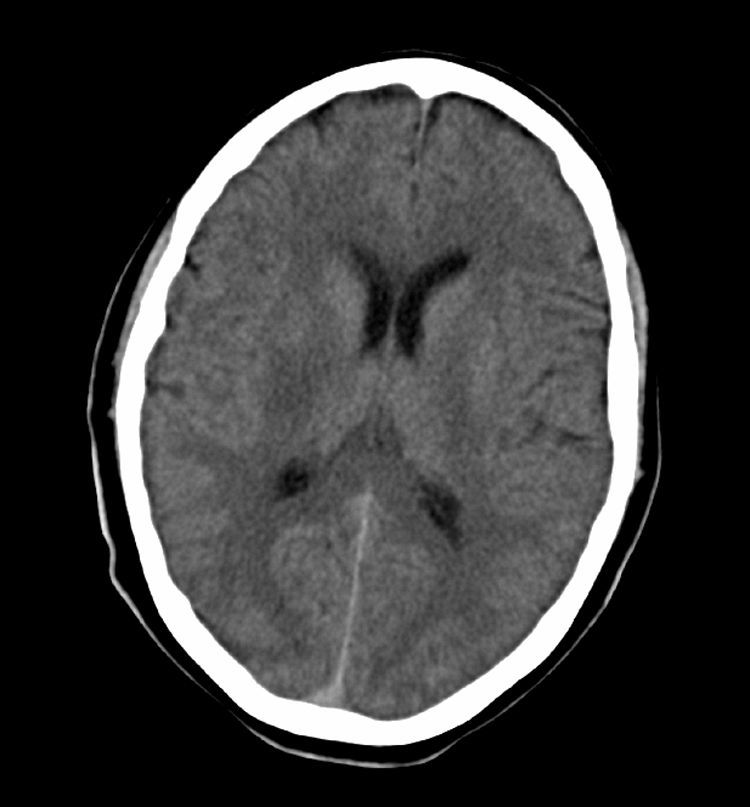
We present the case of a man aged 52 with a history of smoking, alcohol abuse, and obstructive sleep apnoea syndrome (OSAS), who was undergoing treatment with CPAP. He experienced 2 sudden-onset transient episodes of left-sided weakness and difficulty articulating words, each lasting less than 30minutes. He was treated in his referral hospital, where he suffered a third identical episode before being sent to our hospital. On the way, he suffered another episode in the ambulance. Upon arrival at the hospital, he presented mild right faciobrachiocrural hemiparesis and mild dysarthria (4 on the NIHSS scale). Computed tomography (CT) and intracranial CT angiography yielded normal results. The patient was transferred to the stroke unit for monitoring. After 40minutes, the patient's clinical condition worsened; he presented left hemiplegia, an NIHSS score of 9, and low blood pressure (minimum values: 89/60mmHg). Doctors performed an IVT (rt-PA dose: 0.9mg per kg body weight). After bolus administration, motor deficit showed significant improvement (NIHSS score of 3); however, 15minutes later (during the rt-Pa infusion), he scored 11 on the NIHSS (left hemiplegia and dysarthria) with no subsequent improvement. The patient underwent an emergency cranial CT that revealed a faint hypodense focus affecting the posterior third of the right putamen (Fig. 1). As his blood pressure remained low, intravenous fluid therapy was administered and he was placed in the Trendelenburg position; doctors observed no improvements.
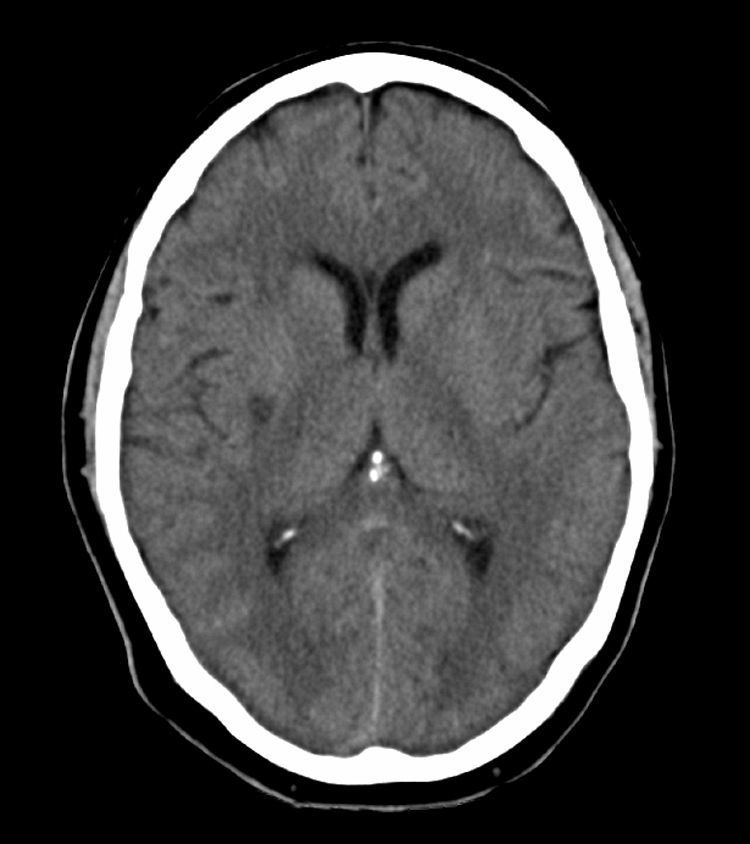
A complementary study (electrocardiogram, echocardiogram, and transcranial and supra-aortic trunk neurosonology) showed no significant changes. The routine CT scan performed 24hours after the IVT revealed an ischaemic lesion affecting the posterior third of the right putamen (Fig. 2). Eight days after admission, the patient was discharged from hospital with left hemiparesis, facial paresis, and dysarthria (NIHSS=8, modified Rankin scale=3).
CWS is considered a recurrent form of lacunar TIA that is related to cerebral small vessel disease. The pathophysiology of CWS is not well-known. The most widely accepted mechanism has to do with haemodynamic changes occurring in a small damaged perforating artery. However, other proposed potential mechanisms include lipohyalinosis, microatheromatosis, vasospasm, and cardiac or artery-to-artery embolism.1
Up to 42% of all CWS patients develop established lacunar infarcts, which in most cases occur in the internal capsule; however, other localisations have included the striato-capsular area and the anterior choroidal artery.1
Raising blood pressure by means of IV rehydration therapy or drugs such as phenylephrine has been suggested as the treatment of choice for counteracting cerebral hypoperfusion in the small vessels. Use of heparin or antiplatelet drugs has not delivered conclusive results.2
IVT has been shown to be beneficial for all aetiological subtypes of stroke.4,5 However, according to some authors, this therapy is not as beneficial and does not affect prognosis in cases of lacunar stroke.6,7
Few articles describe the effectiveness of IVT in CWS. The literature includes descriptions of only 5 patients, 4 of which presented good clinical progress following IVT. Based on these results, the authors conclude that IVT is safe and improves prognosis in this patient subgroup.2,3
IVT did not change the natural course of CWS in our patient. Our case seems to support the haemodynamic hypothesis as a possible mechanism involved in this syndrome.
Please cite this article as: Gutiérrez Ruano B, García Pastor A, Villanueva Osorio JA, Bravo Quelle N, Vázquez Alén P, Díaz Otero F, et al. Trombólisis intravenosa en el síndrome de alarma capsular: ¿es beneficiosa? Neurología. 2013;28:444–446.