Chiari malformation type I (CM1) is defined as the extrusion of the cerebellar tonsils through the foramen magnum and into the spinal canal. It can be confirmed by a radiograph showing descent of brain tissue 5mm or more, lending a pointed appearance to the cerebellar tonsils and decreasing the subarachnoid space at the craniocervical junction.1 The clinical manifestations of CM-I are associated with direct compression of the brainstem and cervical spinal cord, or with changes in cerebrospinal fluid.
A 38-year-old man with no relevant medical history described headaches occurring throughout the preceding year. Pain was dull and moderately intense (VAS score 6) and located in the occipital region radiating to the frontal region. Headache was triggered by laughing, but not by Valsalva manoeuvres or physical exercise. Episodes lasted 10 to 30minutes and were not accompanied by focal neurological signs. In the preceding month, pain had grown more intense (VAS 8) and was triggered not only by laughing, but also by minimal exertion and Valsalva manoeuvres such as coughing or defecating. Lateral and rotational movements of the head also caused headache episodes. The general examination was normal; a neurological examination revealed left-beating horizontal nystagmus with no other relevant findings.
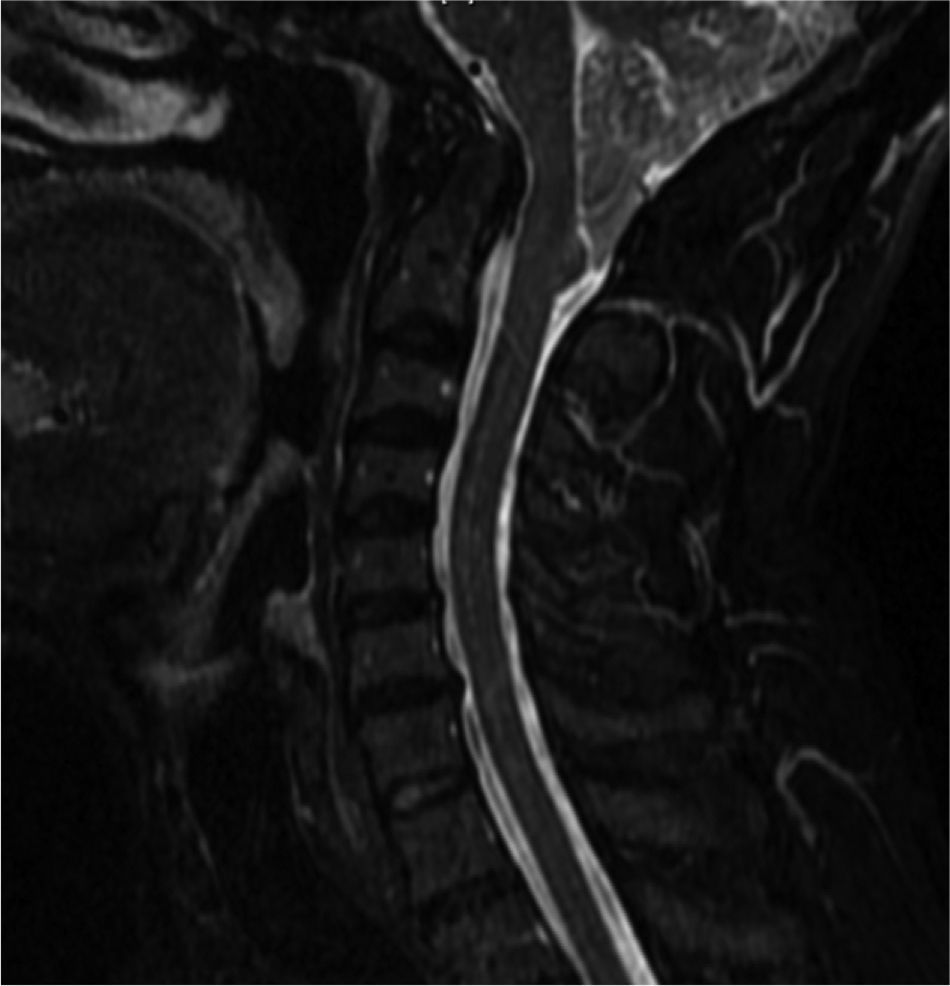
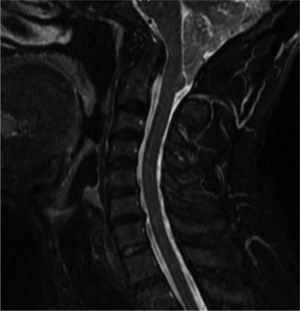
Brain and cervical MRI (Fig. 1) showed that cerebellar tonsils had descended 16mm below the foramen magnum, forming a point. The medulla had taken on an angled shape and the subarachnoid space at the craniocervical junction was reduced. Signs were consistent with a diagnosis of type I Chiari malformation.
The patient was initially treated with 600mg ibuprofen every 8hours but did not respond. Treatment was changed to 25mg indometacin every 8hours, still with no response. As the patient's headaches were incapacitating, he underwent decompressive occipital surgery associated with C1 laminectomy. The headaches, vertigo, and nystagmus all resolved and have not returned in 2 years of follow-up.
Our patient's pain met criteria for headaches caused by type 1 Chiari malformation according to the second edition of the International Headache Classification (Table 1).2 There have been cases in which headaches triggered by laughing,3 one of which was prolonged, signalled the presence of CM1.4 In another published case of a patient with CM1 and IV-ventricle ependymoma without hydrocephalus, headaches triggered by laughing resolved once the tumour had been removed.5 Although the phenomenon of headache caused by laughing is exceptional, and would rarely appear as the first manifestation of CM1, this did occur in our patient.
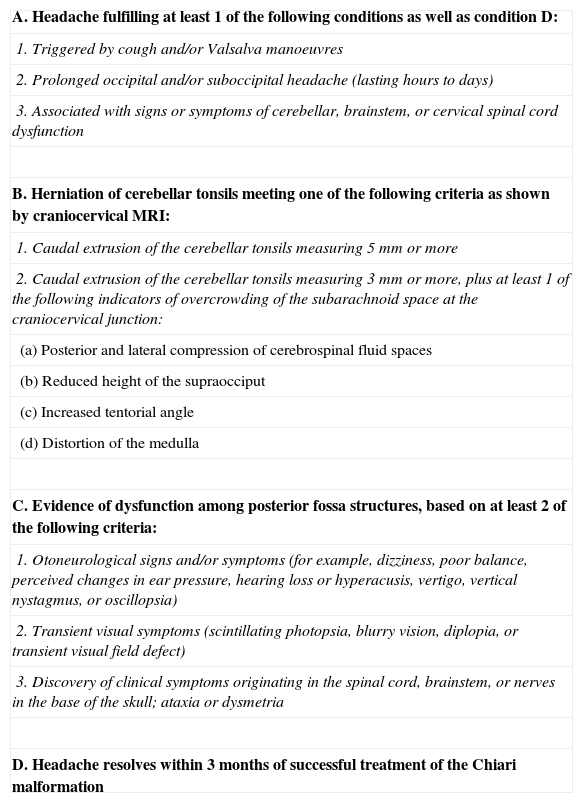
Diagnostic criteria for headaches caused by type I Chiari malformation.
| A. Headache fulfilling at least 1 of the following conditions as well as condition D: |
| 1. Triggered by cough and/or Valsalva manoeuvres |
| 2. Prolonged occipital and/or suboccipital headache (lasting hours to days) |
| 3. Associated with signs or symptoms of cerebellar, brainstem, or cervical spinal cord dysfunction |
| B. Herniation of cerebellar tonsils meeting one of the following criteria as shown by craniocervical MRI: |
| 1. Caudal extrusion of the cerebellar tonsils measuring 5mm or more |
| 2. Caudal extrusion of the cerebellar tonsils measuring 3mm or more, plus at least 1 of the following indicators of overcrowding of the subarachnoid space at the craniocervical junction: |
| (a) Posterior and lateral compression of cerebrospinal fluid spaces |
| (b) Reduced height of the supraocciput |
| (c) Increased tentorial angle |
| (d) Distortion of the medulla |
| C. Evidence of dysfunction among posterior fossa structures, based on at least 2 of the following criteria: |
| 1. Otoneurological signs and/or symptoms (for example, dizziness, poor balance, perceived changes in ear pressure, hearing loss or hyperacusis, vertigo, vertical nystagmus, or oscillopsia) |
| 2. Transient visual symptoms (scintillating photopsia, blurry vision, diplopia, or transient visual field defect) |
| 3. Discovery of clinical symptoms originating in the spinal cord, brainstem, or nerves in the base of the skull; ataxia or dysmetria |
| D. Headache resolves within 3 months of successful treatment of the Chiari malformation |
Laughter constitutes a Valsalva manoeuvre, and, like coughing, it raises intracranial pressure. Coughing and other activities involving Valsalva manoeuvres may cause primary cough headache. They may also trigger a headache in the context of CM1.6,7 The difference between the headaches is that primary cough headache has an older age at onset (>60 years) and a shorter duration (seconds rather than minutes).8 This trend can be seen in our patient; since he is a young adult with headaches lasting several minutes, symptoms are consistent with CM1. The pathophysiology of headache secondary to CM1 is uncertain. The postulated mechanism is a temporary increase in the pressure difference between the intracranial and intramedullary compartments. This would further force the cerebellar tonsils against the foramen magnum, causing pain due to traction on pain-sensitive structures.9 In some case series, the resolution rate for headaches after surgery reaches 88%.10 Headache triggered by laughing may be primary, but it may also indicate diseases of the posterior fossa. Age at onset, pain duration, and the presence of neurological signs and symptoms may point to a structural cause.
Headache secondary to CM1 is often described as being similar to primary cough headache except that it may last longer (minutes instead of seconds). One theory holds that primary cough headache responds better than secondary headache to indometacin. However, distinguishing between primary and secondary headaches may be difficult. A brain MRI is not only useful, but absolutely necessary in cases of headache provoked by the Valsalva manoeuvre. Headache is the most frequent symptom of CM1, but patients may have localised vestibulo-ocular disorders (in 74% of cases); cranial nerve, brainstem, or cerebellar disorders (in 50%); and/or cervical spinal cord disorders indicating syringomyelia (in 66%). These symptoms are the most indicative of a secondary headache.
In addition to being associated with better surgical results, early diagnosis and early treatment can prevent development of more critical cerebellar, brainstem, or cervical symptoms.
Please cite this article as: Jiménez Caballero PE, Calle Escobar ML, Portilla Cuenca JC, Casado Naranjo I. Cefalea desencadenada por la risa como forma de presentación de una malformación de CHIARI tipo I. Neurología. 2013;28:446–447.