Occipital condyle syndrome (OCS) is a rare condition first identified by Greenberg in 1981, in a series of patients with brain metastases.1 The syndrome is characterised by paralysis of the ipsilateral hypoglossal nerve and persistent occipital pain that usually radiates to the mastoid process, is exacerbated by inclination of the head to the contralateral side, and is associated with increased sensitivity of the scalp.
It is often caused by tumour metastasis, usually originating from breast or prostate cancer.2 In the most recent case series,2 OCS was the first manifestation of the neoplasia in more than half of patients.
A literature search on PubMed (keywords: “occipital condyle syndrome” and “colorectal cancer”) identified no cases of the syndrome as the initial manifestation of a rectal tumour. We present a case of OCS in which the aetiological study identified rectal adenocarcinoma.
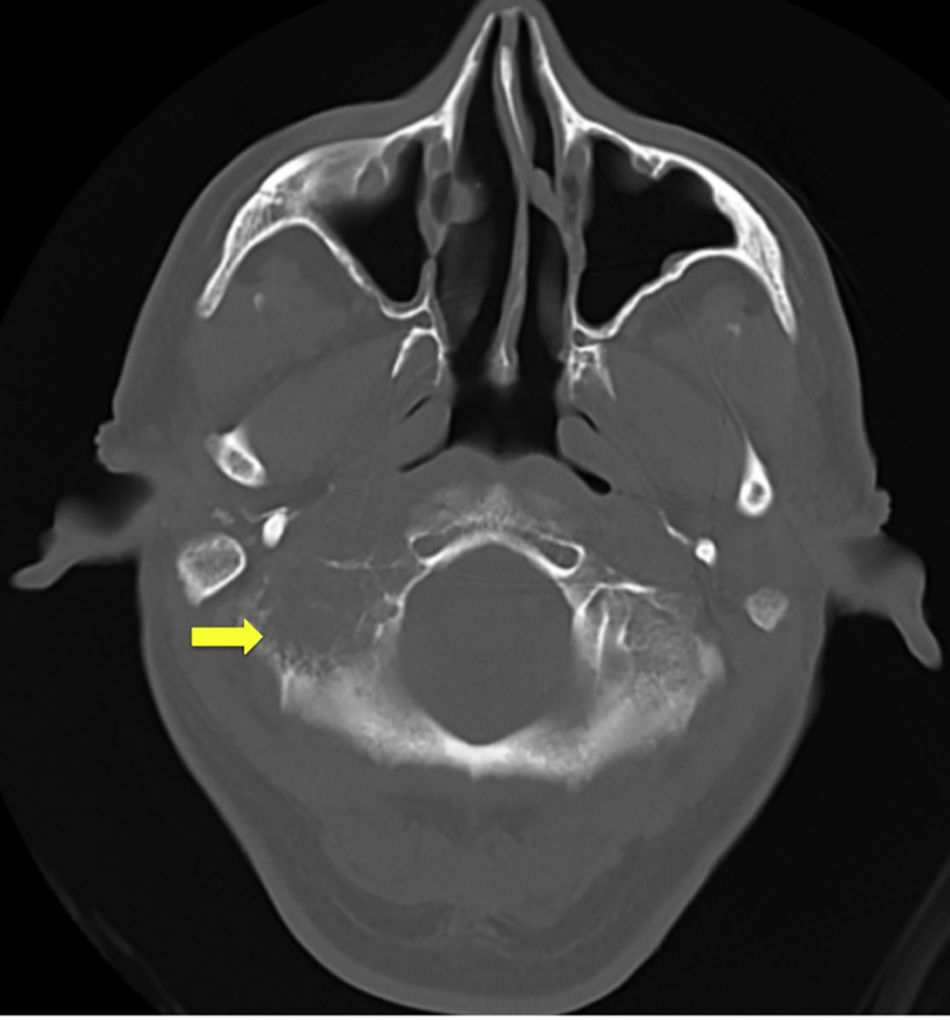
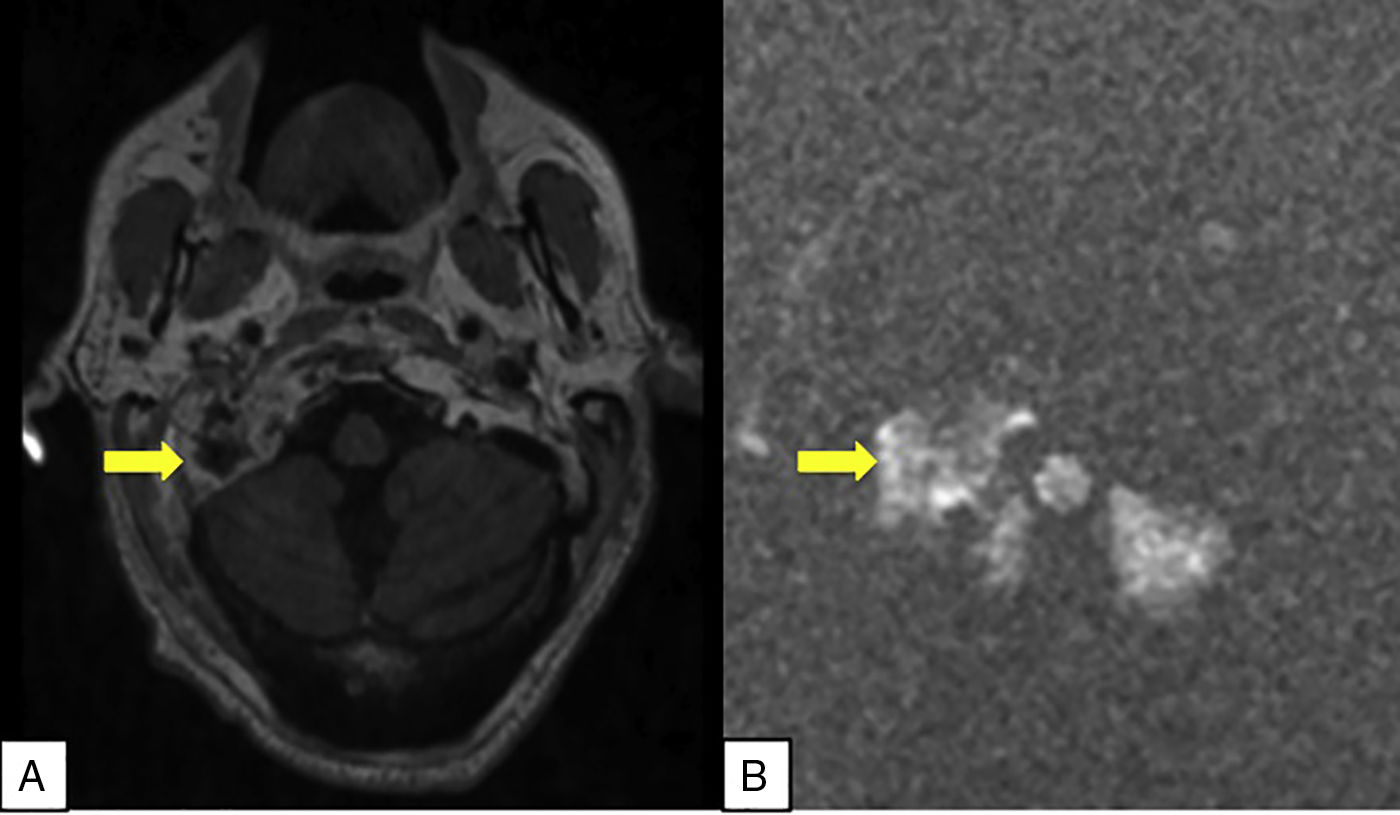
The patient was a 62-year-old man, an active smoker, with personal history of arterial hypertension and diabetes and family history of colorectal cancer. He consulted due to weight loss and alterations to tongue mobility that caused dysarthria and frequent choking. The only relevant finding from the physical examination was atrophy of the right side of the tongue and reduced tongue lateralisation strength (Fig. 1). Blood analysis revealed normocytic normochromic anaemia (haemoglobin: 11.8 g/dL) with ferritin at 622 ng/mL (normal range, 30-400 ng/mL) and a marked increase in levels of carcinoma embryonic antigen (9.562 ng/mL; normal range, < 5.20 ng/mL) and carbohydrate antigen 19-9 (3552 U/mL; normal range, < 39 U/mL). A chest radiography showed elevation of the right hemidiaphragm. A head CT scan showed a lytic lesion on the basal portion of the right squama occipitalis, proximal to the occipital condyle. A brain MRI study (Fig. 2A and B) confirmed presence of a lytic lesion associated with a soft tissue mass on the occipital condyle and the left temporal and parietal bones. A space-occupying lesion surrounded by vasogenic oedema was observed on the left cerebellar hemisphere. A colonoscopy revealed a hard, mammillated, infiltrating tumour on the anus; biopsy confirmed rectal adenocarcinoma. Further testing revealed liver and lung metastases. The patient responded well to holocranial radiotherapy, rarely presenting headache over the course of the disease.
Despite multiple reports of brain metastases as the initial manifestation of cancer, these mainly occur later in the course of the disease, with patients usually presenting metastasis in other organs before onset of the classical symptoms of OCS. This suggests that the entity is underdiagnosed.3 The literature includes 2 reports of OCS secondary to rectal cancer, but the cancer was already known in both cases.4 Ours is the first report of OCS as the initial manifestation of rectal adenocarcinoma. However, cerebellar metastasis is very common in colorectal cancer.5 Haematogenous spread is the mechanism most frequently underlying skull base metastases. In our patient, the internal vertebral venous plexus was the most likely pathway.6
MRI is the radiological technique of choice for diagnosing OCS,2 with CT studies being insufficient in most cases. Diagnosing this entity represents a challenge, as localisation of the lesion requires a comprehensive study of the skull base. Therefore, clinical suspicion assists radiologists in detecting OCS. Prognosis is poor and depends on the primary tumour and the extent of metastasis.
Treatment is primarily palliative. Pain rarely responds to conventional analgesia in these patients. Local radiotherapy relieves pain in most cases, and is more effective if treatment is started early.7
In conclusion, recognising OCS is crucial, as clinical suspicion facilitates radiological detection; confirmation of the diagnosis indicates advanced cancer. As early radiotherapy offers good relief of the signs and symptoms of OCS, diagnosis is important to preserving the patient’s quality of life.
Please cite this article as: Martín Asenjo M, Martín Guerra JM, Galvan Fernández J, Martín-Luquero Ibañez M, Prieto de Paula JM. Síndrome del cóndilo occipital como manifestación primera de una neoplasia de recto. Neurología. 2020;35:417–419.