To discover if there have been changes in the treatment time for SAH in our hospital environment.
Material and methodsComparative analysis of 571 patients treated at Hospital Universitari la Fe during 2 different time periods. The SAH-OLD group consisted of 462 patients attended consecutively between April 1997 and March 2005, while SAH-NEW comprised 109 patients attended consecutively between March 2007 and April 2010. We analysed demographic factors, risk factors, severity at time of admission, time to arteriography, diagnosis of aneurysm, use of surgical or endovascular treatment and time to treatment, frequency of neurological complications, in-hospital deaths, and modified Rankin Scale (mRS) at discharge.
ResultsMean time to arteriography was 2.18±2.5 days for the SAH-OLD group and 2.37±2.23 days, for the SAH-NEW group (P=.49). Mortality rates for SAH-OLD patients were calculated at 30%, compared to 18.3% in SAH-NEW patients (P=.01).
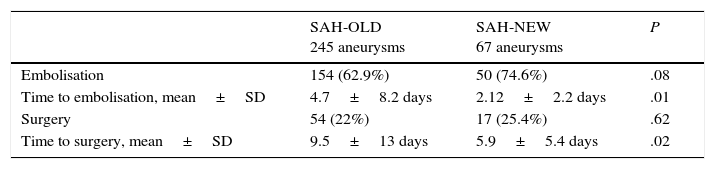
Among patients surviving the hospital stay in the SAH-OLD group, 13.3% had an mRS>3, compared to 21.3% of survivors in the SAH-NEW group (P=.06). Two hundred forty-five patients in the SAH-OLD group had cerebral aneurysms and 208 were treated (45% of the patient total). Sixty-five of the SAH-NEW patients received treatment (60% of the patient total, P=.007). In the SAH-OLD group, 62.9% of the patients underwent embolisation vs 74.6% in the SAH-NEW group (P=.08). Time to embolisation was 4.7±8.2 days for SAH-OLD patients and 2.12±2.2 days for SAH-NEW patients (P=.01). Twenty-two percent of SAH-OLD patients underwent surgery, compared to 25.4% in the SAH-NEW group (P=.62).
ConclusionsCare for SAH patients has improved in this hospital: results include fewer mortalities, a higher number of treatments with a smaller proportion of endovascular treatments, and shorter times to treatment. Elapsed time to arteriography remains stable.
Conocer, en nuestro medio, si ha habido variaciones en el tiempo en la atención a la HSA.
Material y métodosAnálisis de 571 pacientes con HSA tratados en el Hospital Universitario La Fe.
Comparación de 2 periodos: HSA-VIEJA: 462 pacientes consecutivos atendidos entre abril del 1997 y marzo del 2005; HSA-NUEVA: 109 pacientes consecutivos atendidos entre marzo del 2007 y abril del 2010. Se analizaron las características demográficas, los factores de riesgo, la gravedad al ingreso, los tiempos hasta la arteriografía, el diagnóstico de aneurisma, el tratamiento quirúrgico o intravascular y sus tiempos, frecuencia de complicaciones neurológicas, la mortalidad durante el ingreso y escala de Rankin modificada (mRS) al alta.
ResultadosMedia hasta la realización de la arteriografía: HSA-VIEJA: 2,18 ± 2,5 días, HSA-NUEVA: 2,37 ± 2,23 días, p = 0,49. Mortalidad: HSA-VIEJA 30% frente al 18,3% en HSA-NUEVA, p = 0,01. Entre los supervivientes al alta hospitalaria, un 13,3% en HSA-VIEJA tenía mRS > 3 frente a un 21,3% en HSA-NUEVA, p = 0,06. HSA-VIEJA: 245 pacientes tenían aneurisma cerebral, se trataron 208 (45% del total de los pacientes); HSA-NUEVA: reciben tratamiento 65 (60% del total de los pacientes), p = 0,007. HSA-VIEJA: se embolizaron 62,9%, HSA-NUEVA: 74,6%, p = 0,08. HSA-VIEJA: cirugía 22%, HSA-NUEVA: 25,4%, p = 0,62.
ConclusionesEn nuestro hospital ha mejorado la atención a la HSA: menor mortalidad, mayor número de tratamientos a expensas del tratamiento intravascular y menor tiempo hasta el tratamiento. El tiempo hasta la arteriografía ha permanecido estable.
Non-traumatic subarachnoid haemorrhage (SAH) accounts for 5% of all cases of stroke. Compared to other types of stroke, this severe condition affects younger patients, and it is associated with high mortality, severe disability, and a substantial economic and social burden.1 Treatment for SAH has evolved over the past few decades, mainly due to the introduction of endovascular treatment,2 but also thanks to the development of neurosurgical techniques3 and recent advances in neurocritical care.4
Hospital Universitario y Politécnico de La Fe, in Valencia, is a reference centre for the treatment of SAH. Our patients with SAH are managed according to the following protocol: after SAH diagnosis, patients are admitted to the intensive care unit (ICU) and undergo cerebral angiography as soon as possible. When aneurysms are detected, patients undergo embolisation immediately following diagnosis if the procedure is viable; when this is not the case, patients either undergo embolisation at a later time or receive surgical treatment, according to the neuroradiologist's and neurosurgeon's joint assessment. As a general rule, after discharge, patients receiving endovascular treatment are monitored by the neurology department whereas those undergoing surgery are monitored by the neurosurgery department.5
Treatment for cerebral aneurysms has undergone a paradigm shift: at present, endovascular treatment is the first-line option.6 The growing interest in improving SAH management shown by neurologists, neurosurgeons, and neuroradiologists alike has led to developing protocols for treating SAH and its associated complications.
We were able to analyse SAH treatment outcomes longitudinally in our setting given that we had access to data on SAH spanning over a decade.
ObjectiveOur purpose was to analyse any changes in SAH management over time in our setting.
Material and methodsA total of 571 patients with SAH treated at our hospital were included in our study. We compared 2 databases of consecutive patients (both created by our team) and covering 2 different periods. The first one is a retrospective database (SAH-OLD) including 462 patients with SAH receiving medical attention at our hospital between April 1997 and March 2005.5 The second is a prospective database (SAH-NEW) comprising 109 consecutive patients attended between March 2007 and April 2010.7
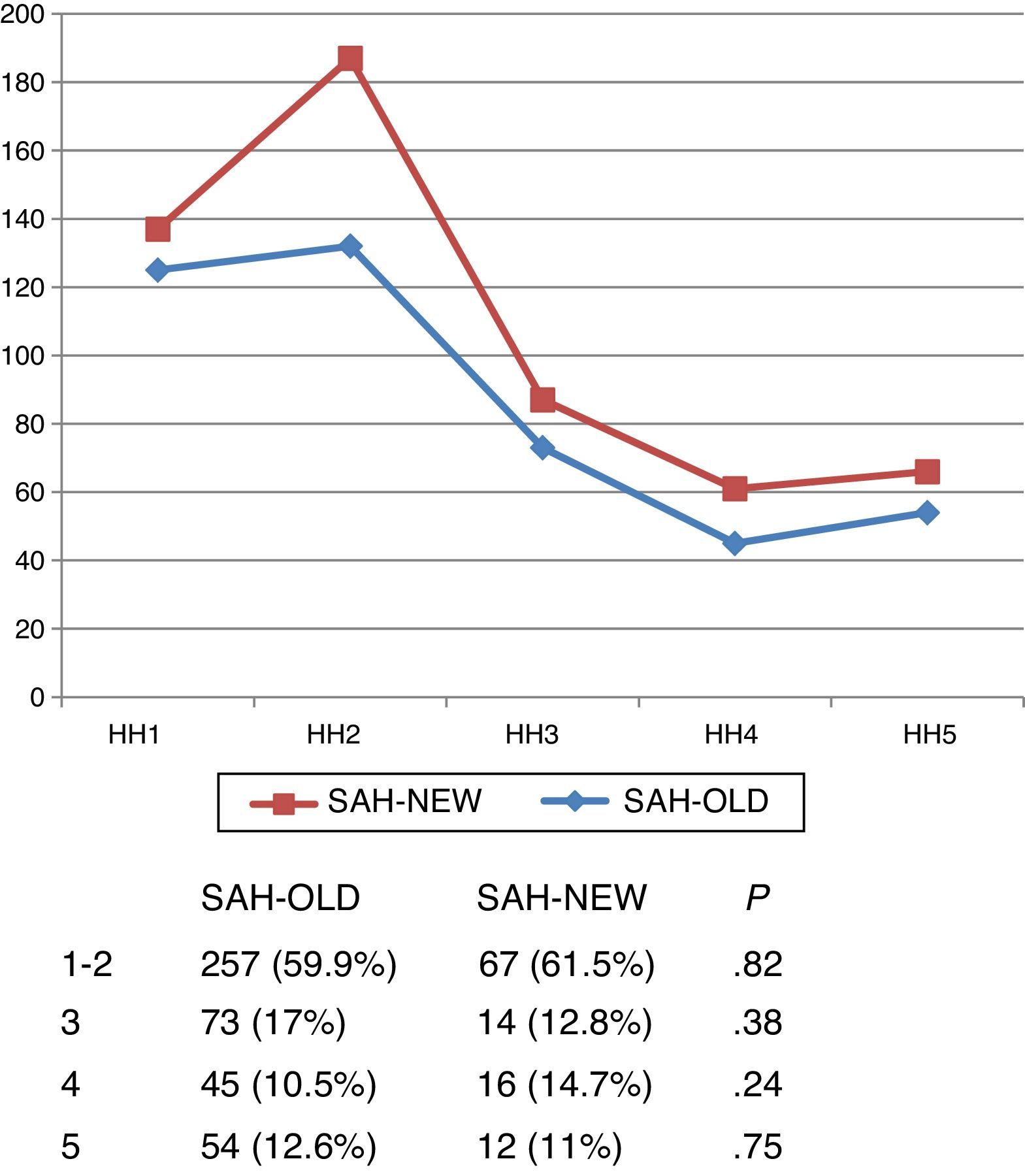
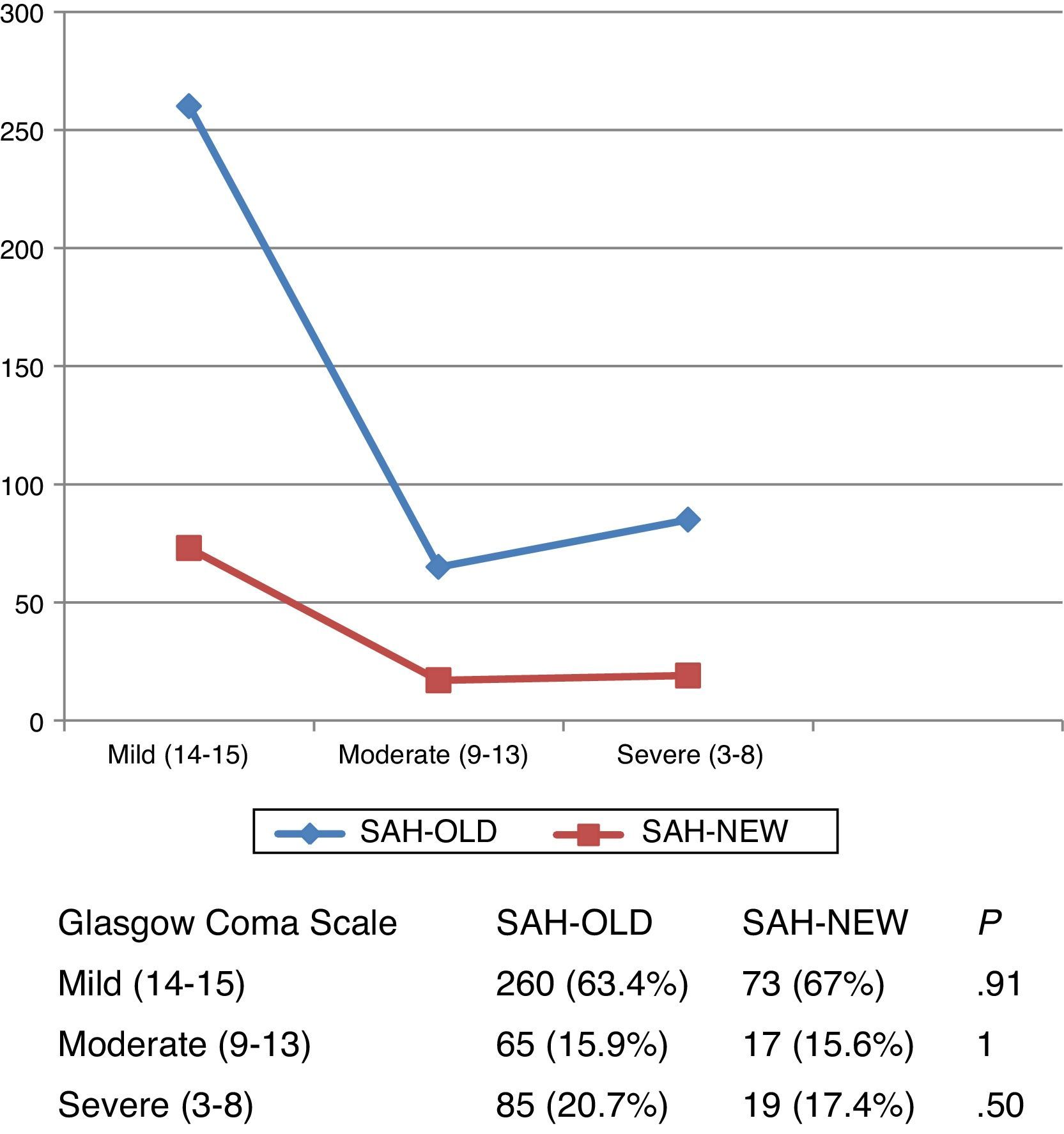
All patients had been admitted to the ICU according to our hospital's action protocol for SAH management and received treatment to prevent vasospasm in line with established practices in each period. Demographic characteristics (age, sex), risk factors, clinical status at admission (Hunt and Hess scale and Glasgow Coma Scale), time to angiography, diagnosis of aneurysm, surgical/endovascular treatment, and time to treatment were compared between the 2 groups.
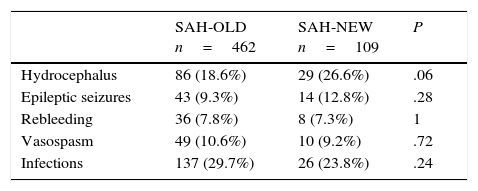
Likewise, we studied frequencies of the following neurological complications in both periods: epileptic seizures, rebleeding, hydrocephalus, and clinical vasospasm (defined as delayed neurological impairment associated with signs of vasospasm in a vascular study and/or signs of ischaemia in imaging studies). We also gathered data on presence of infections and compared mean hospitalisation times, in-hospital mortality, and modified Rankin Scale (mRS) scores at discharge.
Statistical analysisQualitative variables are expressed as relative frequencies and quantitative variables as means±SD. Qualitative variables were compared using the chi-square test; quantitative variables were compared using either the t test for independent samples or the Mann–Whitney U test for quantitative variables lacking a normal distribution (hospitalisation time). Values of P<.05 were considered statistically significant.
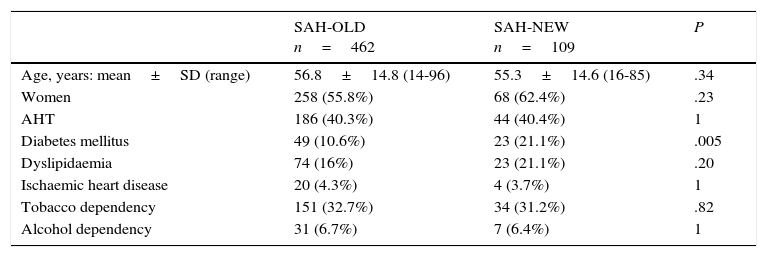
ResultsThe retrospective database included 462 cases of spontaneous SAH; 55.8% were women and mean age was 56.8±14.8 years (range, 14-96). The prospective database included 109 cases of SAH; 62.4% were women and mean age was 55.3±14.61 years (range, 16-85). Mean hospitalisation time was 20.53±19.83 days (range, 1-199) in SAH-OLD patients and 23.89±28.43 days (range, 1-245) in SAH-NEW patients (P=.15).
Demographic characteristics and risk factorsTable 1 shows demographic characteristics and risk factors of patients with SAH in both study periods. The only significant differences were in presence of diabetes mellitus, which was more prevalent among SAH-NEW patients (21.1% vs 10.6%; P=.005).
Demographic and risk factors.
| SAH-OLD n=462 | SAH-NEW n=109 | P | |
|---|---|---|---|
| Age, years: mean±SD (range) | 56.8±14.8 (14-96) | 55.3±14.6 (16-85) | .34 |
| Women | 258 (55.8%) | 68 (62.4%) | .23 |
| AHT | 186 (40.3%) | 44 (40.4%) | 1 |
| Diabetes mellitus | 49 (10.6%) | 23 (21.1%) | .005 |
| Dyslipidaemia | 74 (16%) | 23 (21.1%) | .20 |
| Ischaemic heart disease | 20 (4.3%) | 4 (3.7%) | 1 |
| Tobacco dependency | 151 (32.7%) | 34 (31.2%) | .82 |
| Alcohol dependency | 31 (6.7%) | 7 (6.4%) | 1 |
SD: standard deviation; AHT: arterial hypertension.
During the first period, 369 patients underwent a diagnostic cerebral angiography (80%) vs 97 patients (89%) in the second period (P=.02). Aneurysms were detected in 245 SAH-OLD patients (66.4%) and 67 SAH-NEW patients (69%) (P=.62).
Of the 369 SAH-OLD patients undergoing cerebral angiography, 57.2% displayed only one aneurysm, 9.2% had multiple aneurysms, and 2.7% displayed arteriovenous malformations. Studies yielded normal results in 30.9%. Cerebral angiography was not performed in this period in 20% of the patients, 80% of whom died prematurely. During the second period, 97 patients underwent cerebral angiography; 64% had only one aneurysm, 5.2% multiple aneurysms, and 3% had arteriovenous malformations. Results were normal in 24.8% of these patients.
In this subgroup, 11% did not undergo cerebral angiography and most of these patients (83%) died prematurely.
Mean time to angiography in the first period was 2.18±2.5 days (median, 1; mode, 1) and 2.37±2.23 days in the second (median, 2; mode, 1) (P=.49).
OutcomesRegarding outcomes, 139 patients (30.1%) died during the first period and 20 (18.3%) during the second period (P=.01). Among survivors, 13.3% of SAH-OLD patients scored over 3 on the mRS at discharge vs 21.3% of SAH-NEW patients (P=.06).
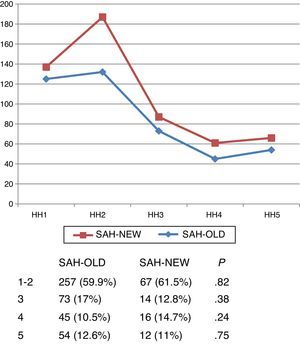
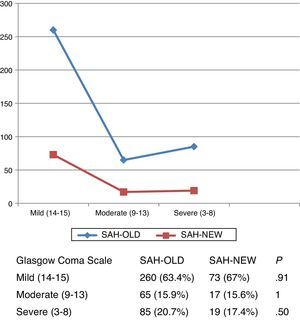
Severity at admissionSeverity at admission was similar in both subgroups according to Hunt and Hess scale scores (Fig. 1) and Glasgow Coma Scale scores (Fig. 2).
ComplicationsComplications in the 2 groups are summarised in Table 2. Although there were more cases of hydrocephalus among SAH-NEW patients, the difference was not statistically significant.
TreatmentOf the 245 SAH-OLD patients with cerebral aneurysms, 208 (45% of the patient total) received treatment. In the second period, 65 patients of the 109 with aneurysms (60% of the patient total) were treated (P=.007).
Table 3 summarises times to treatment, which were significantly shorter in the second period, for both embolisation and surgery.
DiscussionManagement of SAH has improved in our hospital: during the second period, the mortality rate was lower, a greater number of patients received treatment (increases were more marked for endovascular treatment), and times to treatment were shorter (for both embolisation and surgery). However, time to angiography has remained stable.
Both databases present comparable demographical data except for presence of diabetes (there were significantly more cases in the second period) and severity at SAH onset. Severity is an essential measure when comparing progression over time as it has the most bearing on prognosis.8,9
Guidelines for the management of SAH recommend early treatment of aneurysms to avoid rebleeding, the most severe complication of SAH.10,11 Emergency cerebral angiography is therefore essential to determine the most appropriate treatment (embolisation or surgery) as quickly as possible. Time to angiography is similar in both study periods, which suggests that the status of SAH as a medical emergency has not changed. Since January 2014, our hospital has had an on-call vascular surgeon who performs emergency angiography studies in cases of SAH, especially during the weekends. This measure will presumably reduce time to angiography in the future. In any case, time to treatment, whether embolisation or surgery, has also decreased significantly, which probably reflects good adherence to treatment protocols and guidelines for SAH management.
Endovascular treatment for cerebral aneurysm is on the rise, although surgeries are still performed. The publication of the International Subarachnoid Aneurysm Trial2 has resulted in a change in medical practice: at present, aneurysms are more frequently managed with endovascular treatment than with surgery.6,12 This pattern holds in our hospital: treatment for aneurysms increased significantly during both study periods, mainly due to expanded use of endovascular treatment.
While mortality rates in SAH are high compared to those of other types of stroke,13 they have decreased in the past few decades (17% between 1973 and 2002, according to a meta-analysis by Nieuwkamp et al.14). In our hospital, mortality decreased significantly during the study periods, and severity at SAH onset was similar in both periods. This decrease has been attributed to improvements in SAH management and increased use of endovascular treatment.15 Fewer patients in our series died during the acute phase, although disability was greater among SAH-NEW patients (differences approach statistical significance). If this is confirmed, we may be witnessing a change with a major healthcare, economic, and social impact. According to Lovelock et al.15, if fewer patients with SAH die during the acute phase and the survivors are left more severely disabled, the rehabilitation and hospitalisation burden will increase considerably.
In addition to such factors as age and severity at SAH onset, mortality is also believed to depend on complications.1 Both databases provide the number of complications per patient. No differences in the presence of complications were detected between the 2 periods except for hydrocephalus, which was more frequent among SAH-NEW patients (the difference was not significant). We therefore cannot attribute the decrease in mortality to a lower number of complications.
Another change observed during this time was the introduction of a protocol for multidisciplinary management of SAH patients. Treatment guidelines recommend admitting patients to the stroke unit or ICU11,16 in the most severe cases. Management of SAH in neurocritical care units, such as the one in our hospital, is widely accepted.17 Prognosis in patients attended in these units has improved in recent years18,19; our study provides a clear example. Management protocols are essential in these patients.17
One of the limitations of our study is that it is hospital-based rather than population-based. Furthermore, although the second database is prospective, the first is retrospective, which may affect data quality. In contrast, one of the strengths of our study is that it compares data from 2 different periods in the same population affected by a specific condition, SAH.15
ConclusionsAt our hospital, management of SAH has improved in the analysed period and time to angiography has remained stable over time.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Lago A, López-Cuevas R, Tembl JI, Fortea G, Górriz D, Aparici F, et al. Tendencias en el tratamiento de los aneurismas cerebrales: análisis de una serie hospitalaria. Neurología. 2017;32:371–376.