The COVID-19 pandemic has had an impact on ischaemic stroke management, with a reported decrease in hospital admissions, and even disruptions in healthcare and increased in-hospital mortality. However, there is a lack of evidence on the impact of the pandemic on functional prognosis. The aim of this study is to analyse the effect of the COVID-19 pandemic on the 3-month functional outcomes of patients hospitalised due to acute ischaemic stroke in Aragon (Spain).
MethodsWe reviewed the data of all patients admitted due to ischaemic stroke to any hospital in our regional healthcare system between 30 December 2019 and 3 May 2020. We compared modified Rankin Scale scores and mortality at 3 months in patients hospitalised before and after the declaration of a state of emergency due to the COVID-19 pandemic.
ResultsIn total, 318 patients with acute ischaemic stroke met our inclusion criteria. No differences were observed between periods in global or specific characteristics, with the exception of a higher proportion of patients older than 80 years during the first period (42.2% vs 29.0%, P = .028). In the comparative analysis, we found no significant differences in mortality (12.3 vs 7.9, P = .465) or in the proportion of patients with modified Rankin Scale scores ≤ 2 (57.7% vs 57.1%, P = .425) at 3 months.
ConclusionTo our knowledge, this is the first study to analyse the impact of COVID-19 pandemic on the 3-month functional outcomes of patients with ischaemic stroke. In our region, there has been no increase in rates of mortality or disability at 3 months in patients admitted due to ischaemic stroke during the pandemic.
La pandemia COVID-19 ha tenido un impacto en el manejo del ictus isquémico, se ha descrito una disminución de los ingresos hospitalarios e incluso una interrupción en la cadena de atención y aumento de la mortalidad intrahospitalaria. Sin embargo, falta evidencia sobre su impacto en el pronóstico funcional. El objetivo de este estudio es analizar el efecto de la pandemia COVID-19 en el pronóstico funcional a tres meses de los pacientes con ictus isquémico agudo hospitalizados en Aragón.
Material y métodosRevisamos los datos de todos los pacientes ingresados por ictus isquémico en todos los hospitales de nuestro sistema sanitario entre el 30 de diciembre de 2019 y el 3 de mayo de 2020. Comparamos su mRS y mortalidad a tres meses de los hospitalizados antes y después de haberse establecido el estado de emergencia secundario a la pandemia COVID-19.
ResultadosEn total, 318 pacientes con ictus isquémico agudo cumplieron nuestros criterios de inclusión. No hubo diferencias en las características globales y específicas de cada período, excepto por una mayor proporción de pacientes mayores de 80 años de edad durante el período pre-CoV (42,2% vs 29,0%, p = 0,028). En el análisis comparativo, no encontramos una diferencia significativa en la mortalidad (12,3 vs.7,9, p = 0,465) o la proporción de pacientes con mRS ≤2 (57,7% vs 57,1%, p = 0,425) a los tres meses.
ConclusiónHasta donde sabemos, este es el primer estudio que analiza el impacto de la pandemia de COVID-19 en el pronóstico funcional a tres meses de pacientes con ictus isquémico. En nuestra Comunidad Autónoma, no ha habido un incremento en la mortalidad o discapacidad a tres meses de pacientes hospitalizados por ictus isquémico durante el período COVID-19.
Since the first case of SARS-CoV-2 infection was reported in late 2019, COVID-19 has spread rapidly, collapsing healthcare systems across the globe.1–3 During the early months of the pandemic, controlling the outbreak became the main priority in most hospitals and healthcare centres, which had a negative impact on the management of patients with other diseases due to the overload of emergency services. Many studies have described a decrease in the number of hospital admissions due to ischaemic stroke,4–8 and even interruptions in stroke management protocols and an increase in stroke-related in-hospital mortality.5,9–12
Spain was one of the countries worst affected by the COVID-19 pandemic, and was under strict lockdown for 15 weeks: a state of alarm was in place from 14 March to 21 June 2020. We are now facing a second wave, with even higher numbers of infections (937 000 confirmed cases and 33 775 deaths as of 18 October 2020).13 While in early summer 2020, the focus seemed to be limited to regions with significant production of fruits and vegetables (Aragon and Catalonia), it later spread to other regions in Spain, resulting in one of the highest infection rates in Europe, according to data from the European Centre for Disease Prevention and Control.14 A “new reality” has emerged, which we all must accept; this raises the question of how the functional prognosis of ischaemic stroke has been affected.
This study aims to analyse the impact of the first wave of the COVID-19 pandemic on the 3-month functional prognosis of patients admitted to hospital with acute ischaemic stroke in the region of Aragon, Spain.
MethodsStudy design and populationWe included all consecutive patients admitted due to acute ischaemic stroke (with scores ≤ 2 on the modified Rankin Scale [mRS] before the event) to any hospital belonging to the Health Service of Aragon between 30 December 2019 and 4 May 2020.
Patients were classified into 2 groups, according to whether they were admitted before or after the state of alarm was declared in Spain (pre-CoV and CoV groups), and distributed by week. Week 11 (W11, 9-15 March) marks the beginning of the CoV period, since it was during that week that political decisions began to be made (limiting mobility and open-air events, closing schools) to contain the spread of the virus, with the state of alarm being declared on 14 March 2020.
We gathered the following demographic and clinical data: age, sex, cerebrovascular risk factors, baseline National Institutes of Health Stroke Scale (NIHSS) score, Alberta Stroke Program Early Computed Tomography Score (ASPECTS), type of code stroke activation, whether the patient had presented wake-up stroke or stroke with unknown time of symptom onset, stroke aetiology, onset-to-door time, door-to-needle time, door-to-puncture time, puncture-to-reperfusion time, whether mechanical thrombectomy achieved successful reperfusion (TICI grade 2b-3), type of anaesthesia during mechanical thrombectomy, and SARS-CoV-2 test results. The prognostic variables analysed were mortality and mRS score at 3 months.
Statistical analysisA descriptive statistical analysis was performed to compare both patient groups, in order to detect any differences in the study variables between the 2 periods. Qualitative variables are expressed as absolute frequencies and percentages, and continuous quantitative variables are expressed as mean and standard deviation (SD) or as median and quartiles 1 and 3 (Q1-Q3), as appropriate.
Comparisons between groups were performed with the chi-square test, for categorical variables, and the t test or the Mann-Whitney U test, for continuous variables. A multiple logistic regression analysis was performed to identify the factors associated with prognostic variables previously showing statistically significant differences between groups. Statistical significance was set at P < .05. Statistical analysis was performed with the SPSS Statistics software (IBM SPSS Statistics 21.0.0.0; New York, NY, USA).
The study was approved by the research ethics committee of the region of Aragon.
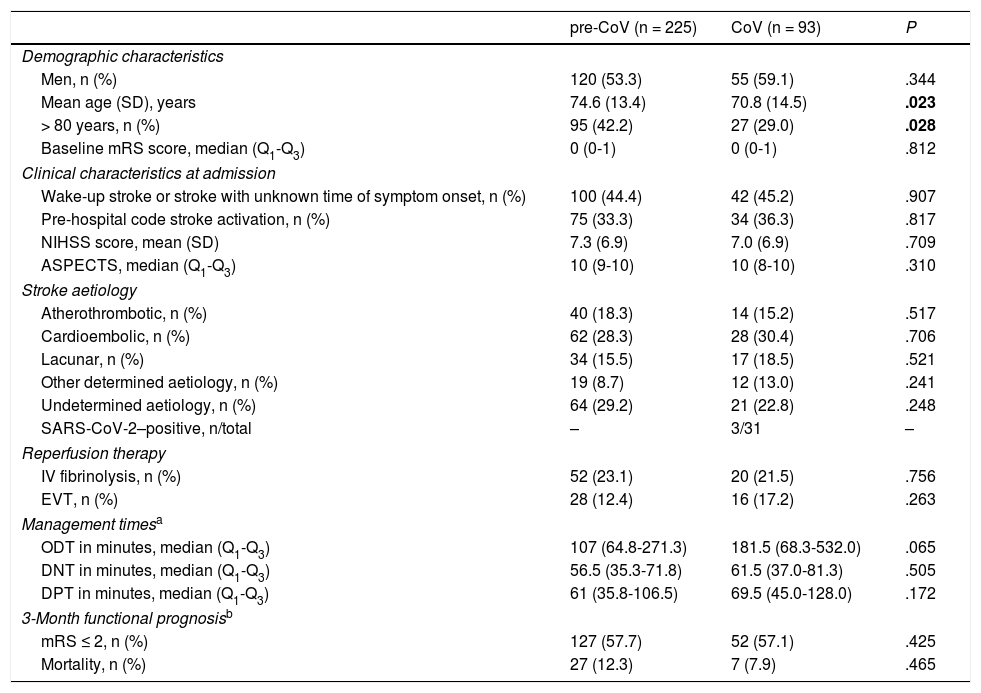
ResultsA total of 382 patients diagnosed with acute ischaemic stroke were admitted to hospitals in Aragon between 30 December 2019 and 4 May 2020 (225 during the pre-CoV period and 93 during the CoV period). Of these, 318 had a functional status of mRS ≤ 2 before the event. Men accounted for 55.0% (n = 175) of the sample; mean age (SD) was 73.5 years (13.8). We found no differences in global or specific characteristics between periods, except for age at presentation and the percentage of patients older than 80 years, which was higher in the pre-CoV group (42.0% vs 29.0%; P = .028). The age-adjusted comparative analysis found no significant differences in mortality (12.3% vs 8.9%; P = .465) or in the percentage of patients scoring ≤ 2 on the mRS at 3 months (57.7% vs 57.1%; P = .425) (Table 1). Cerebrovascular causes accounted for 66.7% of deaths. Cardioembolic ischaemic stroke was the stroke subtype associated with the highest mortality rate, accounting for 17.7%11 of deaths in the pre-CoV period and 21.4%6 deaths in the CoV period.
Characteristics of our sample of patients admitted to hospital due to acute ischaemic stroke and presenting a baseline modified Rankin Scale score ≤ 2 (N = 318). Patients were classified according to whether they were admitted before (pre-CoV) or after (CoV) declaration of the state of alarm in Spain.
| pre-CoV (n = 225) | CoV (n = 93) | P | |
|---|---|---|---|
| Demographic characteristics | |||
| Men, n (%) | 120 (53.3) | 55 (59.1) | .344 |
| Mean age (SD), years | 74.6 (13.4) | 70.8 (14.5) | .023 |
| > 80 years, n (%) | 95 (42.2) | 27 (29.0) | .028 |
| Baseline mRS score, median (Q1-Q3) | 0 (0-1) | 0 (0-1) | .812 |
| Clinical characteristics at admission | |||
| Wake-up stroke or stroke with unknown time of symptom onset, n (%) | 100 (44.4) | 42 (45.2) | .907 |
| Pre-hospital code stroke activation, n (%) | 75 (33.3) | 34 (36.3) | .817 |
| NIHSS score, mean (SD) | 7.3 (6.9) | 7.0 (6.9) | .709 |
| ASPECTS, median (Q1-Q3) | 10 (9-10) | 10 (8-10) | .310 |
| Stroke aetiology | |||
| Atherothrombotic, n (%) | 40 (18.3) | 14 (15.2) | .517 |
| Cardioembolic, n (%) | 62 (28.3) | 28 (30.4) | .706 |
| Lacunar, n (%) | 34 (15.5) | 17 (18.5) | .521 |
| Other determined aetiology, n (%) | 19 (8.7) | 12 (13.0) | .241 |
| Undetermined aetiology, n (%) | 64 (29.2) | 21 (22.8) | .248 |
| SARS-CoV-2–positive, n/total | – | 3/31 | – |
| Reperfusion therapy | |||
| IV fibrinolysis, n (%) | 52 (23.1) | 20 (21.5) | .756 |
| EVT, n (%) | 28 (12.4) | 16 (17.2) | .263 |
| Management timesa | |||
| ODT in minutes, median (Q1-Q3) | 107 (64.8-271.3) | 181.5 (68.3-532.0) | .065 |
| DNT in minutes, median (Q1-Q3) | 56.5 (35.3-71.8) | 61.5 (37.0-81.3) | .505 |
| DPT in minutes, median (Q1-Q3) | 61 (35.8-106.5) | 69.5 (45.0-128.0) | .172 |
| 3-Month functional prognosisb | |||
| mRS ≤ 2, n (%) | 127 (57.7) | 52 (57.1) | .425 |
| Mortality, n (%) | 27 (12.3) | 7 (7.9) | .465 |
SARS-CoV-2–positive: during the CoV period, 31 patients with acute ischaemic stroke were tested with SARS-CoV-2 polymerase chain reaction assays of nasopharyngeal exudates. Three of these tested positive.
ASPECTS: Alberta Stroke Program Early Computed Tomography Score; DNT: door-to-needle time; DPT: door-to-puncture time; EVT: endovascular treatment; IV: intravenous; mRS: modified Rankin Scale; NIHSS: National Institutes of Health Stroke Scale; ODT: onset-to-door time; SD: standard deviation.
Statistically significant values are shown in bold (P < .05).
The COVID-19 pandemic has had a considerable impact on the management of acute ischaemic stroke worldwide. Several studies have reported a decrease in the number of hospital admissions due to ischaemic stroke during the first wave of the pandemic.4–8 The pandemic also negatively affected pre-hospital management times, door-to-needle times, and in-hospital mortality during that period.5,9–12
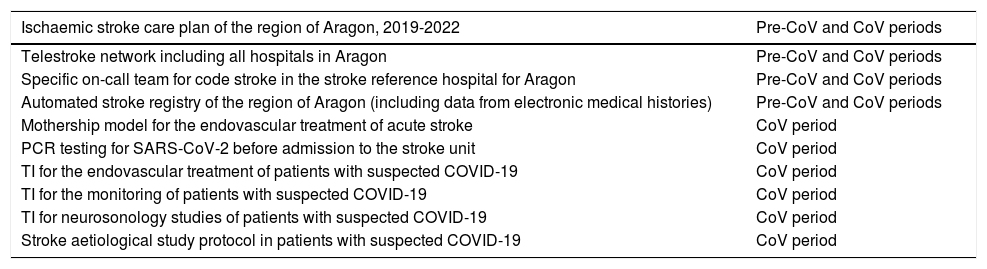
These findings raise the question of whether these changes have had a significant impact on these patients’ functional prognosis. Functional prognosis is typically assessed 3 months after stroke using the mRS. According to our results, the pandemic has had no impact on the functional prognosis of patients with stroke in Aragon, as no significant differences were found between patients admitted before and after declaration of the state of alarm. This may in part be explained by the response of the Health Service of Aragon to this new situation. Ischaemic stroke care in the region of Aragon is coordinated by the regional stroke care plan, which is based on a patient registry that is updated in real time using admission and discharge data from the electronic medical history database of the region of Aragon. This enables the region’s different hospitals and medical specialties to follow a coordinated, dynamic, and efficient approach to acute stroke management.4,15 During the first wave of the pandemic, all ordinary and extraordinary meetings of the regional stroke care working group were held by video conference, which allowed us to analyse data and implement several measures, including a neurosonology study protocol and shifting from a drip-and-ship model to a mothership model for the endovascular treatment of acute ischaemic stroke (Table 2). The patients attended during the CoV period were younger than in the pre-CoV period, but after adjusting for age, this was not found to be an explanatory variable.
Acute ischaemic stroke management strategies used during the study period in Aragon, Spain.
| Ischaemic stroke care plan of the region of Aragon, 2019-2022 | Pre-CoV and CoV periods |
|---|---|
| Telestroke network including all hospitals in Aragon | Pre-CoV and CoV periods |
| Specific on-call team for code stroke in the stroke reference hospital for Aragon | Pre-CoV and CoV periods |
| Automated stroke registry of the region of Aragon (including data from electronic medical histories) | Pre-CoV and CoV periods |
| Mothership model for the endovascular treatment of acute stroke | CoV period |
| PCR testing for SARS-CoV-2 before admission to the stroke unit | CoV period |
| TI for the endovascular treatment of patients with suspected COVID-19 | CoV period |
| TI for the monitoring of patients with suspected COVID-19 | CoV period |
| TI for neurosonology studies of patients with suspected COVID-19 | CoV period |
| Stroke aetiological study protocol in patients with suspected COVID-19 | CoV period |
PCR: polymerase chain reaction; TI: technical instructions.
However, we should be mindful that these findings refer to hospitalised patients only: our sample did not include patients with ischaemic stroke who did not seek medical attention,4,5 who may therefore not be receiving preventive treatment or not be under follow-up.
Despite these findings, we should be alert to any changes in hospital management of ischaemic stroke during the pandemic. Lower rates of admission to stroke units, premature discharges, and reduced access to early rehabilitation therapy have been observed in this period.16 The need for a comprehensive aetiological study in these patients should not be overlooked. Although it seems not to have been the case in our series, an increase in the percentage of patients with stroke of undetermined aetiology due to incomplete aetiological studies may have negative consequences, such as an increase in stroke recurrence rates in the short term due to a failure to implement specific preventive measures.
Well-designed protocols and coordination between all healthcare professionals involved in ischaemic stroke management, not only in the acute phase but also during hospitalisation and follow-up, are essential for providing optimal care to these patients. Furthermore, coordination between all hospitals in the region may help to solve this and other problems that may arise.
Given the multiple outbreaks of COVID-19 being reported across Europe, it may be necessary to design long-term strategies aimed at ensuring adequate medical care in this new reality, rather than regarding the pandemic as a transient situation. In this context, there is a need to raise public awareness of the importance of seeking emergency medical attention when needed, and to promote digital communication and coordination strategies. Telestroke, teleconsultations, and telerehabilitation may be considered in this context. Some scientific societies have already issued consensus documents for the implementation of telemedicine consultations; these guidelines may also be applied to the management of neurological patients.17
The main limitation of this study is its retrospective, observational design. Furthermore, given the small number of patients from our sample who presented COVID-19, we are unable to assess the effect of SARS-CoV-2 infection on the functional prognosis of ischaemic stroke. Our results cannot be generalised to other regions or countries, given the peculiarities of our acute ischaemic stroke care model, the geographical characteristics of our region, and differences in healthcare resources used during the pandemic.
ConclusionThis is the first study into the impact of the COVID-19 pandemic on 3-month functional prognosis of patients with acute ischaemic stroke in the region of Aragon. Previous studies have described the negative effects of the pandemic on the management of acute stroke. However, our study, including hospitalised patients from throughout the region, did not find an increase in mortality or disability at 3 months.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Tejada Meza H, Lambea Gil Á, Villar Yus C, Pérez Lázaro C, Navarro Pérez MP, Campello Morer I, et al., Pronóstico funcional a 3 meses de pacientes hospitalizados por ictus isquémico agudo en Aragón: análisis regional de la repercusión de la COVID-19. Neurología. 2021;36:531–536.