Cerebral Autosomal Dominant Arteriopathy with Subcortical Infarctions and Leukoencephalopathy (CADASIL) is a hereditary cerebral cerebrovascular disease in young adults that is clinically manifested by migraine, cognitive impairment, psychiatric symptoms and progressively severe neurological deficits, caused by subcortical ischemic infarcts.1,2
It is believed that the first description was probably Van Bogaert, reported as progressive subcortical encephalopathy of the Binswanger type with rapid evolution.3 In 1977, Sourander and Walinder, described in eight members of the same family, the clinical, genetic and morphological characteristics of a previously unrecognized type of multiple heart attack dementia that affected young adults of both sexes.4,5 Ten years later, Sonninen and Savontaus, reported a family in which 16 members had multipart dementia beginning in adulthood associated with cerebrovascular infarctions in white matter.6 The disorder was characterized by recurrent strokes with neuropsychiatric symptoms, affecting young adults of both sexes and transmitted in an autosomal dominant pattern. This may be the same disorder known as familial subcortical dementia with arteriopathic leukoencephalopathy by Davous and Fallet-Bianco in 1991.7
CADASIL is an autosomal dominant disease resulting from mutations of the gene encoding the transmembrane receptor Notch 3, located on chromosome 19, and genetic testing is the gold standard for diagnosis.8,9 In the last decade, more than 80 Notch 3 mutations were identified in more than 400 families with CADASIL. All mutations responsible for CADASIL lead to an odd number of cysteine residues.
We present a patient carrying the new mutation variant c.1565G>C of the NOTCH-3 gene, which has not yet been recorded in the Human Gene Mutation Database (HGMD) for that gene and therefore described as a new one.
We present a 56-year-old woman, secretary, with eleven years of schooling, who has a 15-day headache, with twitches of bilateral temporal location, without vomiting, without aura, without photo or phonophobia. No history of smoking or alcohol use. Under treatment for hypertension and dyslipidemia.
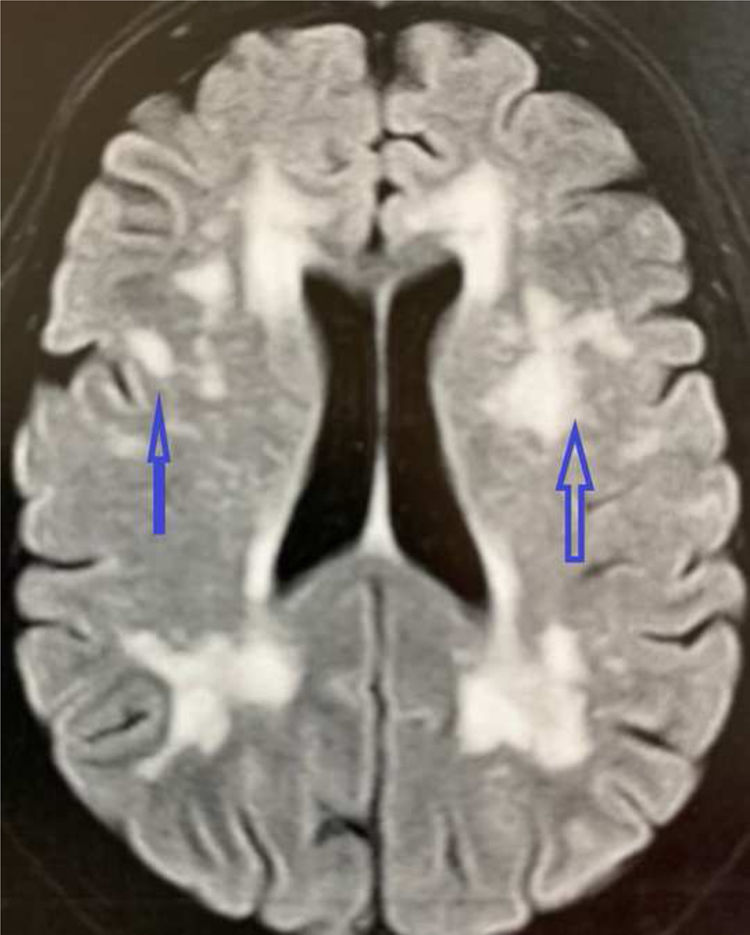
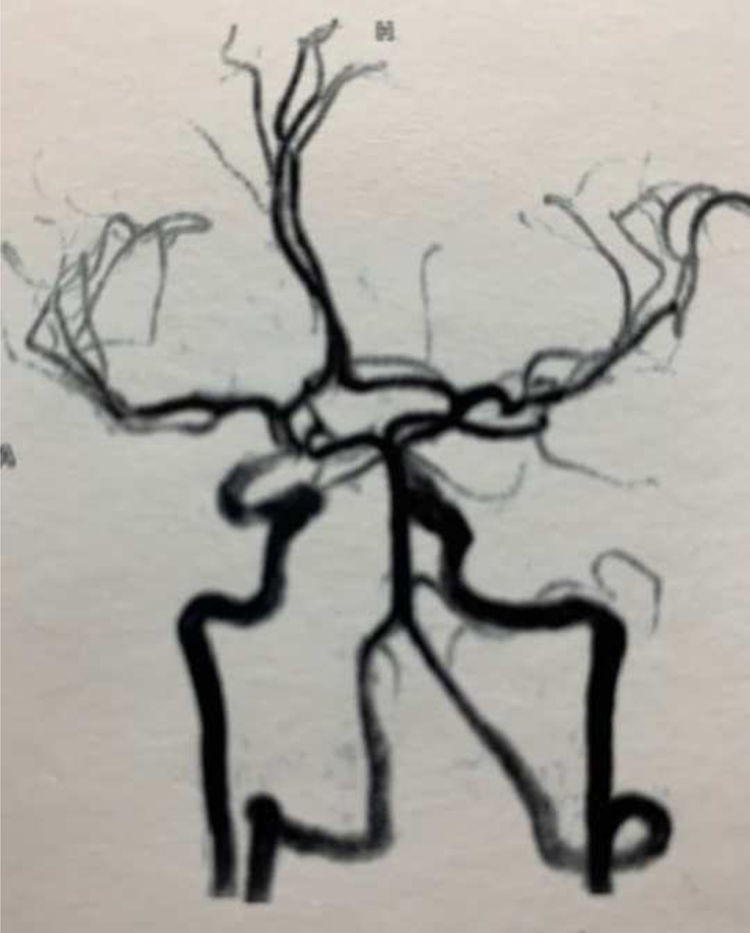
A carotid and vertebral Doppler ultrasonography demonstrated a normal spectrum of blood flow. Brain MRI showed nonspecific lesions in the white matter of the cerebral hemispheres, with subcortical involvement in the pole of the left temporal lobe, probably related to microangiopathy, Fazekas index grade 3 (Fig. 1). Normal brain MRI-angiography (Fig. 2).
MRI legend: Multiple nodular images, some confluent, with hypersignal in the FLAIR and T2, without restriction in the diffusion of water, observed in the periventricular white substance, semioval centers and radiated crowns, in the external capsule bilaterally, in the insula lobes and in the anterior portions of the temporal lobes associated with multiple small old infarctions observed in the radiated heart of the right frontal lobe, in the knee and trunk of the corpus callosum and in the white pericalosal substance bilaterally.
Neuropsychological assessment revealed cognitive impairment (23 points on the MMSE scale, having regard to age, education, a reduced auditory, and visual immediate memory span, impaired working memory and lower verbal fluency).
Taking into consideration the clinical data, the patient was suspected to suffer from CADASIL. The deletion/duplication analysis of the Notch 3 gene followed by complete gene sequencing showed the variant c.1565G>C (p.Cys522Ser) in heterozygosis.
CADASIL is now recognized as the most common cause of hereditary stroke and vascular cognitive impairment in adults. The pathophysiological mechanisms are being studied. The great variability in the clinical presentation and the nonspecific pattern of MRI lesions, at least in the early stages, make the clinical diagnosis difficult. This disease is underestimated by the diagnostic screening of all 33 exons and NOTCH3 flanking regions using PCR amplification and direct Sanger sequencing in patients with suspected CADASIL.10
Considered as a prototype of vascular dementia related to subcortical microangiopathy, it also results in additional psychiatric disorders, particularly mood changes, usually in association with the development of cognitive impairment.
The disease manifests itself in adulthood with signs of brain impairment caused by the progressive development of disseminated white matter lesions in association with subcortical lacunar infarctions. As the total lesion volume increases and cerebral atrophy develops, the frequency and severity of motor difficulties and cognitive dysfunction also increase. The cognitive disorder is progressive and CADASIL is the most common form of hereditary vascular dementia.
With the genetic diagnostic resources available today (complete exome and the genome) we can now sequence families and identify pre-symptomatic individuals with the disease.11
Environmental factors appear to play an important role in clinical development and disease severity, as family studies affected with CADASIL demonstrate different disease courses in individuals with the same mutation, including monozygotic twins. We need more evidence, but in a retrospective study of the Chinese population, characteristics that CADASIL is a genotypic and phenotypic heterogeneity.12
Our CADASIL patient carry mutation p.Cys522Ser in heterozygosis of the NOTCH-3 gene, which has not yet been recorded in the HGMD for that gene and therefore described as a new one.
We consider it important to report new information about CADASIL patients, as new mutations and pathogenic phenomena are being considered, described and made possible a better understanding of the disease.
Conflict of interestThere is no conflict of interest to declare.